 |
 |
- Search
|
|
||
Abstract
Anterior surgical approaches to the cervical spinal pathology have become a frequently used technique. Anterior cervical spine surgeries are generally considered to be safe with low incidence of neurological complications. Vertebral artery (VA) injuries are infrequent during an anterior cervical spine approach but can be devastating. A retrospective review of these injuries documents an incidence of 0.3%–0.5%. However, there is no established strategy or guidelines for managing iatrogenic VA injuries. We describe a case of iatrogenic VA injury at C5 vertebral level during an anterior cervical approach for C5 cervical osteoblastoma; successful managed by endovascular coiling using detachable coils achieving complete occlusion. The patient had a good clinical outcome, with no symptoms of vertebrobasilar insufficiency at 2-year follow-up. There is a paradigm shift in the management of the VA injury after introduction of the interventional angiography. Endovascular embolization is a safe and effective treatment option, which offers certain advantages over open surgery such as minimal invasion, lower risk of neurological injury, lower morbidity, and recurrence rates.
Anterior surgical approaches to the cervical spinal pathology have become a frequently used technique for conditions like degenerative disc disease, fractures, spondylosis, infections, and neoplasms. Anterior cervical spine surgeries are generally considered to be safe with low incidence of neurological complications [1]. Injuries to the vertebral artery (VA) are infrequent during anterior approach but can be lethal, with serious complications like pseudoaneurysm, arteriovenous fistula, delayed hemorrhage, thromboembolism, ischemic stroke, and death [2-4]. A retrospective review of these injuries documents an incidence of 0.3%–0.5%. Prompt management of the complications can decrease the morbidity and mortality from VA injury (VAI) [5]. However, there is no established consensus or strategy for the management of VAI in anterior cervical spine surgeries. In this article, we report a case of iatrogenic VAI at C5 vertebral level during cervical spinal surgery for C5 cervical osteoblastoma; successful managed by endovascular coiling using detachable coils achieving complete occlusion.
A 19-year-old girl was transferred to our Emergency Department, after undergoing an anterior cervical spine surgery for a cervical spine pathology at another institution. Her preoperative computed tomography (CT) scan showed an expansile bony lesion centered on the right C5 pedicle and lamina with mixed sclerotic/lytic internal matrix and prominent sclerotic rim, suggesting an osteoblastoma. The lesion had a close relationship with the right VA canal. During surgery, profuse and uncontrollable arterial bleeding was encountered while drilling the right C5 pedicle. The initial hemostasis was achieved by packing, and the anterior interbody fusion with cervical plate was done. In our institution, she underwent a CT cerebral angiogram which revealed complete transection of right VA. Catheter angiography from right VA demonstrated an abrupt cutoff of second part (V2) of the VA. Left VA angiogram revealed normal caliber VA without any significant abnormality. Then, 5F Envoy guide catheter was positioned in V2 segment of the left VA. Subsequently by using Excelsior SL10 microcatheter Excelsior SL 10 (Stryker Neurovascular, Fremont, CA, USA) & 0.014- inch traxcess microwire the right VA was cannulated retrogradely using cross-over technique via vertebrobasilar junction. The microcatheter was navigated close to transected site and the angiographic run revealed active extravasation of the contrast (Fig. 1). Because of the extensive vessel injury, reconstructive approach was not feasible. Also, there is a possibility of steal phenomena from the opposite VA, so the vessel both proximal and distal to the injured site was occluded using detachable coils to avoid retrograde filling of the fistula. Postprocedure angiogram revealed complete obliteration of the right VAI (Fig. 2). The schematic illustration of the endovascular procedure is described in Fig. 3. The patient had a good clinical outcome, with no symptoms of vertebrobasilar insufficiency at 2-year follow-up.
VAI during an anterior cervical spinal approach is an uncommon but potential life-threatening complication. If bleeding is not controlled carefully, risk of severe hypotension is present with increased mortality [6]. The exact incidence of these VA injuries during anterior decompressive surgery is not known. Smith et al. [7] reported an incidence of 0.5% (10 out of 1,195 operations) in their retrospective review. The causes that they emphasized were: off midline drill; removal of excessive bone and disc; or pathological softening of the bone, due to preexisting infection or tumor. Two scenarios may account for iatrogenic VAI during anterior cervical spine procedures. The first is unrecognized tortuosity of the VA or other anomalies. Careful attention to the preoperative CT and magnetic resonance imaging studies may reveal dilated or tortuous VA anatomy, which can then be avoided intraoperatively. The second scenario involves inadvertent wide dissection, which should be avoided taking the location of the VA into consideration [5]. However, in our case the intraoperative bleeding from venous plexus that cover the lateral mass obscured the surgical field leading to VA injury. Therefore, care must be taken during the dissection and maintaining good hemostasis is important.
Bleeding from VAI can be controlled initially by using thrombostatic drugs, along with direct compression. Treatment options include continued local compression, microvascular surgical repair, and VA ligation. Endovascular embolization has also been described as an alternative approach [8]. Injury to the 2nd and 3rd segments of the VA are extremely difficult to expose, as it runs within the bony canal formed by foramen transversarium. So, surgery is not always the best option. The therapeutic goal is to repair the VAI with preservation of the normal patency of the VA [9].
