|
 |
- Search
| Neurospine > Volume 18(3); 2021 > Article |
|
|
Abstract
Objective
Adult cervical deformity (ACD) is a debilitating spinal condition that causes significant pain, neurologic dysfunction, and functional impairment. Surgery is often performed to correct cervical alignment, but the optimal amount of correction required to improve patient-reported outcomes (PROs) are not yet well-defined.
Methods
A review of the literature was performed and Fisher z-transformation (Zr) was used to pool the correlation coefficients between alignment parameters and PROs. The strength of correlation was defined according to the following: poor (0 <r Ōēż 0.3), fair (0.3 < r Ōēż 0.5), moderate (0.5 < r Ōēż 0.8), and strong (0.8 < r Ōēż1).
Results
Increased C2ŌĆō7 sagittal vertical axis was fairly associated with increased Neck Disability Index (NDI) (pooled Zr=0.31; 95% confidence interval [CI], -0.03 to 0.58). Changes in T1 slope minus cervical lordosis poorly correlated with NDI (pooled Zr=-0.04; 95% CI, -0.23 to 0.30). Increased C7ŌĆōS1 was poorly associated with worse EuroQoL 5-Dimension (pooled Zr=-0.22; 95% CI, -0.36 to -0.06). Correction of horizontal gaze did not correlate with legacy metrics. Modified Japanese Orthopedic Association correlated with C2-slope, C7ŌĆōS1, and C2ŌĆōS1.
Conclusion
Spinal alignment parameters variably correlated with improved health-related quality of life and myelopathy after corrective surgery for ACD. Further studies evaluating legacy PROs, Patient-Reported Outcomes Measurement System, and ACD specific instruments are needed for further validation.
Adult cervical spine deformity (ACD) can negatively impact the quality of life of patients by causing pain, myelopathy, radiculopathy, sensorimotor deficits, as well as inability to maintain horizontal gaze [1]. The severity of kyphosis and cervical deformity may also affect the global sagittal alignment and negatively impact overall posture, gait, and ambulation as cervical deformity may overwhelm compensation mechanisms to maintain normal physiologic function. The highly heterogeneous clinical and radiographic presentations of ACD have led to its designation as a distinct clinical entity within spinal disorders, culminating in development of the Ames-International Spine Study Group (ISSG) Cervical Spine Deformity classification system that incorporates anatomical, radiographic, and clinical characteristics, thereby providing a systematic approach for classifying ACD (Table 1) [2]. This classification seeks to further optimize the treatment of ACD with respect to clinical evaluation, radiographic analysis, operative planning, and outcomes assessment. A study by the ISSG demonstrated a substantial health impact of symptomatic ACD of different deformity types in a prospective cohort evaluating various health-related quality of life (HRQoL) measures [3].
Moving toward a patient centered-treatment approach, surgical goals for ACD typically include correction of the deformity, restoration of horizontal gaze and posture, decompression of the neural elements, and alleviation of pain. Given the wide range of techniques utilized to address cervical deformity, such as multilevel anterior approaches, combined anterior and posterior approaches, and various osteotomy techniques including posterior 3-column osteotomies, studying the impact of the invasiveness of surgery and potential complications on patient outcomes is critical to not only guide surgical strategy but to also determine how much correction is needed to provide benefit from the patientsŌĆÖ perspective. Achieving radiographic correction is certainly feasible now with improvements in surgical implant technology, intraoperative imaging, and technical innovations. However, assessing patient-reported outcomes (PROs) and HRQoL measures are necessary to understand the full impact of deformity and correction on patientsŌĆÖ health and daily functioning. As such, considerable efforts have been made by special study groups including but not limited to the International Spine Study Group (ISSG) and other study groups in North America, Europe, and Asia [4-6].
Many HRQoL and PRO instruments have been used to assess general health, pain, disability, and function for cervical spine disorders. These include but are not limited to the EuroQoL 5-Dimension (EQ-5D), the modified Japanese Orthopedic Association (mJOA) score, the Oswestry Disability Index, Neck Disability Index (NDI), and the Patient-Reported Outcomes Measurement System (PROMIS) [7]. A number of PRO instruments are used in practice and there is variability in adoption and implementation. Various PROs study-specific parameters such as pain, function, depression, and anxiety, among others. The Scoliosis Research Society-22r questionnaire (SRS-22r), developed to assess PROs in adult spinal deformity, was designed to play an important role in personalized treatment of spinal deformity by addressing specific symptoms and expectations of patients seeking treatment for correction of the deformity [8-10]. Moreover, prediction models for SRS-22r were designed to accurately predict a probability of achieving the patientŌĆÖs goal from surgery, exploring a new horizon where the patient goals play a central role in the decision to undergo correction for a spinal deformity [8]. Along these lines, a greater understanding of PROs would help overcome the challenges associated with the existing heterogeneity and difficult interpretation and transportability of the collected data.
