 |
 |
- Search
|
|
||
See commentary "Commentary on ŌĆ£Mini-Open Intercostal Retroperitoneal Approach for Upper Lumbar Spine Lateral Interbody FusionŌĆØ" in Volume 20 on page 564.
Abstract
Objective
Conventional oblique lumbar interbody fusion (OLIF) approach is possible from the L2/3 to L4/5 levels. However, obstruction of the lower ribs (10thŌĆō12th) makes it difficult to maintain disc parallel maneuvers or orthogonal maneuvers. To overcome these limitations, we proposed an intercostal retroperitoneal (ICRP) approach to access the upper lumbar spine. This method does not expose the parietal pleura or require rib resection and employs a small incision.
Methods
We enrolled patients who underwent a lateral interbody procedure on the upper lumbar spine (L1/2/3). We compared the incidence of endplate injury between conventional OLIF and ICRP approaches. In addition, by measuring the rib line, the difference in endplate injury according to rib location and approach was analyzed. We also analyzed the previous period (2018ŌĆō2021) and the year 2022, when the ICRP has been actively applied.
Results
A total of 121 patients underwent lateral interbody fusion to the upper lumbar spine (OLIF approach, 99 patients; ICRP approach, 22 patients). Endplate injuries occurred in 34 of 99 (34.3%) and 2 of 22 patients (9.1%) during the conventional and ICRP approaches, respectively (p = 0.037; odds ratio, 5.23). When the rib line was located at the L2/3 disc or L3 body, the endplate injury rate was 52.6% (20 of 38) for the OLIF approach but 15.4% (2 of 13) for the ICRP approach. Since 2022, the proportion of OLIF including L1/2/3 levels has increased 2.9-fold.
Oblique lumbar interbody fusion (OLIF) has recently been in the spotlight owing to its advantages of indirect decompression and minimal invasiveness. In particular, the advantages of a short operation time and less bleeding volume are emphasized in multilevel surgery rather than in single-level surgery [1]. Direct lateral interbody fusion (DLIF) is a similar approach to OLIF, but DLIF is only applied in limited range of lumbar spines owing to obstructions of the rib and pelvis. In contrast, OLIF can be applied in a relatively wide range because it can gain access despite interference of the pelvis [2-4].
The OLIF approach can reach L2ŌĆō5 levels. However, L1/2 is inaccessible owing to rib obstruction, and in some patients, L2/3 is also difficult to access. If the procedure is forcibly performed even with rib obstruction, an endplate injury is common because performing a procedure parallel to the disc is impossible, as shown in Fig. 1.
Endplate injury is one of the more concerning complications of OLIF, which is mainly aimed at indirect decompression [5-10]. In case of failure of disc height restoration owing to endplate injury, indirect decompression may be inadequate, resulting in incomplete surgical outcomes or the need for additional laminectomy [5,7,9,10].
When OLIF is performed for deformity correction, endplate preservation is important for scoliosis correction and sagittal alignment restoration. Endplate injuries result in insufficient correction, leading to additional fusion or suboptimal outcomes [11-13]. In this regard, best efforts are needed to reduce endplate injuries when performing OLIF on the upper spine.
The upper lumbar spine can also be fixed using posterolateral fusion (PLF) or posterior lumbar interbody fusion (PLIF). However, since OLIF mainly uses percutaneous pedicle screws (PPS) for posterior fixation, the combination of OLIF and PLF/PLIF has limitations, such as additional incisions in the posterior back, muscle injuries, more bleeding, and longer operation times [14]. In this regard, accessing the upper lumbar spine from the same lateral position has advantages in that it reduces operation time and bleeding and enables the use of PPS.
Previous studies have focused on the approach of upper lumbar spine corpectomy, which requires rib resection [15-19]. Studies of OLIF access to the upper lumbar spine are limited, and the recently published paper by Mitsui et al. [20] is the only search result. In this study, the location of the rib varied from patient to patient, particularly for thoracic kyphosis and scoliosis. The authors reported that a considerable number of patients required rib resection to access the upper lumbar spine. However, complications following rib resection, such as chronic pain in the chest wall, pneumothorax, and chest tube insertion are a burden to spine surgeons. Therefore, we considered ways of accessing the upper lumbar spine without rib resection and have devised an approach.
We noted the location of the lower ribs and parietal pleura. As shown in Fig. 2, the parietal pleura descends posteriorly to the 12th rib, but it descends laterally to the 10th rib [21-23]. In the lateral position, the distal intercostal space between the 10th and 12th ribs is a space without parietal pleura. If we approach this area, we can reach the retroperitoneal space through dissection of the intercostal muscle and diaphragm. This approach does not require rib resection and is less likely to expose the parietal pleura. Thus, we devised an intercostal retroperitoneal (ICRP) approach to access the upper lumbar spine for OLIF.
