|
 |
- Search
Abstract
Objective
The purpose of this study is to evaluate the efficacy of laminoplasty in the treatment of spinal cord injury (SCI) without instability.
Methods
79 patients with SCI without instability who underwent surgical treatment in our institute between January 2005 and September 2012 were retrospectively reviewed. Twenty nine patients fulfilled the inclusion criteria as follows: SCI without instability, spinal cord contusion in MRI, cervical stenosis more than 20%, follow up at least 6 months. Preoperative neurological state, clinical outcome and neurological function was measured using the American Spinal Injury Association (ASIA) impairment scale, modified Japanese Orthopedic Association (mJOA) grading scale and Hirabayashi recovering rate.
Results
Seventeen patients showed improvement in ASIA grade and twenty six patients showed improvement in mJOA scale at 6 month follow up. However, all patients with ASIA grade B and C have shown improvement of one or more ASIA grade. Mean Hirabayashi recovery rate was 47.4±23.7%. There was better neurologic recovery in those who had cervical spondylosis without ossification of posterior longitudinal ligament (OPLL) (p<0.05, χ2 test).
Conclusions
It is different in B, C, D with ASIA A that there are debates going on about the application of surgical treatment in ASIA A, and surgical treatment is helpful in B, C, D since it contributes to neurologic improvement. We concluded that laminoplasty provided good neurologic recovery in SCI without instability that cervical canal stenosis, especially spondylosis without OPLL and neurologic deterioration in ASIA B, C and D.
Spinal cord injury (SCI) is a devastating event for the patient and family. The patient may result in permanent disability and the socio-economic impact is a tremendous total.
In the acute post-injury phase, intensive hemodynamic monitoring and critical care management is very important17,25,27,30). The treatment of SCI without instability such as fracture, dislocation and ligament injury, however, remains controversial.
Additionally, the role and timing of surgical treatment in SCI without instability was debated in several literatures. Mirza et al,reported that stabilization within 72 hr of injury in cervical spine injured patients is sufficient to improve neurological outcome23). Other investigators have also reported spontaneous neurological recovery in the conservatively managed group3,4,28). However, neural compressions by stenotic lesions may warrant surgical interventions to improve paralysis in acute stage. Laminoplasty has been widely accepted as a reasonable option to treat multilevel pathology of the cervical spine, such as OPLL and cervical spondylotic myelopathy (CSM). It permits adequate decompression of the cervical spinal cord and is safe and easily performed16,20,21). The purpose of our study was to evaluate the efficacy of laminoplasty in the treatment of SCI without instability.
We retrospectively reviewed the medical records of 79 patients with SCI without instability who underwent surgical treatment in our institute between January 2005 and September 2012. Twenty nine patients (36.7%) fulfilled the inclusion criteria as follows: SCI without instability, spinal cord contusion in MRI, cervical stenosis more than 20%, follow up at least 6 months. The spinal cord diameter was measured according to previous authors19),
where A is the diameter of the cervical cord at the injured level and B is the diameter of the cervical cord at the non-compression level. Exclusion criteria is existence of instability or kyphosis. Cervical spine instability is defined as the loss of ability of cervical spine under physiological loads. Instability was judged by destruction or loss of function of anterior or posterior elements, relative translation of vertebra in sagittal plane higher than 3.5mm and angulation higher than 11 degrees. The degree of cervical instability was assessed by plain film, stress view(flexion and extension), computed tomography (CT) and magnetic resonance image (MRI). There were 26 males and 3 females ranging in age from 31 to 73 years old (mean age 57) (Table 1).
The patients sustained by several different causes of injuries from motor vehicle accident, fall-down and slip down. Preoperative neurological state, clinical outcome and neurological function was measured using the ASIA impairment scale, mJOA grading scale and Hirabayashi recovering rate. Those assessments were made at admission and at 6 month follow-up after surgery.
