|
 |
- Search
Abstract
Purpose
The aim of our study is to determine the alterations on coronal balance after overcorrection of Lenke type 1 curve, retrospectively.
Methods
Datas of 34 patients (29 female, 5 male patients; mean age, 16.3±3.3 years; range, 13-24 years) surgically treated for scoliosis between 2004 and 2010 were reviewed, retrospectively. The adolescent idiopathic scoliosis patients with Lenke type 1 curve treated with only posterior pedicle screw and postoperative thoracic curves less than 10° by Cobb method on frontal plane were enrolled in this study. Mean follow-up period was 52.5±29.7 months.
Results
The mean amount of the preoperative thoracic curves was measured as 41.2°±6.1° (range, 30°-56°). The mean amount of the early postoperative thoracic curves was measured as 6.5°±1.8° (range, 3°-9°). The mean amount of the thoracic curves was measured as 8.5°±4.6° (range, 3°-22°) during the last follow-up (p=0.01). The mean preoperative coronal balance was measured as 8.5mm(range, 1-30mm). The mean early postoperative coronal balance was measured as 3.5mm(range, 0-36 mm). The mean coronal balance was measured as 5.5mm(range, 0-38mm) during the last follow-up (p>0.05).
Conclusion
We suggest that Lenke type 1B and 1C should be carefully evaluated and the fusion levels should be accurately selected in order to maintain the correction of coronal balance. We suggest that selective fusion with overcorrection in Lenke type 1A are applied to curves that can be corrected lumbar curve at the preoperative bending radiograph and curves that not have coronal decompensation and >10° distal junctional kyphosis, preoperatively.
Performing selective fusion in scoliosis surgery gained popularity through the possibility of obtaining more correction by the help of new developed surgical techniques. Ideally, the lowest instrumented vertebra should be as proximal as possible to preserve lumbar motion, but it should be distal enough to avoid trunk imbalance. The level of the lowest instrumented vertebra and the amount of sufficient correction are still controversial8,14,17,20). It is also uncertain if coronal imbalance may develop in a spinal column, totally corrected with a short segment fusion.
The aim of this study is to evaluate the effect of overcorrection on coronal balance in the patients with Lenke type 1 adolescent idiopathic scoliosis (AIS) in whom selective fusion was performed.
Thirty-four patients (29 female, 5 male patients; mean age, 16.3 years; range, 13-19 years) who were operated due to AIS via selective fusion and posterior instrumentation between the years 2004 and 2010 were retrospectively evaluated. In all of the patients, the curves were classified as Lenke type 1. Postoperatively, the deformity was measured to be under 10 degrees in all patients. The patients with congenital, neuromuscular, infantile, juvenile and adult idiopathic scoliosis, and the patients in whom intramedullary pathologies were detected in magnetic resonance imaging were not included in the study.
Anterior-posterior (AP), lateral, right, and left bending radiographies of the whole spinal column were obtained preoperatively. In AP radiographies, the apical, the stabile, the proximal and the distal end vertebrae were defined. The amount of thoracic and lumbar curves were measured by Cobb method. The flexibility of the curves were measured in bending radiographies. Kyphosis angle was measured in lateral radiographies using Cobb method, by measuring the angle between the lines parallel to the upper endplate of T5 and the lower enplate of T12 vertebra. Lordosis angle was measured in lateral radiographies using Cobb method, by measuring the angle between the lines parallel to the upper endplate of L1 and the upper endplate of S1 vertebra. All measurements were performed by the same author using a computer software (Surgimap 1.1.2, Nemaris Inc., New York, NY, USA). The curves were classified according to Lenke classification10) (Figs. 1, 2, 3).