In this study, we provided a detailed description of the surgical technique and complications associated with the ICRP approach. In addition, we compared the endplate injury rate of the upper lumbar spine between the conventional OLIF and ICRP approaches according to the rib position.
The Institutional Review Board (IRB) of our institution approved the study protocol and waived the requirement for informed consent owing to the retrospective nature of this study (IRB number: 05-2022-214). All procedures involving human participants were performed according to the ethical standards of the IRB of the hospital.
Our institution performed 677 OLIF procedures between April 2018 and December 2022. Among them, we enrolled patients as following inclusion criteria; (1) Degenerative lumbar stenosis, spondylolisthesis, degenerative scoliosis, degenerative kyphosis, or adjacent segment disease that did not respond to medications and conservative treatments for more than 6 weeks, (2) demineralized bone matrix (DBM) filling polyetheretherketone (PEEK) cage, (3) OLIF was performed on the upper lumbar spine (L1/2 or L2/3 or L1/2/3), (4) OLIF was extended form the upper lumbar spine (L1/2 or L2/3 or L1/2/3) to the lower lumbar spine (L3/4/5/S1) (Fig. 3). We excluded patients as following exclusion criteria: (1) surgery due to infection, trauma, or tumor, (2) using interbody material other than PEEK+DBM, (3) among multilevel fusions, simple posterior fixation of the upper lumbar spine without OLIF (L1/2 or L2/3 or L1/2/3), (4) patients in whom additional surgeries at the index level during the follow-up period were excluded. Demographic data such as body mass index (BMI), bone mineral density (BMD), American Society of Anesthesiologists (ASA) physical status classification grade, past medical history, operation time, estimated blood loss (EBL), and history of previous lumbar spine surgery were collected. In addition, the diagnosis that led to the operation was classified as follows; adjacent segmental disease (ASD), scoliosis, multiple stenosis with/without sagittal deformity, and focal stenosis
When planning the ICRP approach for the upper lumbar spine, the extent of descent of the left costophrenic recess was evaluated using preoperative x-ray and computed tomography (CT) images. This evaluation was valuable because in patients in whom the OLIF L1/2/3 approach is obstructed by the ribs, the rib cage is located considerably downward, but the costophrenic recess rarely descends to the upper lumbar spine levels (Fig. 4).
The disc level of L1/2 or L2/3 was marked using the C-arm. The ribs were marked by palpation around the disc level. An incision of approximately 4 cm was made between the anterior and posterior axillary lines (Fig. 5A).
The subcutaneous skin, external intercostal muscles, internal intercostal muscles, innermost intercostal muscles, and diaphragm were exposed in sequence. This layer-by-layer approach involves spreading each muscle bundle. The diaphragm was incised to visualize the retroperitoneal fat (Fig. 5BŌĆōE). We should pay attention about the exposure of pleura in the space between the innermost intercostal muscles and diaphragm.
After retroperitoneal fat is retracted to the medial side, the psoas muscle is exposed. When the psoas muscle was retracted dorsally, the disc space was exposed. During this process, attention should be paid to the sympathetic chain, which is located close to the psoas muscle in the upper lumbar spine. When the path of the sympathetic chain overlapped with the annulotomy margin, the sympathetic chain was medially dissected and retracted (Fig. 5F). At this time, the commercially available OLIF25 retractor was inserted between the ribs (Fig. 5G). When the retractor was distracted between the ribs, sufficient fixation force was obtained without pinning (Fig. 5H).
After confirming the annulotomy margin through the C-arm, annulotomy, discectomy using a shaver, contralateral annulus release, trial placement, endplate preparation, and cage insertions were performed as in conventional OLIF [7,14]. The contralateral annulus release process requires attention. When a sharp device, such as a curette, enters deeply during the contralateral annulus release, it can cause damage to the renal vessels, since the kidneys are located on the right side of the upper lumbar spine (Fig. 4B, D).
We measured radiologic parameters using preoperative x-ray, intraoperative C-arm, postoperative 1-week x-ray, postoperative 1-week magnetic resonance (MR). Endplate injury was defined as any endplate disruption (> 1 mm) occurred in the postoperative MR T2 sagittal images (Fig. 6). We measured the depth of the endplate defect using postoperative MR T2 sagittal images.
The occurrence of pneumothorax and diaphragmatic herniation was evaluated using serial chest x-ray.
The rib line was defined as a line connecting the distal ends of ribs 10, 11, and 12 in the L-spine lateral image, and the level of the lumbar spine where this rib line crosses was measured (Fig. 4, red dotted line).