Considering the variability in adoption, utilization, and implementation of such outcome measures for adult cervical deformity (ACD), we reviewed the current literature to determine associations between corrections in spinal alignment and PROs and their significance. Understanding the association and relevance of such outcomes assessments may help surgeons implement such metrics in their clinical practice.
Following the Cochrane methodology, a literature review was performed to identify studies involving patients diagnosed and treated for ACD and reporting PROs [11]. Our search was completed on OVID encompassing the MEDLINE, and Embase databases to identify English articles published from inception to July 2020. We used the search terms ŌĆ£cervical deformity,ŌĆØ ŌĆ£patient-reported outcomes,ŌĆØ ŌĆ£quality of life,ŌĆØ ŌĆ£treatment outcomesŌĆØ other PRO-associated terms ŌĆ£pain,ŌĆØ ŌĆ£depression,ŌĆØ ŌĆ£activity,ŌĆØ and commonly used PRO instruments in spine surgery ŌĆ£EQ-5D,ŌĆØ ŌĆ£Neck Pain NRS,ŌĆØ ŌĆ£NDI,ŌĆØ ŌĆ£mJOA,ŌĆØ ŌĆ£VAS,ŌĆØ ŌĆ£SF12,ŌĆØ ŌĆ£SF36,ŌĆØ ŌĆ£PROMIS.ŌĆØ In addition to electronic databases search, the references of selected studies were searched. Literature reviews and conference abstracts were excluded (Supplementary method 1).
Two authors (EM and JS) independently screened titles and abstracts of all search results to identify potential articles for full-text review. All screening steps were done on Covidence, a web-based platform for managing and streamlining systematic reviews [12]. Information from eligible articles, including senior authorŌĆÖs name and year of publication, study group, study design (observational, interventional), study setting (single institutional vs. multi-institutional), sample size, definition of ACD, PROs, timepoints of PROs assessment, and specification of how PROs were used in the each study (i.e., outcome, main predictor, covariable, descriptor, or other) were extracted. Our primary goal was to identify the role of PROs in guiding the treatment of ACD at baseline, in the perioperative setting, and after treatment. Given that none of the retrieved studies was a randomized controlled trial, the quality of the included studies was assessed using the Newcastle-Ottawa Quality Assessment Form for Cohort Studies, which is recommended by Cochrane for evaluation of nonrandomized cohort studies [13] (Supplementary Table 1). Each study was evaluated independently by 2 authors (EM and JS) based on selection of study groups, comparability of study groups, and outcomes assessment.
We used descriptive statistics to summarize the characteristics of the included studies. Correlation coefficients (r) were reported and the strength of the correlation was defined according to the following: poor (0<rŌēż0.3), fair (0.3<rŌēż0.5), moderate (0.5<rŌēż0.8), and strong correlation (0.8<rŌēż1). Results of regression analyses, Žć2 tests for categorical variables, and unpaired t-tests for continuous variables were also reported if present. Owing to the heterogeneity of the data available, we performed a meta-analysis only when 3 or more independent correlation coefficients were available. Correlation coefficients between cervical deformity parameters and PROs were converted into Fisher z-scores (Zr) to be used in the meta-analyses. Z-scores were pooled to obtain overall effect sizes as the inverse variance weighted average of an independent study z-score. The degree of heterogeneity of the pooled effect size was assessed by the Žć2 test and the inconsistency index (I2). If I2<50% and p>0.1, the fixed-effect model was assumed because of the homogeneous effects of parameters. With I2Ōēź50% and pŌēż0.1, the random-effect model was selected due to heterogeneous effects. All statistical analyses were conducted using ŌĆśmetaŌĆÖ and ŌĆśmetaphorŌĆÖ packages in the R ver. 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria). The threshold for statistical significance was ╬▒=0.05. All tests were 2-sided.
We identified 19 studies that studied a correlation between cervical parameters and PROs used to assess pain, disability, and quality of life in ACD surgery (Fig. 1). Across the 19 studies, 10 studies were conducted by the ISSG representing 19 sites in the United States (US), 2 sites in Japan, and 1 site in Canada [3,14-21]. The remaining studies were conducted in single institutions in the US [4,22-24], Lebanon [25], China [25], Japan [26], and South Korea [27,28]. The characteristics of each study are summarized in Supplementary Table 2. In the following analysis, we examine the association of radiographic parameters with PROs, with specific interest in identifying the association between the deformity modifiers in the Ames cervical deformity classification system and PROs (Fig. 2).