The apical vertebra translation was measured in milimeters, by measuring the distance between the midpoint of the apical thoracic vertebra and the plumb line drawn from the midpoint of C7 vertebra10). Coronal balance was measured in the coronal plane, by measuring the distance between the central sacral line and the plumb line drawn from the midpoint of C7 vertebra. When the values were measured to be greater than 2 centimeters, the result was described as coronal imbalance, as defined by Scoliosis Research Society (SRS)21). We evaluated the coronal decompensation that coronal imbalance with a greater than 20-mm shift to the left of the C7 plumbline due to spontaneous progression of the unfused lumbar curve after selective thoracic fusion at the follow-up period.
Selective fusion was performed in the cases which fulfilled the criteria described by Lenke et al.9). Distal fusion level was selected according to the neutral or the stabile vertebra levels. This variety is because of the preference of the different surgeons performing the operations.
All of the patients were operated in hypotensive general anesthesia and prone position. The chest and iliac crests are fixed firmly with a silicone bolster and sponge pads. The selected fusion levels were defined under fluoroscopy and the incision line was marked. A longitudinal midline incision was used. Paraspinal muscles were subperiosteally dissected. Third generation instrumentation systems were used in all cases. The system elements consisted of polyaxial titanium screws, hooks, rods, and cross-links. Following the insertion of the pedicle screw and the fluoroscopic control, 2 rods were adapted into the system in appropriate sagittal curvature. Distraction applied in the concave side and compression was applied in the convex side. Apical derotation was performed. Thus, global correction was obtained. Cross-links contributed the rigid fixation. The spinous processes of the vertebrae were resected and after decortication, were used as autograft. Wake-up test was performed in all cases.
Radiographies of the whole spinal column were obtained in the second postoperative day and the parameters were measured. The radiological process was repeated during the last control.
The data were analyzed using SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). For the comparison of; preoperative-postoperative-follow-up thoracic and lumbar curve magnitudes, kyphosis, lordosis and other parameters Pillai's Trace test was used via general linear models in repeated measures method. Bonferroni test was used for dual comparisons. Values of p<0.05 were accepted as being statistically significant.
The mean follow-up period was 52.5±29.7 months. Risser sign was 5 in 50% of the cases (17), 4 in 35.3%(12), 3 in 14.7%(5). According to lumbar modifiers, 15 patients (44.1%) were classified as Lenke type 1A, 14 patients (41.2%) were classified as Lenke type 1B and 5 patients (14.7%) were classified as Lenke type 1C.
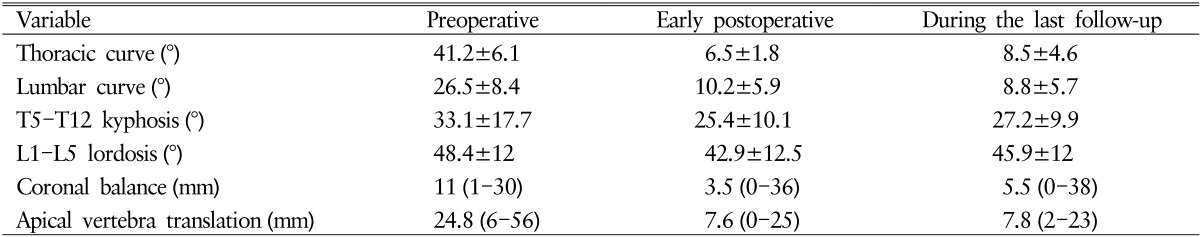
The mean amount of the preoperative thoracic curves was measured as 41.2°±6.1° (range, 30°-56°). The mean amount of the early postoperative thoracic curves was measured as 6.5°±1.8° (range, 3°-9°). The mean amount of the thoracic curves was measured as 8.5°±4.6° (range, 3°-22°) during the last follow up (p=0.01) (Table 1).
The mean amount of the preoperative lumbar curves was measured as 26.5°±8.4° (range, 8°-47°). The mean amount of the early postoperative lumbar curves was measured as 10.2°±5.9° (range, 2°-26°). The mean amount of the lumbar curves was measured as 8.8°±5.7° (range, 1°-24°) during the last follow-up (p=0,01) (Table 1).
The mean preoperative T5-T12 kyphosis was measured as 33.1°±17.7° (range, 3°-65°) The mean early postoperative T5-T12 kyphosis was measured as 25.4°±10.1° (range, 5°-40°). The mean T5-T12 kyphosis was measured as 27.2°±9.9° (range, 13°-42°) the last follow-up (p>0.05) (Table 1).
The mean preoperative L1-L5 lordosis was measured as 48.4°±12° (range, 24°-77°). The mean early postoperative L1-L5 lordosis was measured as 42.9°±12.5° (range, 25°-66°). The mean L1-L5 lordosis was measured as 45.9°±12° (range, 30°-64°) the last follow-up (p>0.05) (Table 1).