Among the continuous variables, age, operative time, and BMD were normally distributed (using the Shapiro-Wilk test), whereas length of hospital stay, BMI, and EBL were not. The independent T-test or Mann-Whitney test was performed to compare the 2 groups of continuous variables according to the normal distribution. Fisher exact test was used to compare categorical variables between the 2 groups. In addition, to measure the clinical changes after the active application of ICRP, the level of fusion and endplate injury between the previous period (2018ŌĆō2021) and 2022 were compared. All analyses were performed using IBM SPSS Statistics ver. 27.0 (IBM Co., Armonk, NY, USA).
A total of 121 patients underwent lateral interbody fusion of the upper lumbar spine. The conventional OLIF approach was employed in 99 patients (conventional group), and the ICRP approach was applied in 22 patients (ICRP group). OLIF at the L1/2 level was performed in 10 cases, and 2-level ICRP (L1/2/3) was performed in 2 cases (Fig. 2). There was no difference between the 2 groups regarding patientsŌĆÖ demographic characteristics such as BMI, BMD, ASA physical status classification grade, previous lumbar spine operation history, and disease entity (Table 1).
The ICRP group underwent longer-level fusion. Regarding surgical indications, multiple level stenosis with/without sagittal deformity was the most common (49 patients), followed by ASD according to the previous fusion (37 patients) (Table 1).
Endplate injury occurred in 34 of 99 patients (34.3%) in the conventional group and 2 of 22 (9.1%) patients in the ICRP group. There was a significant difference in the incidence of endplate injuries between the 2 groups (p = 0.020; odds ratio, 5.23). In the conventional group, the average endplate defect depth was 1.28┬▒ 2.20 mm, whereas that in the ICRP group was 0.27┬▒ 0.94 mm (p= 0.037) (Table 1).
When comparing the year 2022 (when ICRP was actively applied) and the previous period (2018ŌĆō2021), OLIF for L1/2/3 level was further increased among all OLIF patients. In 2022, the fusion level increased significantly, and OLIF was more applied even when the rib line was low. The endplate injury rate and endplate injury depth were partially reduced, but there was no statistical significance (Table 2).
The rib line was diversely distributed from the L1/2 disc space to the L3 vertebra; L2 vertebra - L2/3 disc level (80.2%), L1/2 disc level (9.9%), and L3 vertebra level (9.9%) (Table 1). When the rib line was high (L1/2 disc, L2 vertebra level), the conventional approach and ICRP showed no significant difference in endplate injury and endplate injury depth, but when the rib line was low (L2/3 disc, L3 vertebra level), ICRP was related with significantly lower endplate injury and endplate injury depth (Table 3).
Complications of the ICRP approach included 1 case of minimal endplate injury and 2 cases of transient sympathetic nerve injury. There was 1 case of pleura laceration and pneumothorax, which was described separately in the case. No other complications, including diaphragmatic hernia, rib fracture, contralateral root, vessel, or organ injury, were observed.
We encountered the first pneumothorax case (15th ICRP approach). L1ŌĆō5 OLIF was performed to correct degenerative scoliosis in a 74-year-old female patient. After conventional OLIF for L2/3/4/5, we could not access the L1/2 level because of lower ribs. In this case, the ICRP incision line was designed quite posteriorly (Fig. 7A). And during the dissection, we found one extra layer between innermost and diaphragm. This layer is tough, membrane-like layer without muscle (Fig. 7B, C). Postoperative chest CT showed pneumothorax (Fig. 7D, E). Since there was no lung or visceral pleura injury, it was absorbed naturally. We guess that the cause of the pneumothorax was the posterior location of the incision. Since the parietal pleura descends to the lower rib posteriorly, there is a risk of pneumothorax injury if the incision is designed posteriorly to the midaxillary line (Fig. 2).
The ICRP approach for upper lumbar spine OLIF has some advantages over the existing approach involving rib resection. Because the pleura is exposed at the posterior part of the lower rib, an incision between the anterior and posterior axillary lines can avoid exposure of the parietal pleura. In addition, the ICRP approach is free of rib resection-related complications. Since the commercial retractor can be fixed in the intercostal space without pinning, no risk of pin-site complications such as segmental vessel injury or ureter injury, is present. The most important advantage of ICRP is the lower risk of endplate injury because we can insert a surgical device parallel to the disc space.
We analyzed differences in surgical trends after use of ICRP by comparing 2022 and previous period (2018ŌĆō2021). Compared to the past, we performed L1/2/3 level surgery in much more cases in 2022. Even in the similar disease entity at the 2 timepoints, we believe that the difference in fusion level is due to following reasons; (1) In the past, when the rib line was low, we could not approach the upper lumbar spine; (2) The endplate was severely damaged when approaching excessively with the conventional approach; (3) With the development of ICRP, we can perform OLIF on the upper spine while reducing endplate injury even a lower rib line. Through these changes, we can reduce the back muscle injury, EBL, and additional time for posterior fusion of the upper lumbar spine. In addition, our experience showed that, through ICRP, even a spine surgeon who has no experience in chest wall surgery can easily extend the range of OLIF to the upper lumbar spine.
