INTRODUCTION
The vacuum disc phenomenon, known as a presence of gas in the intervertebral disc space, is a relatively common radiological finding, especially on computed tomography (CT) finding1,6,8). Gas production in the intervertebral disc space canoccur as a result of disc degeneration. Although its clinical importance is low, sometimes it can cause different clinical pattern12). Patients with epidural gas may complain of low back or radicular pain due to compression of the dural sac and nerve root4).
The clinical symptoms are similar to those of common sciatica, with radicular pain and positive straight leg-raising test2,17).
We recently experienced two cases with an unusual significance, that is lumbosacral radiculopathy resulting from epidural gas containing cyst. It is suspected to be formed in the degenerative disc and presumably released into epidural space through the tears of annulus fibrosus.
CASE REPORT
Case 1
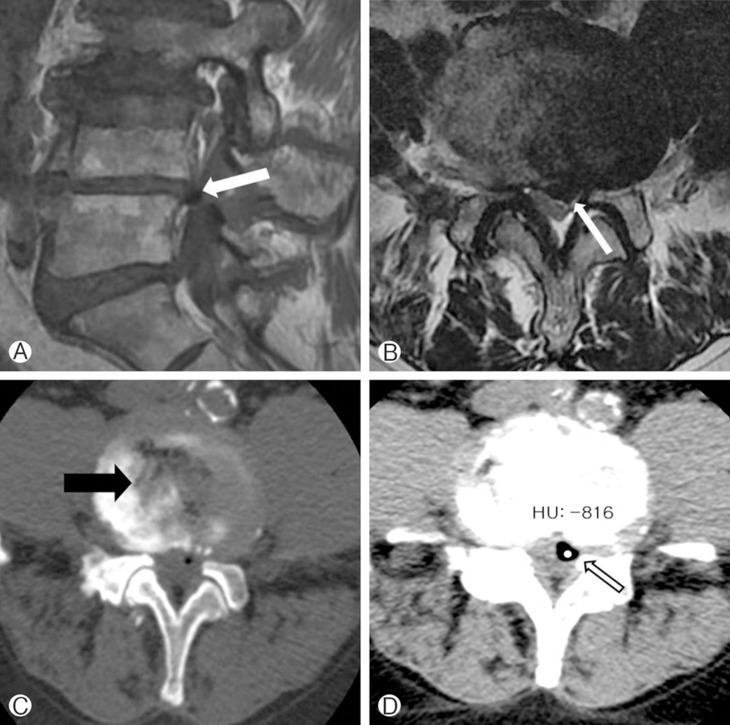
A 83-year-old man with a 8-week history of back and left radiating pain was admitted to our clinic. The pain was localized to left L-5 dermatome and there was no motor dysfunction. The MRI revealed marked disc space narrowing, and a lesion of low signal intensity on both T1- and T2-weighted images, consistent with gas formation or calcification. Axial CT showed marked L4-5 vacuum disc phenomenon, and a gas-containing cyst located at posterolateral aspect of the spinal canal was observed at the same level. Hounsfield unit of the cyst was -816, which corresponds to air. During the partial hemilaminectomy, this gas-containing cyst was actually a bluish colored sac which was not communicated to disc space, and there was no evidence of disc extrusion in neural foramen; this lesion was removed via subtotal resection of the capsule microsurgically. His symptoms improved after the surgery and he didn't have any remarkable complaints during a 6 month follow-up.
Case 2
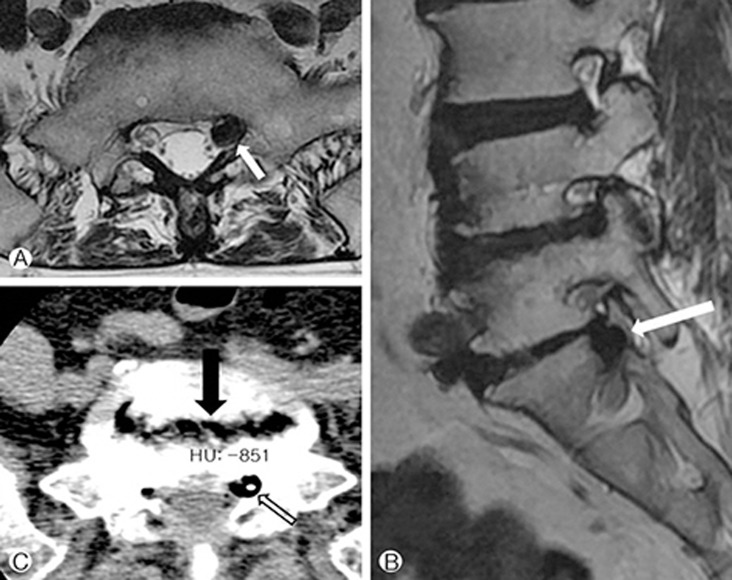
A 72-year-old woman presented with last 1-month history of pain in the left lower extremity, which radiated to the buttock, lateral aspect of the upper thigh, and the posterior calf. Symptoms were aggravated by standing and walking, and were improved by sitting position. There was no history of any invasive procedure such as surgery, lumbar puncture, or epidural injection. Her straight leg-raising test was negative and there was no motor dysfunction. MR imaging showed a well-encapsulated low signal intensity lesion was compatible with a gas formation or calcification. Axial CT revealed vacuum disc phenomenon at L5-S1 level, and intracannular posterolateral gas collection at the same level. Hounsfield unit of the lesion was measured as -851. The patient underwent laminectomy and the left L5-S1 discectomy. During the surgery, compression of the left S1 nerve root by a gas-containing cyst was observed. Needle puncture of the gas-containing cyst with subtotal excision of the wall was performed. After the surgery, the radicular symptom was improved significantly. The patient showed no recurrence of complaint at 1-year follow up evaluation.