The mean preoperative coronal balance was measured as 8.5mm(range, 1-30mm). The mean early postoperative coronal balance was measured as 3.5mm (range, 0-36 mm). The mean coronal balance was measured as 5.5mm (range, 0-38 mm) during the last follow-up (p>0.05) (Table 1).
The mean preoperative apical vertebra translation was measured as 24.8mm(range, 6-56 mm). The mean early postoperative apical vertebra translation was measured as 7.6mm (range, 0-25mm). The mean apical vertebra translation was measured as 7.8mm(range, 2-23mm) during the last follow-up (p=0.01) (Table 1).
The fusion ended at the level of the stabile vertebra in 11 cases (32.4%), whereas it ended over the level of the stabile vertebra in 12 cases (35.3%).
The mean Cobb angle of bending lumbar curve in 29 of 34 patients was measured as 5° (range, 0°-9°); and the others was measured as 15° (12°-18°). Decompensation was seen in cases of over 10°. The complications consisted of distal junctional kyphosis in 2 cases (5.9%) and coronal decompensation in 5 cases (14.7%).
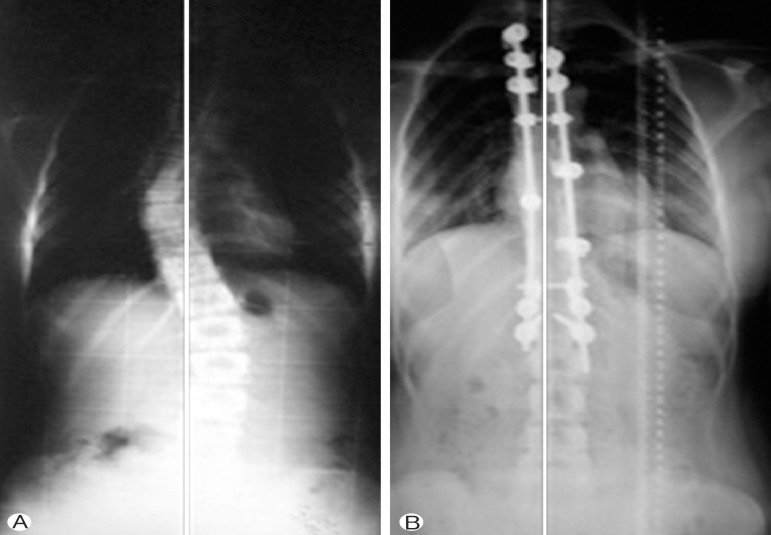
Our study showed that over correcting the 3 Lenke type 1B and 2 Lenke type 1C pateints led to decompensation. However, all of them did not complained any clincial symptoms during the follow-up. Therefore no intervention to correct the decompensation followed. Already, 2 (1 Lenke type 1B and 1 Lenke type 1C patients) of the 5 patients with postoperative decompensation had coronal imbalance preoperatively. These patients had coronal imbalance 26 and 30mm, respectively. Two Lenke type 1B and one Lenke type 1C patients showed postoperative decompensation at the most recent follow-up. Left and right side-bending radiographs in 5 patients partially was improved. These patients had minimum >30° (31°, 36°, 40°, 40°, 47°) lumbar curve and less flexibility (mean, 18°; range, 16°-23°).
Two patients had distal junctional kyphosis in follow-up period. One patient did not complained any symptoms, so no intervention took place. This patient had Lenke type 1B(N) and 15° local kyphosis between T10-L2. The second case underwent surgery. This patient had Lenke type 1B(+) and 19° local kyphosis between T10-L2. Fusion level was extended to L4 from T12.
The main aim of the scoliosis surgery is to correct the deformity, to increase pulmonary functions and to improve cosmesis. The amount of sufficient correction and the correct instrumentation levels are still controversial. With the help of the developing surgical techniques, the available correction of frontal plane deformities improved from 40% to 65%, in the last 5 decades21).
still controversial. Some authors evaluate the coronal balance by taking the position of the cranium over pelvis into account, whereas some uses the position of the thorax for this purpose1,5,10,13,15). SRS describes the coronal balance as the distance between the C7 plumb line and the vertical line passing through the midpoint of the S1 upper endplate10). When the distance is greater than 2 centimeters it is described as coronal imbalance. The position of the thorax may be evaluated with 2 methods, the measurement of lateral trunk shift or the apical vertebra translation. In their study, Richards et al.17) have evaluated the relation among lateral trunk shift, thoracic apical vertebra translation, and the coronal balance. They have reported that the sum of coronal balance and the apical vertebra translation is related with lateral trunk shift. However, they claimed that these parameters are not related in the patients with a coronal balance equal to or less than 1.0. Thus, coronal balance does not reflect the position of thorax on pelvis. In the literature coronal balance is also known as trunk shift. This is confusing and misleading for the determination of the correct terminology17). In our study, our evaluation for coronal balance was based on the description by SRS and we have considered it as imbalance when coronal balance was equal to or greater than 2.0.