However, the ICRP approach requires an additional incision, which leads to prolonged surgical time. In this regard, if the rib line is higher than the L2/3 disc level, the conventional approach is preferred over the ICRP approach. If the rib line is L2/3 or lower, the ICRP approach is a good option (Table 3). We also noted that the ICRP approach may be difficult to perform in patients with large rib cages.
Unlike the conventional OLIF approach, the ICRP approach requires an understanding of 4 specific anatomical structures. First: intercostal muscle layers. Four layers of intercostal muscles were visualized during the ICRP approach: the external intercostal muscles, internal intercostal muscles, innermost intercostal muscles, and diaphragm. In the process of exposing each muscle layer, dissection too close to the inferior border of the rib may damage the intercostal nerves or vessels. If a structure other than the muscle layer is identified during the dissection process, determining whether air bubbles are formed after filling the operative corridor with saline is necessary. Second: sympathetic nerves. The thoracic sympathetic nerve descends below the diaphragm (at the L2 level) and becomes the abdominal sympathetic nerve, which is located at the anterior border of the psoas muscle at the L2 level. Going distally, it runs ventral (to the aorta) and away from the psoas muscle [24]. As shown in Fig. 5E, the sympathetic nerve is likely included in the range of annulotomy at L1/2 or L2/3. In such cases, sufficient medial retraction of the sympathetic nerve is necessary before annulotomy. Third: contralateral vessels and organs. As shown in Fig. 4, the L1/2 or 2/3 level is close to the right kidney or renal vessel. Hence, careful maneuvering during contralateral annulus release is advisable. In particular, the use of a blunt device, rather than a sharp one (such as a curette), is recommended for annulotomy. We should also avoid inserting these devices too deep. Finally: rib line and parietal pleura. Every patient has a considerably different rib line due to thoracic kyphosis, and aging [20,25]. However, the costophrenic recess is constantly positioned irrespective of the rib line. The parietal pleura descends to the 12th rib in the midscapular line, 10th rib in the midaxillary line, and 8th rib in the midclavicular line [21]. Therefore, the lateral minimal incision is less likely to expose the parietal pleura than an incision extending posteriorly (Fig. 2). However, serial followup chest x-rays are required to evaluate minor injuries of the parietal pleura that are not recognized during surgery.
This study had several limitations. First, selection bias inevitably existed in patients who chose the conventional and ICRP approaches. However, in our study, ICRP was performed in patients with a lower rib line. The selection bias was more unfavorable for ICRP, yet it presented better results. Second, our study did not describe the clinical outcomes. This is because most of the enrolled patients underwent multisegment surgery for different disease entities, and a simple comparison of clinical results is not meaningful. Third, the fusion rate was not evaluated in our study because we did not have long-term follow-up data, and no follow-up CT evaluations were performed. However, this study focused on the introduction of a new surgical technique and its short-term complications. In addition, we assumed that this approach may have little effect on the fusion rate because ICRP does not require rib resection and has a lower incidence of endplate injury. Fourth, we evaluated endplate injury by MR rather than x-ray. As shown in Fig. 5A, it is difficult to evaluate endplate injury at all levels in patients with scoliosis using only L-spine x-ray lateral images. Therefore, we measured the presence and depth of endplate injury using postoperative MR T2 sagittal images. For this reason, the endplate injury rate was significantly higher than that of previous OLIF endplate injury related studies [26,27].
The ICRP approach is effective in reducing the incidence of endplate injuries in patients with a relatively low rib line. In addition, this approach has the advantage of a smaller incision, without pleural exposure or rib resection, compared to the conventional upper lumbar spine approach. However, the possible risks of sympathetic nerve and contralateral side injuries should be considered.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.2244960.480.
NOTES
Fig.┬Ā1.
Upper lumbar spine approach for lower rib line. (A, B) Intraoperative anteroposterior, lateral images; even with sufficient jack-knife position, the Penfield dissector cannot be parallel to the L2/3 disc space. (C) An immediate postoperative x-ray image: severe endplate injury of L2 lower endplate. (D) Computed tomography image taken 6 months postoperatively: severe subsidence and resulting gap between the cage and L3 upper endplate.