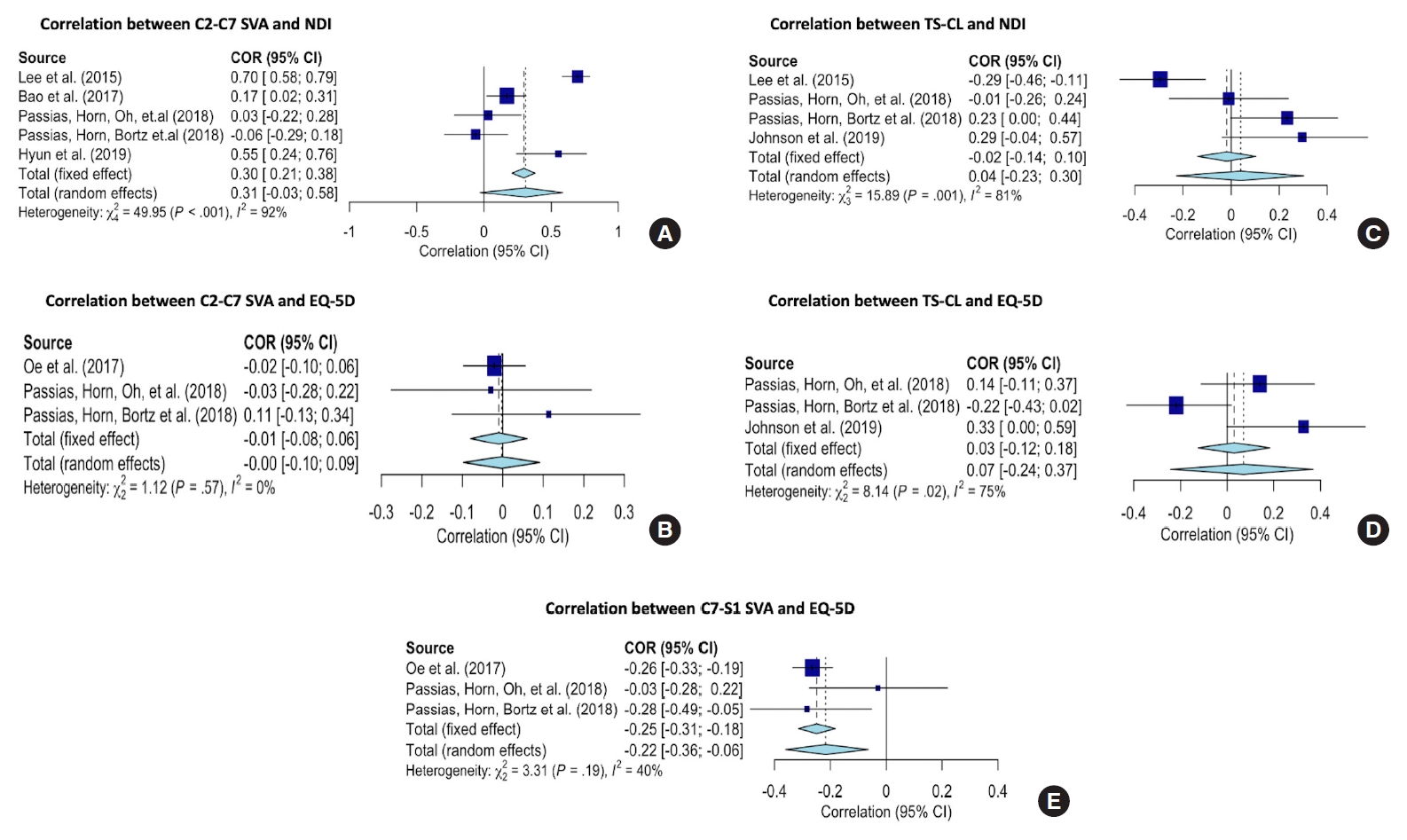
Cervical C2ŌĆō7 sagittal vertical axis (C2ŌĆō7 SVA) was investigated in 9 of the included studies [4,16,19,21,24,26-29], including 3 studies by the ISSG [16,19,30]. Meta-analyses of correlation coefficients showed that C2ŌĆō7 SVA and NDI correlated fairly (random effect; Zr=0.31 [95% CI, -0.03 to 0.58]; p<0.001) [16,24,27,28,31]. C2ŌĆō7 SVA correlated poorly with EQ-5D (fixed effect; Zr=-0.01 [95% CI, -0.0 to 0.06]; p=0.57) (Fig. 3) [16,26,31]. Lee et al. [27] found that an increase in C2ŌĆō7 SVA significantly predicted more pain and disability measured by visual analogue scale (VAS), NDI, and Neck Pain and Disability Scale in multiple regression. Moreover, the ISSG highlighted a significant improvement in Numerical Rating Scale (NRS)-neck and EQ-5D in patients who showed improvement of C2ŌĆō7 SVA 3 months after surgery [32]. Using a composite outcome of NDI, mJOA, and NRS-neck, Virk et al. [18] found that a good outcome following surgery for cervicothoracic deformity was associated with better postoperative C2ŌĆō7 CVA. Only one study investigated the relationship between C2ŌĆō7 SVA categories in CD Ames-ISSG severity groups (score 0, C2ŌĆō7 SVA< 4 cm; score 1, C2ŌĆō7 SVA 4ŌĆō8 cm; score 2, C2ŌĆō7 SVA> 8 cm), and PROMIS domains showing no difference in PROMIS scores between C2ŌĆō7 SVA categories [4]. The authors used conditional tree analysis to determine thresholds for PROMIS domains that were independent of C2ŌĆō7 SVA severities, but did not reach statistical significance [4].
Eight studies investigated the relationship between T1 slope minus cervical lordosis (TSŌĆōCL) and PROs [4,16,19,22,24,25,27,28]. Meta-analyses of correlation coefficients showed that NDI and EQ-5D correlated poorly with TSŌĆōCL (NDI random effect; Zr=0.04 [95% CI, -0.23 to 0.30]; p=0.001] and EQ-5D random effect; r=0.07 [95% CI, -0.24 to 0.37]; p=0.02) (Fig. 3). Of these 8 studies, 2 studies looked at PROMIS domains (physical function, pain intensity, pain interference) and found a weak to fair correlation with TSŌĆōCL (Fig. 2) [4,22]. Bao et al. [24] demonstrated no difference in average TSŌĆōCL between symptomatic (defined by NDI > 15, VAS neck > 3, or VAS arm > 3) and asymptomatic (defined by NDI Ōēż 15, VAS neck Ōēż 3, and VAS arm Ōēż 3) ACD. In parallel, Passias et al. [32] found that TSŌĆōCL modifier grade improvement (score 0, TSŌĆōCL < 15┬░; score 1, TSŌĆōCL 15┬░ŌĆō20┬░; Score 2, TSŌĆōCL > 20┬░; Table 1) at 3 months after surgery showed significant amelioration of both NRS-back and -neck scores. Similarly, Horn et al. [19] found that 1-year postoperative poor outcome (defined as failing to meet minimal clinically important difference [MCID] for NDI, or modified mJOA Ames modifier score 0ŌĆō11) were associated with a higher mean TSŌĆōCL than those who did not have a poor 1-year postoperative outcome. Bakouny et al. [25] found similar 36-item Short Form Health Survey scores across TSŌĆōCL Ames modifier grades (Table 1 for reference) at baseline. Fair (r=0.327 [22]) and weak (r=0.14 [31]; r=-0.218 [16]) correlations between TSŌĆōCL and EQ-5D were reported in 3 studies indicating that there was a low likelihood that a change TSŌĆōCL was associated with a strong change in EQ-5D [22,31,32].
The correlation of chin-brow vertical angle (CBVA) with PROs was examined in 2 studies [24,25]. Neither of these studies identified that a change in CBVA modifiers (grade 0: CBVA 1┬░ŌĆō10┬░; grade 1: CBVA -10┬░ŌĆō0┬░ or 11┬░ŌĆō25┬░; grade 3: CBVA < -10┬░ or > 25┬░; Table 1) was associated with a strong change in PROs. Furthermore, no correlation of CBVA with NDI, VAS, and EQ-5D was identified [24]. One of 2 studies [16,24] examining the association of McGregor slope with PROs, showed that 1-year postoperative McGregor slope was significantly correlated with NDI. Johnson et al. [22] found C1ŌĆō2 lordosis did not correlate significantly with any PROMIS domain or legacy metric. However, Zhong et al. [29] reported a significant correlation between the change in C1ŌĆō2 lordosis after surgery and JOA (r=-0.060), NDI (r=0.676), and SF-12 (r=-0.592). Protopsaltis et al. [21] showed that higher C2-slope, which correlated with upper cervical and subaxial parameters including TSŌĆōCL, C0ŌĆō2 angle, cSVA, and CL, was correlated with worse NDI, mJOA, NRS for neck pain, and EQ-5D in cervicothoracic deformities.