Statistical analyses were performed using SPSS statistic software (18.0 K). A p-values were generated using Fisher exact test and repeated measures ANOVA. A p-value of less than 0.05 was considered statistically significant.
On admission, preoperative ASIA grades were A in 3, B in 7, C in 9 and D in 10 patients. One patient had both leg weakness with cervical spondylosis before the trauma and the others had no neurologic deficits. Overall pre- and postoperative neurologic status are summarized in Table 2. Preoperative mJOA scale ranged 0 to 16 (Mean=8.1±5.3) and postoperative mJOA scale ranged 0 to 18 (Mean=12.1±5.2). Twenty six patients (89.6%) showed improvement in mJOA scale at 6 months follow up. There was statistically significant in improvement of mJOA scale (p<0.05, Repeated measures ANOVA).
Seventeen patients (58.6%) showed improvement in ASIA grade at 6 months follow up and especially all patients with ASIA grade B and C have shown improvement of one or more ASIA grade (Table 3).
All patients had pre-existing lesion such as degenerative cervical spondylosis or OPLL. Presence of OPLL was confirmed using CT and, especially, type of OPLL was classified on CT sagittal view. This can be seen as areas of ossification behind the cervical vertebral bodies. 21 patients had degenerative cervical spondylosis without OPLL and 8 patients had OPLL. There was better neurologic recovery in those who had cervical spondylosis without OPLL before injury than OPLL (p<0.05) (Fig. 1).
We stratified the patients into two groups according to timing of operative intervention. The early surgical group consisted of 25 patients who underwent surgery within 24 hours of injury. Four patients in the delayed surgical group underwent surgery after 24 hours. The causes of delayed operation were unstable vital sign (1 patient) and hospital visiting over 24 hours (3 patients) after trauma. No significant difference was noted in neurologic improvement between the early surgical group and delayed surgical group (p>0.05).
Mean Hirabayashi recovery rate was 47.4±23.7%. Good neurologic outcome also was noted at short segment (2 and 3 levels) laminoplasty in Hirabayashi recovery rate. Hirabayashi recovery rate in 2 and 3 levels laminoplasty group were 66.7% and 49.4%. However it had no statistical significance.
In this study, 20 patients had spinal cord compression rate, lesser than 50% and 9 patients' rate was greater than 50%. A group with compression rate, lesser than 50% showed better neurologic outcome, however, it did not statistical significance (p>0.05) (Fig. 2).
There was no severe postoperative complication but exist some of axial neck pain complaint.
Two major mechanism of spinal cord injury with the neurologic deficits, primary and secondary injuries, are accepted widely1,26). The primary mechanism results from an insult that occurs at the time of impact, such compression, distraction, laceration, or shear, which are not amenable to therapy. The secondary injuries, including edema, inflammation, or ischemia, provide a therapeutic window of opportunity for intervention2,12).
Although there has been neurological improvement shown with early decompression in animal models6,10), clinical studies on surgical results remain controversial. Various investigators have reported spontaneous neurological recovery in the conservatively managed group3,4,28) and conservative treatment remains a good option for patients with incomplete cervical cord injuries18). Kawano et al. reported that surgical treatment was not found to be superior to conservative treatment for cervical spinal cord injury (ASIA B, C) patients without bone and ligament injury in the acute phase19). Therefore some spine surgeons adopted conservative approach. However, the others asserted that operative intervention provided statistically better motor recovery than did conservative therapy5,7). In this study, although not compared with conservative treatment, we concluded that surgical intervention, especially laminoplasty, provided good neurologic recovery in SCI without instability.