Spontaneous correction of the lumbar curve which is not included in the selective fusion has started to be reported in the 50's6), however there is still not an exact consensus on the optimal amount of correction, the best instrumentation technique and the sufficient length of the fusion. In their study including 127 cases, Luk et al.11) has performed 4 different posterior instrumentation techniques and they have compared the preoperative bending radiographies and postoperative radiographies. They have reported that the correction rate is not only related with the surgeon and the surgical technique, but it is also related with the structure and the rigidity of the deformity.
In their review written in 2007, Winter et al.21) claimed that correction more than the major curve's flexibility is overcorrection and that it will lead problems in the compensatory curves. They suggested that, the surgeon may perform overcorrection when the compensatory curve is flexible and it corrects totally in bending radiographies. They also reported that the flexibility of the upper left thoracic curves than that of the right thoracic curves and shoulder imbalance is more common after the surgical overcorrection in right thoracic curves. In the study, the mean early postoperative coronal balance was decreased. The last follow-up coronal imbalance for 5 patients was occurred, but preoperative coronal imbalance in there patients already was available. Left and right side-bending radiographs in 5 patients with decompensation partially was improved in our study. We suggest that the flexibility of the curve should be carefully evaluated and the fusion levels should be accurately selected in order to maintain the correction of coronal balance. Two patients had preoperative decompensation. The decompensation in these patients continued after surgery. Our clinic had not analyzed appropriate preoperative evaluation and management of these patients. Absolutely, we should be careful about the flexibility of curves and preoperative coronal imbalance before deciding certain treatment.
Limiting the correction of the deformity and the selection of the lowest instrumented vertebra are commonly debated2,9,16,19). Takahashi et al.18) claimed that the main factors influencing coronal balance are the flexibility of the lumbar curve, lowest instrumented vertebra, the amount of correction in the thoracic curve, the modifier type of the lumbar curve and the correction of the lumbar curve in the preoperative bending radiographies. Burton et al.3) recommended the distal fusion level to be 2 vertebrae below the stabile vertebra, but on the contrary McCance et al.12) claimed that the fusion level ending below the stabile vertebra emerged as a risk factor for coronal imbalance. Takahashi et al.18) created 3 groups according to the stabile or end vertebrae and compared the groups in terms of the self correction rates of the lumbar curve and coronal balance. They have reported that coronal balance was present in the deformities with end vertebra below the stabile vertebra, but they have found the coronal balance maintained in all groups at the end of the 2 years of follow-up and that the lumbar curve was self corrected. They have found that to stop the fusion level below the stabile vertebra provided better self correction in the lumbar curve and better coronal balance in the deformities with stabile vertebra below the end vertebra. Because of the low number of the cases with end vertebra below the stabile vertebra, they could not conclude about the optimal level for the lowest instrumented vertebra.