Horn et al. [19] reported 24% of patients still had severe disability (mJOA score < 12) after correction surgery, and that poor clinical outcomes were associated with baseline global SVA > 4 cm (odds ratio [OR], 3.2; 95% CI, 0.9ŌĆō10.3), baseline C2ŌĆōT3 SVA > 5.4 cm (OR, 1.01; 95% CI, 0.9ŌĆō1.1), and baseline pelvic tilt (PT) > 20┬░ (OR, 0.92; 95% CI, 0.85ŌĆō0.98). Passias et al. reported only 29 of 63 patients (46%) had improved mJOA, and only 12 of 63 (19%) reached MCID in mJOA 1 year after surgery. However, both mJOA mean improvement and mJOA MCID were not significantly correlated with neither cSVA, TSŌĆōCL, CBVA, SVA, PT, nor PIŌĆōLL [31]. In another study, the same study group found that corrected C2ŌĆōS1 SVA (r=-0.424, p=0.002) and C7ŌĆōS1 SVA (r=-0.434, p<0.001) at 1 year were the only radiographic parameters significantly correlated to 1-year mJOA score [16]. Ailon et al. [14] examined patients with moderate and severe myelopathy (mJOA<15) showing a slight improvement in mJOA (11.8┬▒1.9 to 12.2┬▒2.6 (p=0.43) after surgery without reaching statistical significance. Studying the importance of C2 slope as a marker of cervical deformity, Protopsaltis et al. showed that C2 slope and mJOA were correlated (r=-0.65, p=0.02) [21]. An assessment of depression in ACD showed that mJOA scores were found similar between patients who were depressed and those who were not depressed at all timepoints, including baseline and postoperative outcomes followed to 1 year [15].
In parallel, the effect of global and pelvic parameters on PROs was commonly examined in ACD [16,19,24,26,30,33]. Oe et al. [26] demonstrated a negative but weak correlation between EQ-5D and PT (r=-0.216, p<0.001), pelvic incidence minus lumbar lordosis (PIŌłÆLL; r=ŌłÆ0.206, p=0.001), C7 SVA (r=-0.265 and p=0.001), and C2 SVA (r=-0.262, p=0.001) in ACD. Subanalysis revealed that these correlations were observed more in women than men. Horn et al. [19] did not record a difference in average PT, PIŌłÆLL, and T4ŌłÆ12 kyphosis between those who had a poor 1-year postoperative outcome (failing to reach MCID for NDI, and having severe symptoms measured by mJOA 0ŌłÆ11) and those without a poor 1-year postoperative outcome. Passias et al. [16] demonstrated a significant correlation between C2ŌłÆS1 SVA and C7ŌłÆS1 SVA, and 1-year mJOA, EQ-5D, and NDI. Also, Virk et al. [18] found that improvements in NDI, mJOA, and NRS-neck were associated with better global spine alignment at 1 year after surgery. In another study comparing baseline to 3-month postoperative HRQoL, significant changes in any disability parameters occurred in patients that deteriorated in PT grade (NRS-neck) and PIŌłÆLL grade (NDI score) surgery [32]. Meta-analyses of correlation coefficients showed that C7-SVA and NDI were poorly correlated (random effect; r=-0.22 [95% CI, -0.36 to -0.06]; p=0.19) (Fig. 3).
A wide variety of PRO instruments are available and used in contemporary spine surgery practices. These consist of legacy instruments such as NDI and mJOA and newer instruments such as PROMIS. The ideal PRO measuring tool is a scale that adapts to a patientŌĆÖs responses in order to generate the most personalized questionnaire. Development of computerized adaptive testing (CAT) can offer a dynamic system that can generate specific questions based on a patientŌĆÖs prior answers to provide the most reliable and complete assessment [34,35]. In 2004, the National Institutes of Health created the Patient-Reported Outcomes Measurement Information System (PROMIS) to improve the reporting of patient-driven responses of symptoms, including pain, function, and quality of life. PROMIS utilizes Item Response Theory, which ensures that each individual question is validated for application to the objective of the test as a whole. PROMIS is increasingly being used to study outcomes from spine surgery and has been compared to more traditional spine PRO assessment scales [36]. As highlighted in this analysis, only one study to date has used PROMIS to assess PROs in ACD.
Considering the variability in the tools used to assess PROs in ACD and the uncertainty with how best to measure clinical improvement, we sought to review and analyze these metrics as they related to alignment correction. This meta-analysis shows that PROs correlated with some cervical and global spine alignment parameters better than others. Notably, increases in C2ŌĆō7 SVA and C7ŌĆōS1 SVA were associated with worse NDI and EQ-5D respectively. The correction of other spinal parameters correlated poorly with improvements in HRQoL, revealing that at present, PROs explain and capture a small proportion of the variance in cervical and global spinal parameters. In fact, PROs were broadly used to assess pain, physical activity, mental status, and daily activity, without asking about more specific symptoms that are commonly associated with ACD, including difficulty with swallowing, maintaining horizontal gaze, and respiration. Although studies have validated PROs in cervical myelopathy and radiculopathy using legacy instruments, ACD arguably represents a more complex entity of cervical spine pathology for which conventional outcomes assessments may not capture the extent of impact or benefit on HRQoL [7,37].