Microvascular surgical repair restores the patency of the VA, minimizing the possibilities of ischemic complications [10]. Nevertheless, the procedure is technically challenging. VA ligation is associated with significant periprocedural complications. Neurological complications like brainstem and cerebellar infarcts, cranial nerve palsies, and hemiplegia have been reported after VA ligation [11]. The outcome following VA ligation depends upon sufficient filling of basilar artery by opposite VA. Generally, in 5.7% of cases, the left VA is hypoplastic and absent entirely in 1.8% of cases. The right VA is hypoplastic in 8.8% and absent in 3.1% of cases [12]. Unilateral VA ligation is well tolerated by majority of the patients. Few patients, will have an occluded or stenotic VA, VA ending in the posterior inferior cerebellar artery, or poor collateralization of the posterior circulation. Ligation of the VA in these conditions can cause brainstem or cerebellar infarcts. Shintani and Zervas [11] reported a 12% mortality rate after unilateral VA ligation. Effort should be made to maintain the patency of the artery, since the status of the VA is unlikely to be known before surgery and long-term complications of the VA ligation are still unclear.
There is a paradigm shift in the management of the VAI after introduction of the endovascular management, which offers certain advantages over open surgery like less invasive, minimal risk of neurological complications with lower morbidity and recurrence rates. Intraoperative angiography helps in the urgent evaluation of the VAI and identification of status of the opposite VA. Moreover, as diagnostic angiogram and endovascular management can be performed in the same setting, prompt detection and management of vascular complications are possible [5].
Endovascular management includes deconstructive (parent artery occlusion, coil trapping) and reconstructive (covered stent or stent graft placement) techniques. Stent graft provides a reconstructive method that treats the VAI while maintaining arterial patency. Injury to the dominant VA, may cause catastrophic thromboembolic complications like brainstem ischemia and death. In these cases, parent artery reconstruction using covered stents or stent graft would be the preferred management. For cases not amenable to endovascular treatment, or that have failed endovascular treatment surgical bypass procedures like occipital artery–VA bypass may be considered [13]. However, these procedures are technically challenging and require the patient to withstand surgery and its accompanying risks. In extensive vessel injury like transection, parent vessel has to be sacrificed as reconstructive approach is not feasible. Parent artery occlusion of an injured VA can be done if there is a dominant contralateral VA or a sufficient collateralization of the circle of Willis [14]. There is a possibility of steal phenomena from the opposite VA, so the vessel both proximal and distal to the injured site should be occluded to avoid retrograde filling of the fistula. Also, we reiterate the fact that during angiogram, selective cannulation of the distal ipsilateral VA should be done using microcatheter ‘cross-over’ technique via contralateral VA. This technique may unmask the actual pathology especially in cases of false-negative angiogram like in this case. Cases of less severe VAI like dissection/intramural hematoma with thromboembolic phenomena, can be managed with antiplatelet agents such as aspirin and clopidogrel for a 3-month period. Other options for anticoagulation in VAI include, immediate anticoagulation using heparin, followed by 3 months of oral anticoagulants, with a target International normalized ratio of 2–3 based upon patient comorbidities and any relative contraindications to anticoagulation. There is no consensus on the choice of drug for anticoagulation with recent evidence suggesting equivalent effects of heparin and antiplatelet agents in preventing recurrent ischemic events in patients with extracranial VA dissection [15]. Endovascular revascularization procedures can be reserved for cases with recurrent neurological events despite on antithrombotics. The implication of this case report is the awareness and identification of the VAI and its complications through an anterior cervical surgical exposure. Endovascular embolization is a safe and effective treatment option, for the management of the VAI.
Iatrogenic VA injuries are uncommon, but potentially lethal complication of anterior cervical spine operation. Injuries need to be promptly detected and managed with either direct compression, microvascular repair, or vessel ligation. Management of these VAI has been revolutionized by the supportive role of interventional radiology like assessment of the injured site and status of the contralateral VA. Endovascular treatment offers certain advantages over open surgery like less invasive, minimal risk of neurological complications with lower morbidity and recurrence rates.
ACKNOWLEDGEMENTS
We acknowledge Dr. Harshit Kramadhari, K S Hegde Medical Academy, Mangalore, India, for the schematic illustration (Fig. 3).
Fig. 1.
(A) Angiogram of right vertebral artery shows an abrupt cutoff at V2 portion of right vertebral artery (black arrow). (B) Left vertebral artery angiogram show, retrograde filling of right vertebral artery, however there is no contrast extravasation demonstrated. (C) Excelsior SL-10 microcatheter is navigated into left distal vertebral artery and advanced retrogradely into right distal vertebral artery (white arrow) using cross-over technique. (D) Angiogram of the right vertebral artery through the microcatheter shows extravasation of contrast media at the level of C5, opacifying the surgical drain (arrow head) in the operated site.