Self correction of the lumbar curve and coronal balance do not only depend on the distal fusion level but also depend on many other factors such as the the correction mechanism, the correction strategy and the deformity pattern18). In our study, the distal fusion level was at the level of the stabile vertebra in 11 cases (32.4%), below the level of the stabile vertebra in 11 cases (32.4%) and over the level of the stabile vertebra in 12 cases (35.3%). We have found out that distal level of the fusion and the coronal balance during the last follow-up are not significantly related. This relation should be analyzed in larger case groups for a better evaluation. Distal junctional kyphosis occurred in 2 patients during follow-up period. These patients had T10-L2 kyphosis before surgery. If we prefered minor kyphotic curve, we could not encounter with the distal junctional kyphosis.
Some studies have shown that over correcting the thoracic curve can lead to decompensation9,16). There is not a concensus on the optimal amount of correction necessary. Imrie et al.7) has described a correction more than 80% as an overcorrection. They compared overcorrected cases with the cases in which a correction less than 40% was performed. They reported that they have achieved more lumbar correction by risking the coronal balance and have obtained better clinical results, but they have encountered sagittal imbalance in these cases. They observed that hypokyphosis has occurred. They claimed that there has been a low rate of coronal imbalance with overcorrection in Lenke types 1A and 1B deformities, but there has been more risk with the overcorrection of Lenke type 1C deformities.
In their study in a large case group with Lenke type 1C deformities, Wang et al.20) found out that the correction rate is not an independent factor on coronal balance. They also reported that there has been less coronal imbalance in the cases with a ratio of thoracolumbar curve angle/lumbar curve angle equal to or greater that 1.2 and in which the distal fusion level was at or below the level of the end vertebra.
In their series with 199 cases, Dobbs et al.4) observed coronal imbalance in 5 cases. In 4 of those, the lumbar modifier was type C and in 1 of them the lumbar modifier was type B. These cases were also the ones in which an overcorrection was performed and the thoracic curve was corrected under 10°. In our study, 3 Lenke type 1B and 2 Lenke type 1C patients led to decompensation. The number of the cases with a Lenke type C deformity was low. Thus an evaluation was not possible regarding coronal balance in this cases. However, we believe that these cases tended more to postoperative coronal imbalance and it is not possible to predict the late follow-up results in the preoperative period. If we predicted the correct identification fusion levels in Lenke types 1B and 1C, we could not encounter with the decompensation during follow-up period. We should be carreful such conditions in Lenke type 1 cases, while performing overcorrection.
Limitations of our study had retrospective nature of the study, including limited number of patients, no control group for alternative surgical procedures.
We suggest that the flexibility of the curve should be carefully evaluated and the fusion levels should be accurately selected in order to maintain the correction of coronal balance. Overcorrection for preoperative coronal imbalance with cases may lead to truncal shift in compensatory curves. Especially, Lenke type 1C patients have preoperative impaired coronal balance values, they tend to have postoperative coronal imbalance and late term outcomes can not be predicted before surgery. We suggest that Lenke types 1B and 1C should be carefully evaluated and the fusion levels should be accurately selected in order to maintain the correction of coronal balance. We suggest that selective fusion with overcorrection in Lenke type 1A are applied to curves that can be corrected lumbar curve at the preoperative bending radiograph and curves that not have coronal decompensation and >10° distal junctional kyphosis, preoperatively. We may perform the posterior fusion by doing undercorrection to avoid decompensation in Lenke types 1B and 1C.
NOTES
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
1. Bassett GS, Bunnell WP. Effect of a thoracolumbosacral orthosis on lateral trunk shift in idiopathic scoliosis. J Pediatr Orthop 1986 6:182-185. PMID: 3958173.