Some investigators have reported surgical outcome excluded ASIA A and D patients. The reason of exclusion was that many patients with ASIA A were in very poor general condition and either patients with ASIA A or D did not show significant neurologic outcome after surgery. However, in present study, patients with ASIA A and D were included because of presences of cervical cord compressed lesions and contusion. Nevertheless, there were no neurologic recovery in ASIA A and small degree of neurologic recovery in ASIA D. Therefore, surgical treatment might be required in ASIA D, since there was neurologic improvement in some way. However, in ASIA A, it is difficult to make conclusion that it is justifiable to apply surgical treatment since there was no significant neurologic improvement.
The degree of spinal canal stenosis did not affected patients' recovery rate in this study. Although good neurologic outcome showed at lesser than 50% cord compression rate, neurologic outcome according to the degree of cervical stenosis was no significant statistically difference (p>0.05). However, Yoo et al reported neurologic deterioration after trauma and outcome after surgery depended on the diameter of the residual spinal canal29).
Chikuda, et al. reported better neurological outcome in patients with gait disturbance before injury when they compared surgery and conservative treatment for traumatic cervical spinal cord injury associated with OPLL9). However, they noted no statistical difference between surgery and conservative treatment9). One meaningful result in this study is that there was better neurologic recovery in those who had cervical spondylosis without OPLL before injury than others (p<0.05, χ2 test). Although most patients had no neurologic deficits before the trauma, we considered that patients with OPLL had more compressed and vulnerable cord than spondylosis without OPLL. Therefore, patients with OPLL had more neurologic deficits at the time of injury, relatively.
The decompression surgery was anterior approach, posterior approach or both. Fessler et al. reported anterior decompression and fusion provided symptom improvement for CSM15). Edwards et al. reported improvement of neurologic symptoms after laminoplasty11). The method of surgical intervention was decided based on pathologic lesion location, range, comorbidity, patient conditions, and operator's favor. Open-door expansile cervical laminoplasty (ODECL) is an effective surgical technique in the treatment of multilevel CSM16,20,21). This technique was used in multilevel stenosis, no sagittal malalignment and no kyphotic deformities. Laminoplasty may be simpler, more rapid procedure and more effective decompression of cervical spinal canal than anterior decompression in multilevel stenosis. Therefore, we used this laminoplasty in SCI without instability for better neurologic outcome than conservative treatment.
The optimal timing of surgical intervention for spinal cord injury (SCI) remains controversial. Early spinal surgery (within 72 hr after injury) was associated with shorter length of stay and reduced pulmonary complications, however, no differences in neurologic or functional improvements were noted compared with late surgical groups22). On the other hand, someone argued early decompression (<24 hr) should be considered as part of the therapeutic management of any patient with SCI, particularly those with cervical SCI13,14,23,24). In our study, no significant difference was noted in neurologic improvement between the early surgical group (<24 hr) and delayed surgical group (>24 hr) (p>0.05).
Limitation of this study was that there was non-randomized study, bias inherent to retrospective chart reviews, short follow-up period and small sample size. The length of follow up period was less than 1 year in some patients. However, we observed patients' status minimum 6 months, because the neurologic recovery in terms of JOA scores improved after surgical decompression, reached statistical significance at 3 month and reached a plateau at 6 month 8.
It is different in B, C, D with ASIA A that there are debates going on about the application of surgical treatment in ASIA A, and surgical treatment is helpful in B, C, D since it contributes to neurologic improvement. We concluded that laminoplasty provided good neurologic recovery in SCI without instability that cervical canal stenosis, especially cervical spondylosis without OPLL and neurologic deterioration in ASIA B, C and D.
References
1. Amar AP, Levy ML. Pathogenesis and pharmacological strategies for mitigating secondary damage in acute spinal cord injury. Neurosurgery 1999 44:1027. -1039. discussion 1039-1040. PMID: 10232536.