Fig.┬Ā2.
Computed tomography chest reconstruction image: The positional relationship between ribs and parietal pleura (blue). (A) Posterior view: the parietal pleura descends to the 12th rib at the midscapular line (red arrow). (B) Left lateral view: the parietal pleura descends to the 10th rib at the midaxillary line (red arrow). The distal portion of the 10th to 12th ribs (white square) does not expose the parietal pleura.
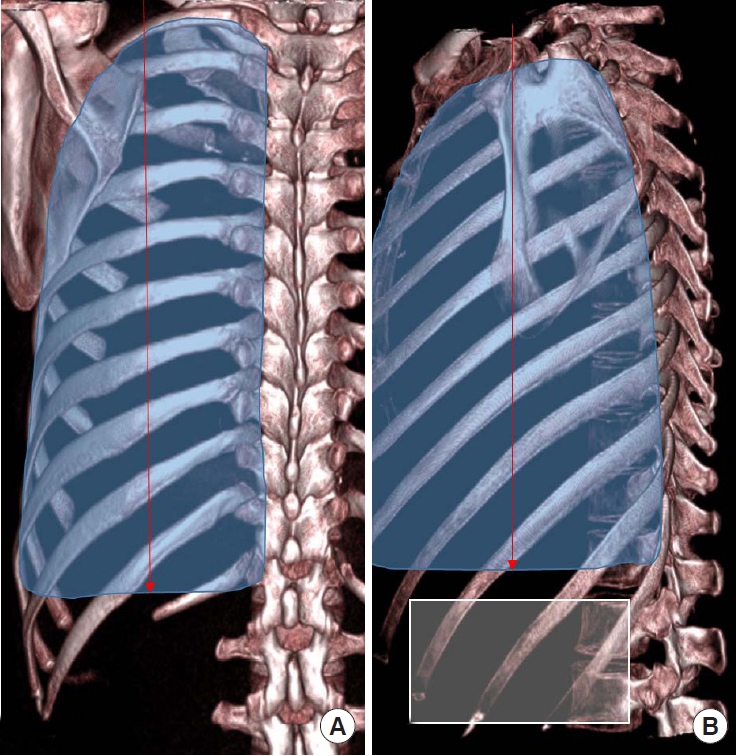
Fig.┬Ā3.
Diagram of inclusion/exclusion. OLIF, oblique lumbar interbody fusion; ICRP, intercostal retroperitoneal approach.
*Among the 3 patients, 2 patients was underwent 2-level ICRP (L1/2/3).
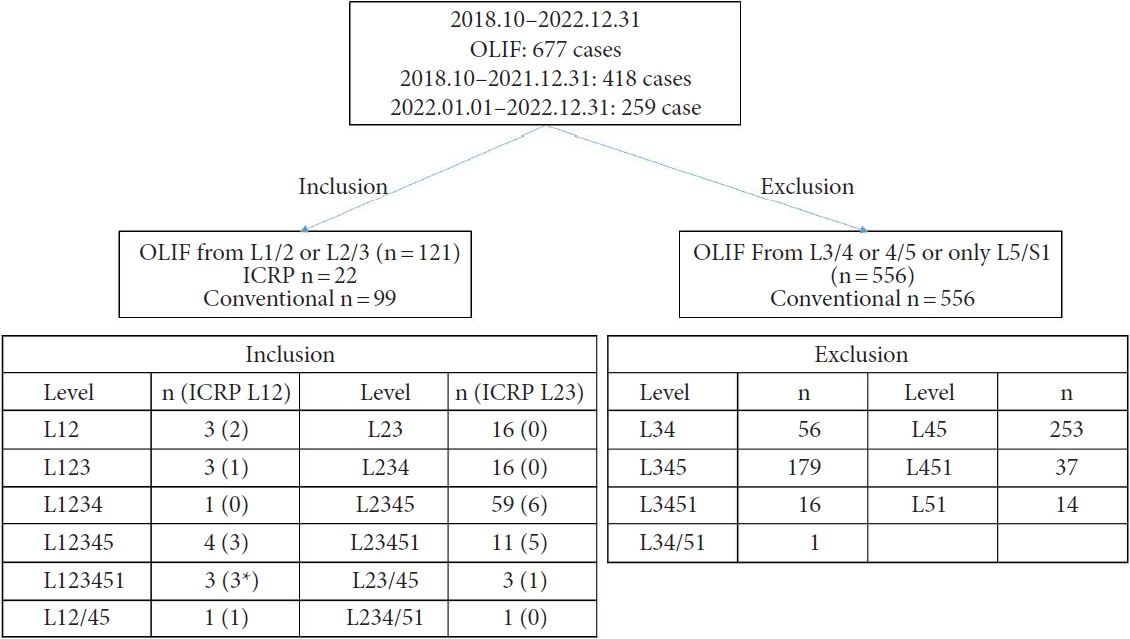
Fig.┬Ā4.
Differences in operative corridor according to the rib line. (A, B) Upper rib line: (A) The rib line crossed L2 body; (B) No rib is identified at L2/3 disc level and the surgical corridor (conventional OLIF approach can be achieved). (C, D) Lower rib line: (C) The rib line crossed L3 body; (D) At L2/3 level, 11th and 12th ribs are identified, and the pleural cavity is not identified between the ribs (require intercostal retroperitoneal approach). (B, D) The kidney, ureter, and renal vessels are located on the right side of the disc space.