Fig. 2.
(A) Trapping of the right vertebral artery by detachable coils through antegrade and retrograde technique. Antegrade (B) and retrograde (C) check angiograms demonstrate successful trapping of transected segment of right vertebral artery after deployment of the coils.
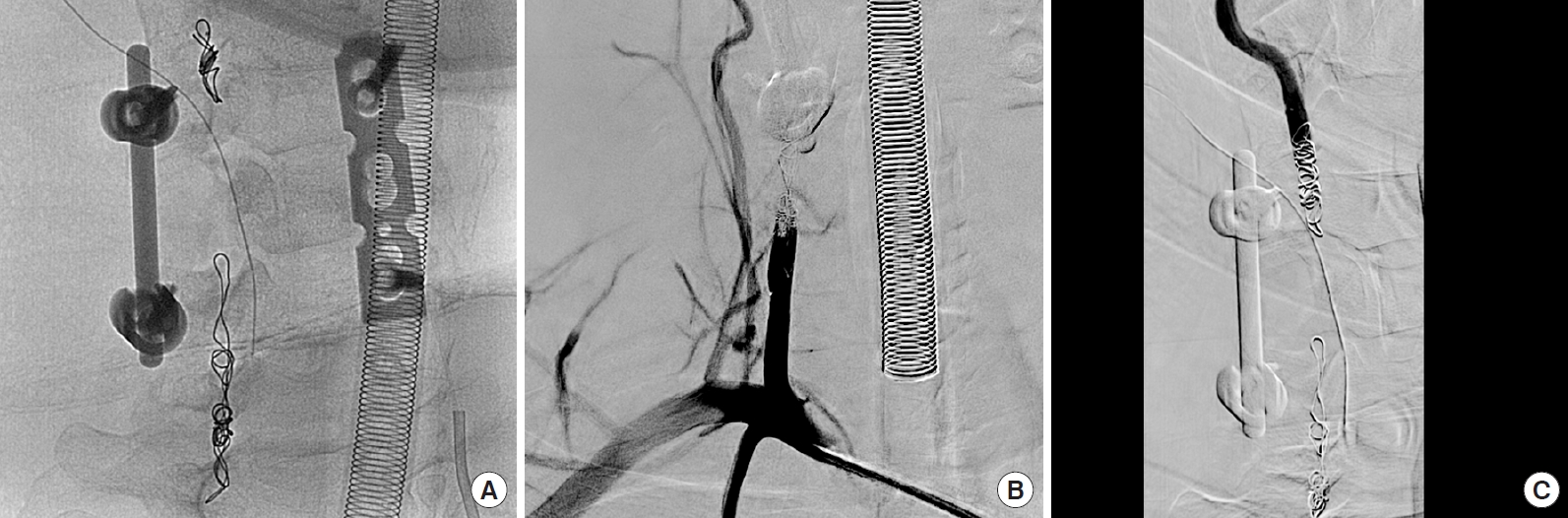
Fig. 3.
(A) Anatomy of the vertebral artery (VA) and its segments with the relation of the right C5 osteoblastoma which was operated. (B) Site of transection (curved arrow) at the level C5 vertebral body. (C) Access obtained through the bilateral VA. The arrows denote the direction of the catheter from right VA (blue arrows) and left VA (black arrow). (D) Coil mass secured in the ends of the transected vertebral artery with cessation of the active extravasation of blood. BA, basilar artery; OB, osteoblastoma; RVA, right vertebral artery; LVA, left vertebral artery; RSCA, right subclavian artery; LSCA, left subclavian artery.