2. Anderson DK, Hall ED. Pathophysiology of spinal cord trauma. Ann Emerg Med 1993 22:987-992. PMID: 8503537.


3. Bedbrook GM. Spinal injuries with tetraplegia and paraplegia. J Bone Joint Surg Br 1979 61-B:267-284. PMID: 225332.


4. Bedbrook GM, Sakae T. A review of cervical spine injuries with neurological dysfunction. Paraplegia 1982 20:321-333. PMID: 7162842.


5. Bose B, Northrup BE, Osterholm JL, Cotler JM, DiTunno JF. Reanalysis of central cervical cord injury management. Neurosurgery 1984 15:367-372. PMID: 6483151.


6. Carlson GD, Gorden CD, Oliff HS, Pillai JJ, LaManna JC. Sustained spinal cord compression: part I: time-dependent effect on long-term pathophysiology. J Bone Joint Surg Am 2003 85-A:86-94. PMID: 12533577.

7. Chen TY, Dickman CA, Eleraky M, Sonntag VK. The role of decompression for acute incomplete cervical spinal cord injury in cervical spondylosis. Spine (Phila Pa 1976) 1998 23:2398-2403. PMID: 9836353.


8. Cheung WY, Arvinte D, Wong YW, Luk KD, Cheung KM. Neurological recovery after surgical decompression in patients with cervical spondylotic myelopathy - a prospective study. Int Orthop 2008 32:273-278. PMID: 17235616.


9. Chikuda H, Seichi A, Takeshita K, Matsunaga S, Watanabe M, Nakagawa Y, et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine (Phila Pa 1976) 2011 36:1453-1458. PMID: 21240049.


10. Dimar JR 2nd, Glassman SD, Raque GH, Zhang YP, Shields CB, et al. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976) 1999 24:1623-1633. PMID: 10472095.


11. Edwards CC 2nd, Heller JG, Silcox DH 3rd, et al. T-Saw laminoplasty for the management of cervical spondylotic myelopathy: clinical and radiographic outcome. Spine (Phila Pa 1976) 2000 25:1788-1794. PMID: 10888947.


12. Faden AI. Experimental neurobiology of central nervous system trauma. Crit Rev Neurobiol 1993 7:175-186. PMID: 8221911.

13. Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976) 2010 35:S166-S173. PMID: 20881458.


14. Fehlings MG, Vaccaro A, Wilson JR, Singh A, W Cadotte D, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One 2012 7:e32037PMID: 22384132.



15. Fessler RG, Steck JC, Giovanini MA. Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery 1998 43:257. -265. discussion 265-257. PMID: 9696078.


16. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976) 1988 13:870-876. PMID: 3143157.


17. Hovda DA, Becker DP, Katayama Y. Secondary injury and acidosis. J Neurotrauma 1992 9(Suppl 1):S47-S60. PMID: 1588632.


18. Katoh S, el Masry WS, Jaffray D, McCall IW, Eisenstein SM, Pringle RG, et al. Neurologic outcome in conservatively treated patients with incomplete closed traumatic cervical spinal cord injuries. Spine (Phila Pa 1976) 1996 21:2345-2351. PMID: 8915069.


19. Kawano O, Ueta T, Shiba K, Iwamoto Y. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: a multicenter prospective study. Spinal Cord 2010 48:548-553. PMID: 20065985.


20. Lee TT, Green BA, Gromelski EB. Safety and stability of open-door cervical expansive laminoplasty. J Spinal Disord 1998 11:12-15. PMID: 9493764.


21. Lee TT, Manzano GR, Green BA. Modified open-door cervical expansive laminoplasty for spondylotic myelopathy: operative technique, outcome, and predictors for gait improvement. J Neurosurg 1997 86:64-68. PMID: 8988083.


22. McKinley W, Meade MA, Kirshblum S, Barnard B. Outcomes of early surgical management versus late or no surgical intervention after acute spinal cord injury. Arch Phys Med Rehabil 2004 85:1818-1825. PMID: 15520977.


23. Mirza SK, Krengel WF 3rd, Chapman JR, Anderson PA, Bailey JC, Grady MS, et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res 1999 104-114. PMID: 10078133.

24. Papadopoulos SM, Selden NR, Quint DJ, Patel N, Gillespie B, Grube S. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma 2002 52:323-332. PMID: 11834996.


25. Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF. Neurological recovery, mortality and length of stay after acute spinal cord injury associated with changes in management. Paraplegia 1995 33:254-262. PMID: 7630650.