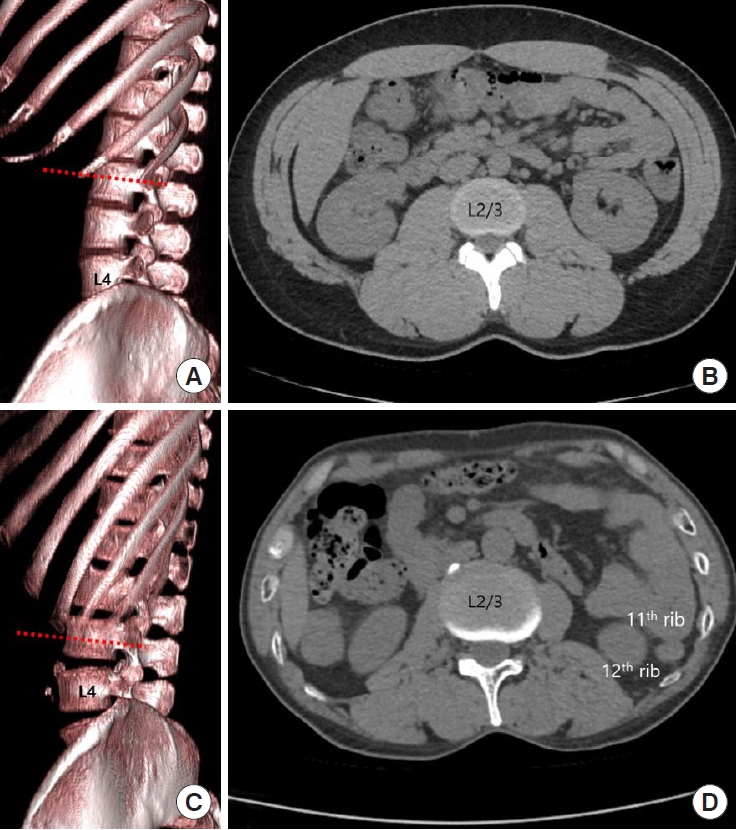
Fig.┬Ā5.
Mini-open intercostal retroperitoneal approach. (A) Incision line (red dot line) is designed at the inter\costal space; 3-dimensional reconstruction image indicates L2/3 disc space is identified between ribs. (B-E) Dissection of the chest wall: (B) External intercostal muscles; (C) Internal intercostal muscles; (D) Innermost intercostal muscles; and (E) Diaphragm are identified, and the pleura is not exposed. Opening this layer exposes the retroperitoneal space. The white arrow indicates the direction of the muscle bundle. (F) The sympathetic nerve is directly anterior to the psoas muscle. The blue arrow indicates the direction of retraction. Dissection and retraction of the psoas muscle to the dorsal side and the sympathetic nerve to the ventral side. (G) The retractor is mounted at L2/3 disc space. (H) The positional relationship between the retractor and the rib, when the retractor is distracted, the operative corridor between the ribs is widened and the retractor can be fixed without pinning. The blue arrow indicates the distraction force of retractor. The red line indicates the rib.