2. Bridwell KH, McAllister JW, Betz RR, Huss G, Clancy M, Schoenecker PL. Coronal decompensation produced by Cotrel-Dubousset "derotation" maneuver for idiopathic right thoracic scoliosis. Spine (Phila Pa 1976) 1991 16:769-777. PMID: 1925753.


3. Burton DC, Asher MA, Lai SM. The selection of fusion levels using torsional correction techniques in the surgical treatment of idiopathic scoliosis. Spine (Phila Pa 1976) 1999 24:1728-1739. PMID: 10472108.


4. Dobbs MB, Lenke LG, Walton T, Peelle M, Della Rocca G, Steger-May K, et al. Can we predict the ultimate lumbar curve in adolescent idiopathic scoliosis patients undergoing a selective fusion with undercorrection of the thoracic curve? Spine (Phila Pa 1976) 2004 29:277-285. PMID: 14752350.


5. Floman Y, Penny JN, Micheli LJ, Riseborough EJ, Hall JE. Osteotomy of the fusion mass in scoliosis. J Bone Joint Surg Am 1982 64:1307-1316. PMID: 7142238.


6. Freeman BL. Scoliosisand Kyphosis. In: Canale ST editors. Campbell's Operative Orthopaedics. ed 10. Vol 2. Philadelphia: Mosby; 2003. p.1751-1837.
7. Imrie M, Yaszay B, Bastrom TP, Wenger DR, Newton PO. Adolescent idiopathic scoliosis: should 100% correction be the goal? J Pediatr Orthop 2011 31(1 Suppl):S9-S13. PMID: 21173626.


8. Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001 83-A:1169-1181. PMID: 11507125.

9. Lenke LG, Bridwell KH, Baldus C, Blanke K. Preventing decompensation in King type II curves treated with Cotrel-Dubousset instrumentation. Strict guidelines for selective thoracic fusion. Spine (Phila Pa 1976) 1992 17(8 Suppl):S274-S281. PMID: 1523512.


10. Lenke LG, Edwards CC 2nd, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976) 2003 28:S199-S207. PMID: 14560193.


11. Luk KD, Lu DS, Cheung KM, Wong YW. A prospective comparison of the coronal deformity correction in thoracic scoliosis using four different instrumentations and the fulcrum-bending radiograph. Spine (Phila Pa 1976) 2004 29:560-563. PMID: 15129073.


12. McCance SE, Denis F, Lonstein JE, Winter RB. Coronal and sagittal balance in surgically treated adolescent idiopathic scoliosis with the King II curve pattern. A review of 67 consecutive cases having selective thoracic arthrodesis. Spine (Phila Pa 1976) 1998 23:2063-2073. PMID: 9794050.


13. Moe JH. A critical analysis of methods of fusion for scoliosis; an evaluation in two hundred and sixty-six patients. J Bone Joint Surg Am 1958 40-A:529-554. PMID: 13539082.


14. Newton PO, Upasani VV, Bastrom TP, Marks MC. The deformity-flexibility quotient predicts both patient satisfaction and surgeon preference in the treatment of Lenke 1B or 1C curves for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2009 34:1032-1039. PMID: 19363458.


15. Ouellet JA, Johnston CE 2nd. Effect of grafting technique on the maintenance of coronal and sagittal correction in anterior treatment of scoliosis. Spine (Phila Pa 1976) 2002 27:2129-2135. PMID: 12394926.


16. Richards BS. Lumbar curve response in type II idiopathic scoliosis after posterior instrumentation of the thoracic curve. Spine (Phila Pa 1976) 1992 17(8 Suppl):S282-S286. PMID: 1523513.


17. Richards BS, Scaduto A, Vanderhave K, Browne R. Assessment of trunk balance in thoracic scoliosis. Spine (Phila Pa 1976) 2005 30:1621-1626. PMID: 16025031.


18. Takahashi J, Newton PO, Ugrinow VL, Bastrom TP. Selective thoracic fusion in adolescent idiopathic scoliosis: factors influencing the selection of the optimal lowest instrumented vertebra. Spine (Phila Pa 1976) 2011 36:1131-1141. PMID: 21343851.


19. Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. Decompensation after Cotrel-Dubousset instrumentation of idiopathic scoliosis. Spine (Phila Pa 1976) 1990 15:927-931. PMID: 2259983.


20. Wang Y, Bünger CE, Wu C, Zhang Y, Hansen ES. Postoperative trunk shift in Lenke 1C scoliosis: what causes it? How can it be prevented? Spine (Phila Pa 1976) 2012 37:1676-1682. PMID: 22460921.