26. Tator CH. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol 1995 5:407-413. PMID: 8974623.


27. Vale FL, Burns J, Jackson AB, Hadley MN. Combined medical and surgical treatment after acute spinal cord injury: results of a prospective pilot study to assess the merits of aggressive medical resuscitation and blood pressure management. J Neurosurg 1997 87:239-246. PMID: 9254087.


28. Wilmot CB, Hall KM. Evaluation of the acute management of tetraplegia: conservative versus surgical treatment. Paraplegia 1986 24:148-153. PMID: 3748593.


29. Yoo DS, Lee SB, Huh PW, Kang SG, Cho KS. Spinal cord injury in cervical spinal stenosis by minor trauma. World Neurosurg 2010 73:50. -52. discussion e54. PMID: 20452868.


30. Young W. The post-injury responses in trauma and ischemia: secondary injury or protective mechanisms? Cent Nerv Syst Trauma 1987 4:27-51. PMID: 3301009.


Fig. 1
Neurologic outcome according to pre-existing lesion There was better neurologic outcome in those who had OPLL than other pre-existing lesion before injury (p<0.05).
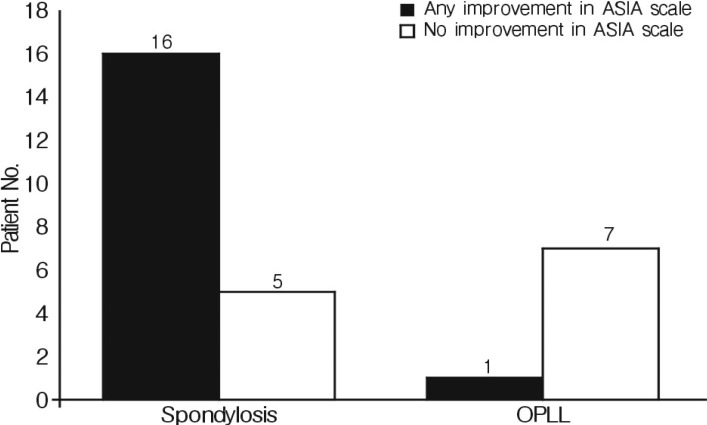
Fig. 2
Neurologic outcome according to cervical stenosis degree Good neurologic outcome was showed at 40-60% cord compression rate but no significant statically difference (p≥0.05).
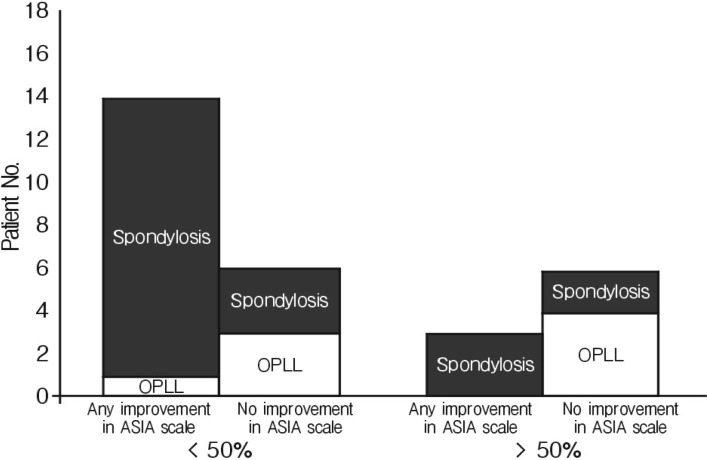
Table 1.
Demographic data of patients
| Category | No. |
|---|---|
| Gender (M/F) | 26 (90%)/3 (10%) |
| Mean age (years) | 57±10.4 |
| Pre-existing stenotic lesion | |
| Spondylosis | 21 |
| OPLL | 8 |
| Timing of surgery | |
| Within 24 hours | 25 (74%) |
| After 24 hours | 4 (26%) |

- TOOLS
-
METRICS

-
- 6 Crossref
- Scopus
- 5,972 View
- 68 Download
- Related articles in NS
-
Journal Impact Factor 3.2