Fig.┬Ā6.
Measurement of endplate injury. (A) X ray image: endplate injury at L3/4 (red arrow), but no endplate injury at the L4/5 level (white arrow). (B) Magnetic resonance image: L3/4 (red arrow), 4/5 (white arrow) both levels show endplate injury.
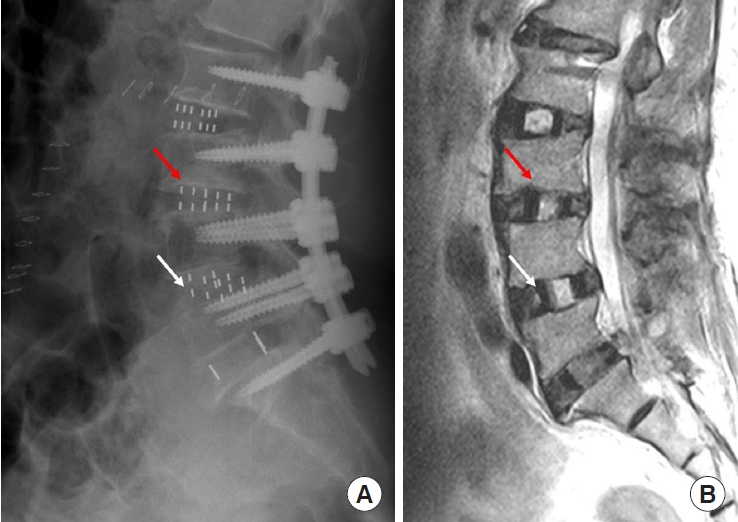
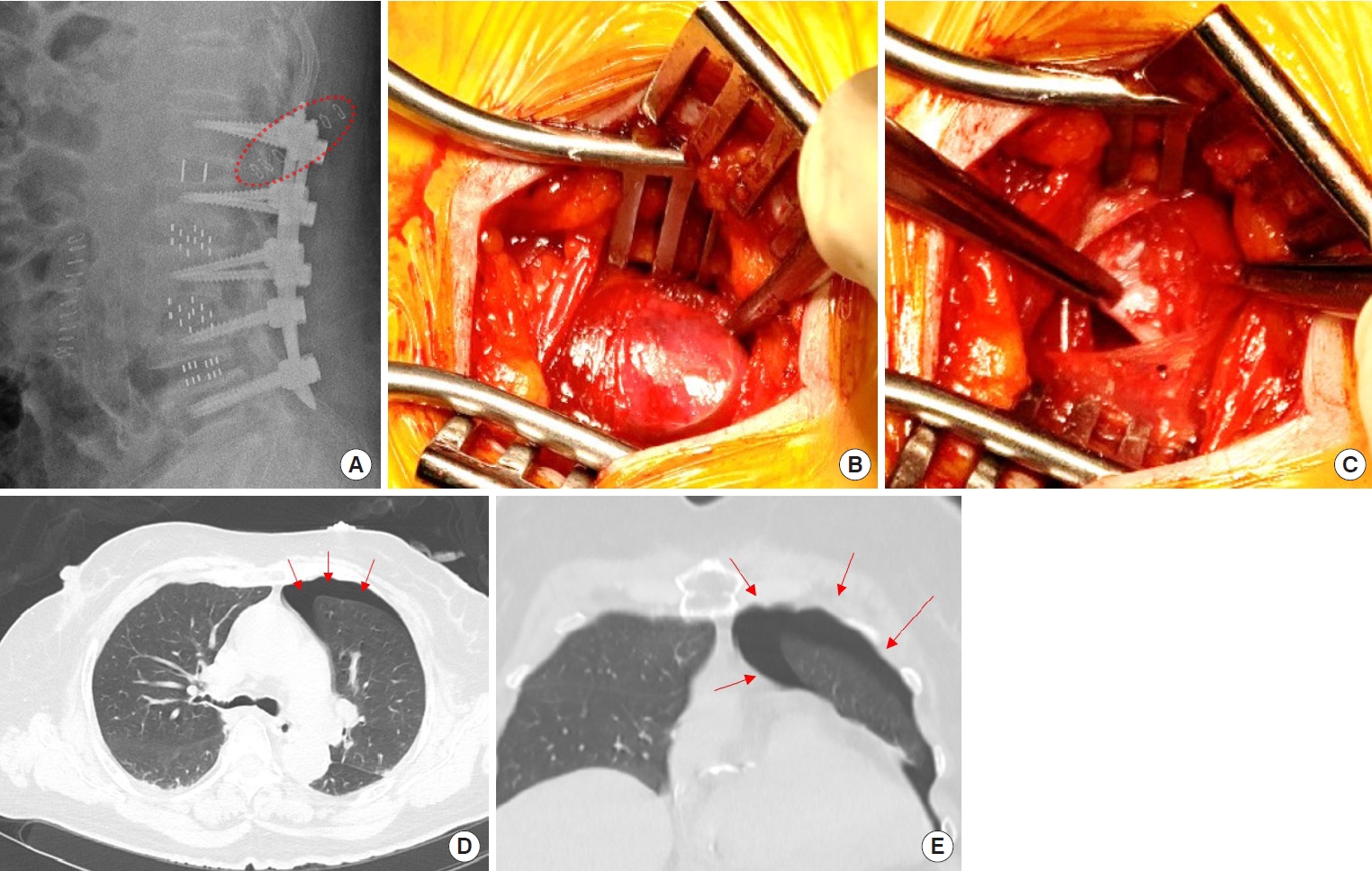
Fig.┬Ā7.
Case illustration of pneumothorax. (A) Conventional OLIF L2/3/4/5 and ICRP L1/2 was performed. Red dotted line indicates incision line of ICRP. (B, C) Extralayer between innermost intercostal muscle and diaphragm. (D, E) Postoperative chest computed tomography, pneumothorax (red arrows). OLIF, oblique lumbar interbody fusion; ICRP, intercostal retroperitoneal approach.
Table┬Ā1.
Operative details
Table┬Ā2.
Comparison of endplate injury and subsidence according to period
Table┬Ā3.
Endplate injury incidence according to rib line and different approach
| Rib line |
ICRP |
Conventional |
p-value (ICRP vs. conventional) |
|||
|---|---|---|---|---|---|---|
| Endplate, injury/total | Endplate injury depth (mm) | Endplate, injury/total | Endplate injury depth (mm) | Endplate injury | Endplate depthŌĆĀ | |
| L1/2 | 0/2 (0) | 0 (0) | 2/10 (20.0) | 0.60 ┬▒ 1.35 | 0.188 | 0.112 |
| L2 | 0/7 (0) | 0 (0) | 12/51 (23.5) | 0.67 ┬▒ 1.63 | ||
| L2/3 | 1/6 (16.7) | 0.33 ┬▒ 0.82 | 17/33(51.5) | 2.15 ┬▒ 2.62 | 0.025 | 0.016 |
| L3 | 1/7 (14.3) | 0.57 ┬▒ 1.51 | 3/5 (60) | 3.20 ┬▒ 3.03 | ||
| Total | 2/22 (9.1) | 0.27 ┬▒ 0.94 | 34/99 (34.3) | 1.28 ┬▒ 2.20 | 0.020 | 0.020 |
REFERENCES
1. Kim H, Chang BS, Chang SY. Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine 2022;19:163-76.