21. Winter RB, Lonstein JE, Denis F. How much correction is enough? Spine (Phila Pa 1976) 2007 32:2641-2643. PMID: 18007238.


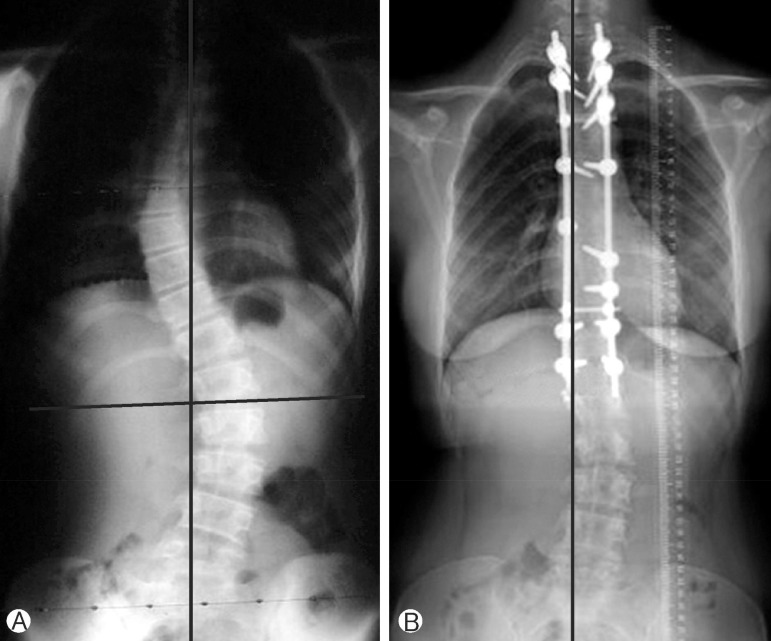
Fig. 1
Eighteen-year-old girl patient with Lenke type 1A curve. (A) Preoperative anterior-posterior graphy, (B) the latest follow-up anterior-posterior graphy.
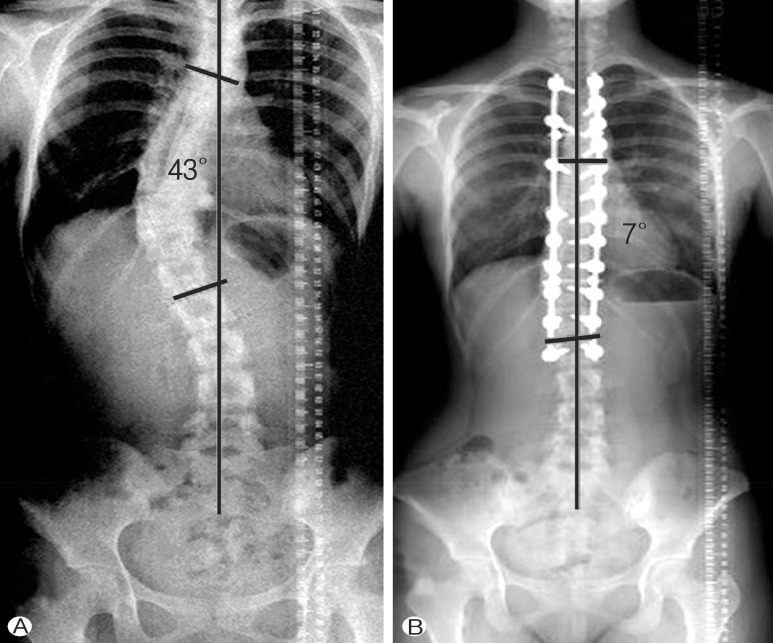
Fig. 2
Fourteen-year-old girl patient with Lenke type 1B curve. (A) Preoperative anterior-posterior graphy, (B) the latest follow-up anterior-posterior graphy.

- TOOLS
-
METRICS

-
- 7 Crossref
- Scopus
- 7,176 View
- 109 Download
- Related articles in NS
-
Journal Impact Factor 3.2