DISCUSSION
Vacuum disc phenomenon is the a radiographic finding which was formed by gas formation, especially in degenerated intervetebral disc15,18). Also it has been associated with infection, invasive procedures and trauma. Fick5) reported this phenomenon in 1904 and Larde et al.12) described the presence of free intraspinal gas, seen in 46% cases on CT examination. Vacuum phenomenon is caused by the liberation of gas, composed of nitrogen and carbon dioxide, in the disc as it degenerates9,18). If annulus fibrosus tears, the air can be released and collected in the epidural space. Although it is well recognized that epidural gas is usually present in asymptomatic patients, in rare instances, it can illicit lumbosacral radiculopathy. The report by Gulati and Weinstein6) described the presence of free epidural gas, 3 of 79 symptomatic patients with spinal steno sis on CT images, who also had vacuum disc phenomenon.
The vacuum phenomenon is recognized on CT as low density areas in the region of the intervertebral disc and is typically acquired Hounsfield unit numbers of less than zero. Also, associated findings include osteophytes of adjacent vertebral bodies and degeneration of discs including bulging or herniation. In some reports, CT myelography is considered to be a gold standard for demonstrating epidural space pathology10,19).
MR imaging is a good modality for evaluation of the interver tebral disc, the spinal cord and nerve roots which may be influenced by degeneration. On MR images, gas is a low signal intensity on T1 and T2-weighted images. Because calcification also marks a low signal intensity similar to that of the gas, it is difficult to distinguish each other. In our cases, MR images showed an epidural space occupying lesion, suggesting the presence of air or calcified disc cause lumbosacral radiculopathy.
Our patients had not undergone any invasive procedures such as epidural or nerve root block, so the source of epidural gas was speculated from the vacuum disc through tear of annulus fibrosus. In accordance with the previous studies and based on our findings on CT and MR, we thought that gas was originated from degenerative vacuum disc. The first patient showed an unusual finding of a gas formation with a left paracentral gas-containing cystic lesion on the radiological findings. During microscopic surgery, we could confirm the gas-containing cyst surrounded by the thin walled capsule and it was removed microsurgically. The second patient showed a gas-containing cyst in the foramen of S1 root and we couldn't find a ruptured disc herniation on the operation field.
Motion of the lumbar spine increases migration of gas into the epidural space by imposing excessive pressure20). The mechanism of root compression was thought to be a valve pump-like pneumatic compression in the gaseous intervertebral disc, that is, squeezing air out into a well-encapsulated sac especially when the patient was in upright position3). This theory is supported by the fact that flexion position may cause disappearance of the gas in lumbar lateral X-ray and improve symptoms because the compression was resolved, allowing air to return to the disc space.
Because gas in the epidural space may usually disappear spontaneously in patients with neurologic symptoms, conservative treatment and a period of observation should be warranted13). And a low resistance of epidural space may make gas bubbles spread into multiple vertebral levels rather than forming a single larger gas formation. Raynor et al.14) reported one case of a symptomatic postoperative gas bubble after performing microdiscectomy, which caused a foot drop 10 days after the surgery. This patient's symptom was improved after 10 days of oral steroid therapy. The follow-up MRI revealed complete resolution of the gas-containing cyst after 6 weeks. So, nonsteroid anti-inflammatory drugs, muscle relaxants, and epidural steroid injection or aspiration of gas under fluoroscope have been reported as alternative treatment options16).
In our patients, oral steroids and expectant observation did not resolve symptoms, and we cannot become assured for the spontaneous absorption of gas because in our cases gas was encapsulated so that surgery was performed.
CONCLUSION
We have presented two cases with regard to the rare occurrence of air within the epidural space, causing nerve root compression For those patients with gas accumulation in the spinal canal without history of any invasive procedures, this report is intended to alert clinicians the existence of this entity and assist in diagnosis of similar cases.