2. Mehren C, Mayer HM, Zandanell C, et al. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res 2016;474:2020-7.




3. Davis TT, Hynes RA, Fung DA, et al. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 2014;21:785-93.


4. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 2017;17:545-53.


5. Yingsakmongkol W, Jitpakdee K, Kerr S, et al. Successful criteria for indirect decompression with lateral lumbar interbody fusion. Neurospine 2022;19:805-15.




6. Xie T, Pu L, Zhao L, et al. Influence of coronal-morphology of endplate and intervertebral space to cage subsidence and fusion following oblique lumbar interbody fusion. BMC Musculoskelet Disord 2022;23:633.




7. Woo JB, Son DW, Lee SH, et al. Which factor can predict the effect of indirect decompression using oblique lumbar interbody fusion? Medicine (Baltimore) 2022;101:e29948.



8. Park SJ, Hwang JM, Cho DC, et al. Indirect decompression using oblique lumbar interbody fusion revision surgery following previous posterior decompression: comparison of clinical and radiologic outcomes between direct and indirect decompression revision surgery. Neurospine 2022;19:544-54.




9. Lee YS, Lee DH, Cho DC, et al. The change of spinal canal according to oblique lumbar interbody fusion in degenerative spondylolisthesis: a prospective observational study. Neurospine 2022;19:492-500.




10. Shimizu T, Fujibayashi S, Otsuki B, et al. Indirect decompression with lateral interbody fusion for severe degenerative lumbar spinal stenosis: minimum 1-year MRI follow-up. J Neurosurg Spine 2020 Mar 13:1-8. doi: 10.3171/2020.1.SPINE 191412. [Epub].

11. Zakaria AF, Kaneko S, Takeda H, et al. Circumferential bone fusion in adult spinal deformity via combination of oblique lateral interbody fusion and grade 2 posterior column osteotomy. Global Spine J 2022 Jan 21:21925682211069936. doi: 10.1177/21925682211069936. [Epub].


12. Jo DJ, Seo EM. Efficacy and radiographic analysis of oblique lumbar interbody fusion in treating adult spinal deformity. PLoS One 2021;16:e0257316.



13. Park SW, Ko MJ, Kim YB, et al. Correction of marked sagittal deformity with circumferential minimally invasive surgery using oblique lateral interbody fusion in adult spinal deformity. J Orthop Surg Res 2020;15:13.




14. Oh BK, Son DW, Lee SH, et al. Learning curve and complications experience of oblique lateral interbody fusion : a single-center 143 consecutive cases. J Korean Neurosurg Soc 2021;64:447-59.




15. Grin AA, Kordonskiy AY, Lvov IS, et al. Lateral retropleural and retrodiaphragmatic approach in patients with spine trauma and diseases: a systematic review and meta-analysis. Zh Vopr Neirokhir Im N N Burdenko 2021;85:94-103.

16. Litre CF, Duntze J, Benhima Y, et al. Anterior minimally invasive extrapleural retroperitoneal approach to the thoracolumbar junction of the spine. Orthop Traumatol Surg Res 2013;99:94-8.


17. Uribe JS, Dakwar E, Cardona RF, et al. Minimally invasive lateral retropleural thoracolumbar approach: cadaveric feasibility study and report of 4 clinical cases. Neurosurgery 2011;68(1 Suppl Operative):32-9. discussion 39.



18. Gumbs AA, Bloom ND, Bitan FD, et al. Open anterior approaches for lumbar spine procedures. Am J Surg 2007;194:98-102.


19. Kim M, Nolan P, Finkelstein JA. Evaluation of 11th rib extrapleural-retroperitoneal approach to the thoracolumbar junction. Technical note. J Neurosurg 2000;93:168-74.

20. Mitsui T, Shimizu T, Fujibayashi S, et al. Predictors of the need for rib resection in minimally invasive retroperitoneal approach for oblique lateral interbody fusion at upper lumbar spine (L1-2 and L2-3). J Orthop Sci 2022 Jul 5:S0949-2658(22)00173-7. doi: 10.1016/j.jos.2022.06.008. [Epub].

21. Smith SE, Darling GE. Surface anatomy and surface landmarks for thoracic surgery: Part II. Thorac Surg Clin 2011;21:139-55, vii.


22. Eroglu M, Guvence N, Kiper A, et al. Rib resection for livedonor nephrectomy. Int Urol Nephrol 2005;37:675-9.



23. Srivastava A, Tripathi DM, Zaman W, et al. Subcostal versus transcostal mini donor nephrectomy: is rib resection responsible for pain related donor morbidity. J Urol 2003;170:738-40.


24. Mahatthanatrakul A, Itthipanichpong T, Ratanakornphan C, et al. Relation of lumbar sympathetic chain to the open corridor of retroperitoneal oblique approach to lumbar spine: an MRI study. Eur Spine J 2019;28:829-34.



25. Joshua A, Shetty L, Pare V. Variations in dimensions and shape of thoracic cage with aging: an anatomical review. Anat J Afr 2014;3:346-55.




