Defining ACD and postoperative clinical outcomes through identification of specific domains and validated PROs is an important step toward phenotyping ACD. Ames et al. [2] proposed a novel classification system for ACD based on determining the plane (sagittal and coronal), location, and apex of the cervical deformity complemented by 5 modifiers including sagittal parameters (C2ŌĆō7 SVA, CBVA, TSŌĆōCL), myelopathy severity, and SRS-Schwab classification for global spine assessment. The Ames-ACD classification was used in many of the included studies to objectively report, and study ACD, yet the association between global and regional spine sagittal parameters, and present PROs need further investigation to better characterize severity and disability. Having identified drivers of cervical deformity, further work is now needed to determine which PROs can best measure the variance in ACD modifiers as well as postoperative recovery, taking into consideration the presenting symptoms of patients seeking correction of their deformity. Studies are required to validate PROs that can be used to guide the extent of sagittal correction, measure postoperative clinical outcomes at difference time points, and meet patient expectations after an intervention has been performed. Given the invasiveness of surgery and the techniques used to achieve such correction, better stratification of alignment correction goals with PROs is critical.
This review shows that there is clearly interest in studying these measures in ACD. More studies utilizing and reporting PROs to evaluate interventions for ACD suggest that this aspect of spine care is clinically important yet still incompletely defined or understood. A detailed understanding of the influence of segmental, regional, and global spine balance on outcomes in ACD is key to correlate PROs including HRQoL following cervical deformity correction [3]. Most studies examined the association between cervical regional parameters (C2ŌĆō7 SVA, C2ŌĆō7 cobb angle, TSŌĆōCL) and PROs, with still nonconclusive results regarding how these parameters relate to clinical outcomes. Many of these parameters including the T1 slope has been studied in recent years and our understanding of these parameters and how they relate to global spinal parameters continue to evolve [38]. For instance, the T1 slope is a measure that is increasingly being studied as a surrogate for the amount of cervical lordosis required. It is defined as the angle between a line drawn across the upper endplate of the T1 vertebra and the horizontal axis. Similar to the relationship between PI and LL, a greater T1 slope suggests that a greater degree of cervical lordosis is required to maintain neutral sagittal alignment. As such, a mismatch in cervical lordosis relative to T1 slope is important to recognize, particularly when planning surgery. Recent studies have sought to compare T1 slope as well as TSŌĆōCL with other measures of cervical misalignment as potential markers of deformity severity and postoperative outcomes [2,39-41].
Though the aforementioned cervical parameters are the most common radiographic parameters used for preoperative planning and postoperative radiographic assessment, a more detailed assessment of subjacent segments, including thoracolumbar and pelvis should be factored in the analysis of clinical outcomes, considering the chain of correlation between regional sagittal parameters and the related compensatory mechanisms that take place [42]. Another challenge is determining the MCID for PROs, defined as the smallest change that patients perceive as beneficial after ACD correction, considering that statistically significant improvements after treatment does not guarantee that the person with corrected ACD has an improved functional capacity or quality of life.
In addition to demographic, clinical, and surgical factors, radiographic parameters such as severe TSŌĆōCL, and global parameters such as severe C2ŌĆōT3 SVA, global C7ŌĆōS1 SVA, and PT were associated with poor outcomes after ACD correction [19]. These findings could be reflective of coincidental thoracolumbar malalignment, which is often noted in ACD and evidently recognized by the Ames-ACD classification, further highlighting the importance of subjacent deformity and the chain of correlation between cervical-specific and global alignment [43]. While cSVA, TSŌĆōCL, and CBVA improvements were associated with better postoperative HRQoL, more severe spinopelvic mismatch and pelvic retroversion had a negative impact on cervical pain and discomfort after surgery [32]. Improving the sagittal balance was associated with improved myelopathy and HRQoL in cervical deformity [16]. Moreover, an improvement in myelopathy was found to be more important to overall patient outcomes than improvement in spinal alignment alone [16]. A better understanding of myelopathy recovery in relation to the degree of correction of the cervical deformity and compensation of global spine parameters is needed during follow-up after ACD correction.