REFERENCES
1. Choi JW, Lee JK, Moon KS, et al. endovascular embolization of iatrogenic vertebral artery injury during anterior cervical spine surgery: report of two cases and review of the literature. Spine 2006 31:E891.


2. Grabowski G, Cornett CA, Kang JD. Esophageal and vertebral artery injuries during complex cervical spine surgery—avoidance and management. Orthop Clin North Am 2012 43:63. -74. viii.


3. Neo M, Fujibayashi S, Miyata M, et al. Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine 2008 33:779-85.


4. Peng CW, Chou BT, Bendo JA, et al. Vertebral artery injury in cervical spine surgery: anatomical considerations, management, and preventive measures. Spine J 2009 9:70-6.


5. Burke JP, Gerszten PC, Welch WC. Iatrogenic vertebral artery injury during anterior cervical spine surgery. Spine J 2005 5:508. -14. discussion 514.


6. Daentzer D, Deinsberger W, Böker DK. Vertebral artery complications in anterior approaches to the cervical spine: report of two cases and review of literature. Surg Neurol 2003 59:300. -9. discussion 309.

7. Smith MD, Emery SE, Dudley A, et al. Vertebral artery injury during anterior decompression of the cervical spine. A retrospective review of ten patients. J Bone Joint Surg Br 1993 75:410-5.


8. Cosgrove GR, Théron J. Vertebral arteriovenous fistula following anterior cervical spine surgery. Report of two cases. J Neurosurg 1987 66:297-9.

9. Mwipatayi BP, Jeffery P, Beningfield SJ, et al. Management of extra-cranial vertebral artery injuries. Eur J Vasc Endovasc Surg 2004 27:157-62.


10. Golfinos JG, Dickman CA, Zabramski JM, et al. Repair of vertebral artery injury during anterior cervical decompression. Spine 1994 19:2552-6.


11. Shintani A, Zervas NT. Consequence of ligation of the vertebral artery. J Neurosurg 1972 36:447-50.


12. George B, Laurian C. The vertebral artery: pathology and surgery. New York: Springer-Verlag; 1987.
13. Wang X, Tong X, Shi M, et al. Occipital artery to extradural vertebral artery bypass for posterior circulation ischemia. Oper Neurosurg (Hagerstown) 2019 16:527-38.



- TOOLS



