By summarizing the available literature, we demonstrate that cervical and global spine parameters were variably associated with present PROs, suggesting that more research is still needed to guide the correction of the deformity based on predicted changes in PROs. However, it is key to note that association does not imply causation, meaning that a change in alignment can be associated with a change in PROs but does not mean that a change in alignment actually causes a change in PROs. Other factors including frailty, progressive myelopathy, symptoms duration and severity, complications, and rehabilitation could influence clinical outcomes following surgical correction of ACD. Passias et al. [16] demonstrated that improvements in myelopathy contribute to better PROs following ACD corrective surgery than just improving the alignment alone. The respective roles of both cervical realignment and direct decompression on PROs need further investigation, since cervical kyphosis can cause flattening of the spinal cord and increase the intramedullary cord pressure leading to neuronal loss and atrophy of the anterior fasciculus and anterior horn [42]. Also, the long-term clinical outcome could be worse in deformities showing intramedullary signal intensity changes on magnetic resonance images, owing to cellular necrosis secondary to ischemia of the anterior spinal artery and from the repeated microtrauma inflicted on the spinal cord from an unstable cervical spine [44]. Moreover, the ISSG demonstrated an association between frailty and HRQoL, suggesting that one of the goals of surgery for ACD should be to reduce frailty by addressing the modifiable factors of the proposed frailty index for cervical deformity like anxiety, unsteady gait, and leg weakness [37].
This review has several limitations restricting the ability to study the association of cervical parameters and PROs in a meta-analysis. Although a large number of studies was included, we were limited by the granularity of the data extracted and the lack of availability of correlation coefficients and confidence intervals. Most studies put more emphasis on p-value and statistical significance, rather than the magnitude of the observed correlations (with r=0 indicating no correlation and r=1 a perfect correlation). The low p-value of the correlation coefficients only indicates that the chance that the actual correlation coefficient is very different from the observed value is small. Considering that the pooled effect estimate could not be calculated for all parameters given the limitations, the correlation between cervical parameters and PROs requires further study. Furthermore, MCID thresholds should be interpreted with caution, considering the variability of the reported values for legacy metrics. An additional limitation is that most postoperative outcomes were collected at 1 year and information about PROs beyond this timepoint is limited. Only one study attempted to compare PROMIS with legacy metrics but this study had a small sample size which limited subgroup analysis for ACD [7]. Further study with PROMIS domains, which utilizes CAT methods, could potentially avoid the floor and ceiling effects associated with commonly used metrics and may provide more sensitive tools to detect HRQoL changes in ACD.
This review demonstrates that correcting ACD to specific alignment parameters inconsistently translates to improvement in PROs. Despite these limitations, we found that increases in C2ŌĆō7 SVA and C7ŌĆōS1 SVA were associated with worse NDI and EQ-5D respectively. Given the lack of specific PRO assessment tools for ACD, further study is needed to better quantify goals for alignment correction to maximize the HRQoL benefits for patients.
SUPPLEMENTARY MATERIALS
Supplementary method 1, Tables 1 and 2 can be found via https://doi.org/10.14245/ns.2040656.328.
Fig.┬Ā2.
Summary of the association between patient-reported outcome measures (PROMs) and cervical modifiers appearing in the Ames-ISSG Cervical Spine Classification. Panel A shows the association between cervical C2ŌĆō7 sagittal vertical axis (SVA) and PROMs. Panel B shows the association between T1 slope minus C2ŌĆō7 lordosis (TSŌĆōCL) and PROMs. Panel C shows the association between chin-brow vertical angle (CBVA) and PROMs. Panel D shows the association between Schwab-SRS parameters, including pelvic tilt (PT), PI minus LL, C7-SVA, and PROMs. Red color indicates a poor correlation (0 <rŌēż0.3), orange color indicates a fair correlation (0.3 <rŌēż0.5), light green indicates a moderate correlation (0.5 <rŌēż0.8), and green indicates a strong correlation (0.8 <rŌēż1). (a) indicates the correlation was significant (p < 0.05). (b) indicates the correlation was not significant. (First Author et al.) refers to the study in the reference list. mJOA, modified Japanese Orthopedic Association; VAS, visual analogue scale; NDI, Neck Disability Index; EQ-5D, EuroQoL 5-Dimension; PROMIS, Patient-Reported Outcomes Measurement System; PF, physical function; ISSG, International Spine Study Group; SF-36, 36-item Short Form Health Survey; TSŌĆōCL, T1 slope minus cervical lordosis; TK, thoracic kyphosis; PT, pelvic tilt; PI, pelvic incidence; LL, lumbar lordosis.
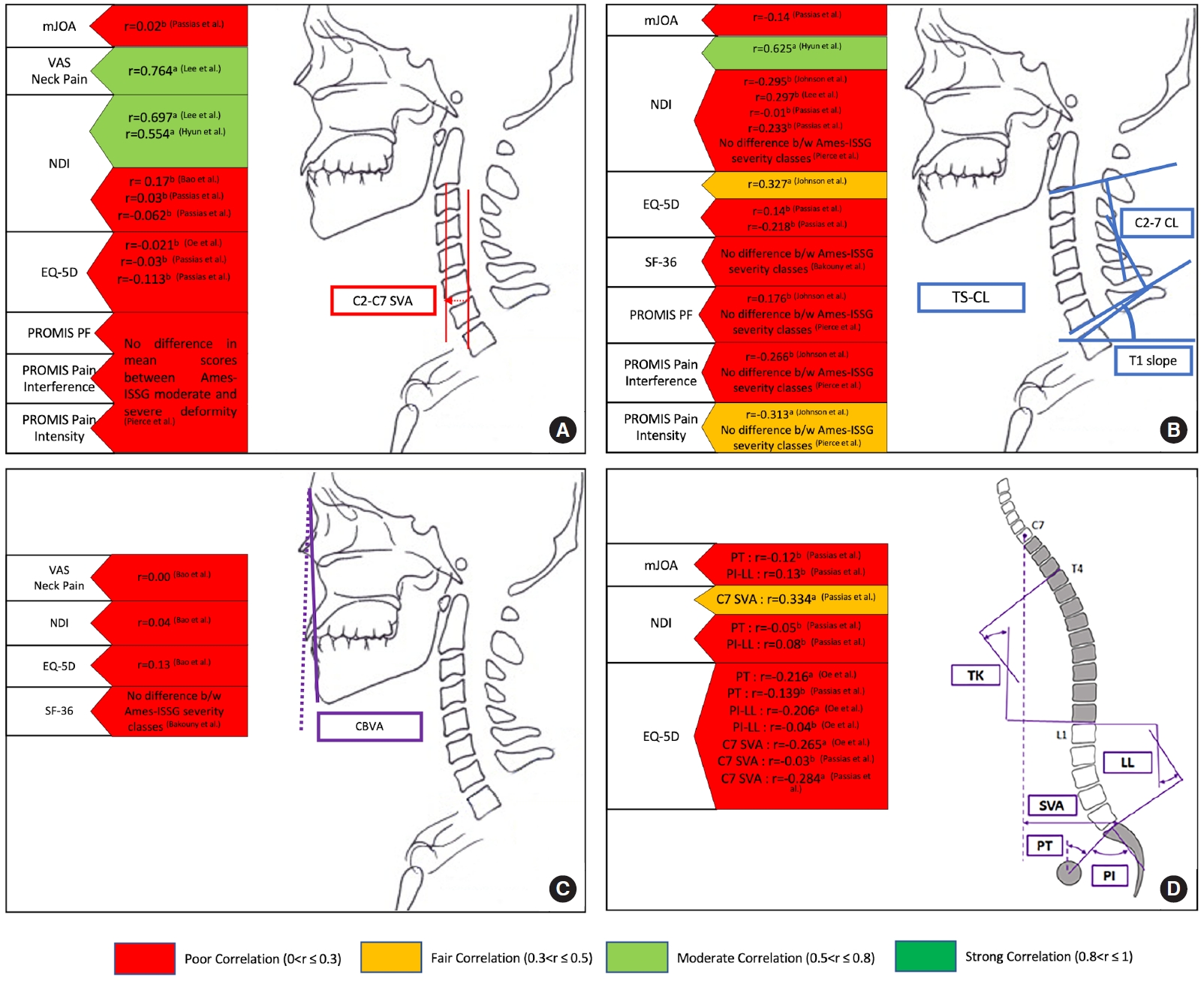
Fig.┬Ā3.
Forest graphs showing the meta-analyses of correlation coefficients (converted to z-scores) between C2ŌĆō7 sagittal vertical axis (SVA) (A, B), T1 slope minus cervical lordosis (TSŌĆōCL) (C, D), C7ŌĆōS1 SVA (E), and patient-reported outcomes. NDI, Neck Disability Index; COR, correlation; CI, confidence interval; EQ-5D, EuroQoL 5-Dimension.
Table┬Ā1.
Ames-ISSG Cervical Deformity Classification by Ames et al.
REFERENCES
1. Steinmetz MP, Stewart TJ, Kager CD, et al. Cervical deformity correction. Neurosurgery 2007 60(1 Supp1 1):S90-7.


2. Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015 23:673-83.


3. Smith JS, Line B, Bess S, et al. The health impact of adult cervical deformity in patients presenting for surgical treatment: comparison to united states population norms and chronic disease states based on the EuroQuol-5 Dimensions questionnaire. Neurosurgery 2017 80:716-25.


4. Pierce K, Alas H, Brown A, et al. PROMIS physical health domain scores are related to cervical deformity severity. J Craniovertebral Junction Spine 2019 10:179.

5. Kim HJ, Piyaskulkaew C, Riew KD. Comparison of smith-petersen osteotomy versus pedicle subtraction osteotomy versus anterior-posterior osteotomy types for the correction of cervical spine deformities. Spine 2015 40:143-6.


6. Lau D, Ziewacz JE, Le H, et al. A controlled anterior sequential interbody dilation technique for correction of cervical kyphosis. J Neurosurg Spine 2015 23:263-73.


7. Boody BS, Bhatt S, Mazmudar AS, et al. Validation of Patient-Reported Outcomes Measurement Information System (PROMIS) computerized adaptive tests in cervical spine surgery. J Neurosurg Spine 2018 28:268-79.



8. European Spine Study Group; International Spine Study Group; Ames CP, et al. Development of predictive models for all individual questions of SRS-22R after adult spinal deformity surgery: a step toward individualized medicine. Eur Spine J 2019 28:1998-2011.


9. Asher AL, Devin CJ, Kerezoudis P, et al. Comparison of outcomes following anterior vs posterior fusion surgery for patients with degenerative cervical myelopathy: an analysis from quality outcomes database. Neurosurgery 2019 84:919-26.


10. Crawford CH, Glassman SD, Bridwell KH, et al. The minimum clinically important difference in SRS-22R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine 2015 40:377-81.


11. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009 339:b2535.



12. Veritas Health Innovation. Covidence systematic review software. Melbourne: Veritas Health Innovation; 2016.
13. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010 25:603-5.


14. Ailon T, Smith JS, Shaffrey CI, et al. Outcomes of operative treatment for adult cervical deformity: a prospective multicenter assessment with 1-year follow-up. Neurosurgery 2018 83:1031-9.


15. Poorman GW, Passias PG, Horn SR, et al. Despite worse baseline status depressed patients achieved outcomes similar to those in nondepressed patients after surgery for cervical deformity. Neurosurg Focus 2017 43:E10.

16. Passias PG, Horn SR, Bortz CA, et al. The relationship between improvements in myelopathy and sagittal realignment in cervical deformity surgery outcomes. Spine 2018 43:1117-24.


17. Passias PG, Segreto FA, Lafage R, et al. Recovery kinetics following spinal deformity correction: a comparison of isolated cervical, thoracolumbar, and combined deformity morphometries. Spine J 2019 19:1422-33.


18. Virk S, Passias P, Lafage R, et al. Intraoperative alignment goals for distinctive sagittal morphotypes of severe cervical deformity to achieve optimal improvements in health-related quality of life measures. Spine J 2020 20:1267-75.


19. Horn SR, Passias PG, Oh C, et al. Predicting the combined occurrence of poor clinical and radiographic outcomes following cervical deformity corrective surgery. J Neurosurg Spine 2020 32:182-90.

20. Segreto FA, Lafage V, Lafage R, et al. Recovery kinetics: comparison of patients undergoing primary or revision procedures for adult cervical deformity using a novel area under the curve methodology. Neurosurgery 2019 85:E40-51.


21. Protopsaltis TS, Ramchandran S, Tishelman JC, et al. The importance of C2-slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine J 2017 17:S48.

22. Johnson B, Stekas N, Ayres E, et al. PROMIS correlates with legacy outcome measures in patients with neck pain and improves upon NDI when assessing disability in cervical deformity. Spine 2019 44:982-8.


23. Grosso MJ, Hwang R, Mroz T, et al. Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery: clinical article. J Neurosurg Spine 2013 18:537-44.

24. Bao H, Varghese J, Lafage R, et al. Principal radiographic characteristics for cervical spinal deformity: a health-related quality-of-life analysis. Spine 2017 42:1375-82.


25. Bakouny Z, Khalil N, Otayek J, et al. Are the sagittal cervical radiographic modifiers of the Ames-ISSG classification specific to adult cervical deformity? J Neurosurg Spine 2018 29:483-90.


26. Oe S, Togawa D, Yoshida G, et al. Difference in spinal sagittal alignment and health-related quality of life between males and females with cervical deformity. Asian Spine J 2017 11:959-67.



27. Lee JS, Youn MS, Shin JK, et al. Relationship between cervical sagittal alignment and quality of life in ankylosing spondylitis. Eur Spine J 2015 24:1199-203.


28. Hyun SJ, Han S, Kim KJ, et al. Assessment of T1 slope minus cervical lordosis and C2-7 sagittal vertical axis criteria of a cervical spine deformity classification system using long-term follow-up data after multilevel posterior cervical fusion surgery. Oper Neurosurg 2019 16:20-6.

29. Zhong J, Pan Z, Chen Y, et al. Postoperative cervical sagittal realignment improves patient-reported outcomes in chronic atlantoaxial anterior dislocation. Oper Neurosurg 2018 15:643-50.

30. Protopsaltis TS, Ramchandran S, Hamilton DK, et al. Analysis of successful versus failed radiographic outcomes after cervical deformity surgery. Spine 2018 43:E773-81.


31. International Spine Study Group (ISSG); Passias PG, Horn SR, et al. Evaluating cervical deformity corrective surgery outcomes at 1-year using current patient-derived and functional measures: are they adequate? J Spine Surg 2018 4:295-303.



32. Passias PG, Jalai CM, Smith JS, et al. Characterizing adult cervical deformity and disability based on existing cervical and adult deformity classification schemes at presentation and following correction. Neurosurgery 2018 82:192-201.


33. Iyer S, Nemani VM, Nguyen J, et al. Impact of cervical sagittal alignment parameters on neck disability. Spine 2016 41:371-7.


34. Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care 2007 45(Suppl 1):S3-11.

35. Brodke DJ, Saltzman CL, Brodke DS. PROMIS for orthopaedic outcomes measurement. J Am Acad Orthop Surg 2016 24:744-9.


36. Brodke DS, Goz V, Voss MW, et al. PROMIS PF CAT outperforms the ODI and SF-36 physical function domain in spine patients. Spine 2017 42:921-9.



37. Miller EK, Ailon T, Neuman BJ, et al. Assessment of a novel adult cervical deformity frailty index as a component of preoperative risk stratification. World Neurosurg 2018 109:e800-6.


38. Martini ML, Neifert SN, Chapman EK, et al. Cervical spine alignment in the sagittal axis: a review of the best validated measures in clinical practice. Global Spine J 2020 Nov 18 2192568220972076. https://doi.org/10.1177/2192568220972076. [Epub].

39. Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2015 76 Suppl 1:S14-21.


40. Staub BN, Lafage R, Kim HJ, et al. Cervical mismatch: the normative value of T1 slope minus cervical lordosis and its ability to predict ideal cervical lordosis. J Neurosurg Spine 2019 30:31-7.

41. Lan Z, Huang Y, Xu W. Relationship between T1 slope minus C2-7 lordosis and cervical alignment parameters after adjacent 2-level anterior cervical diskectomy and fusion of lower cervical spine. World Neurosurg 2019 122:e1195-201.


42. Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013 19:141-59.


- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2