Anatomical Relationship of the Vertebral Artery With the Lateral Recess: Clinical Importance for Posterior Cervical Foraminotomy
Article information
Abstract
Objective
Vertebral artery injuries during posterior cervical foraminotomy are rare, but can be fatal. Therefore, we investigated the anatomical correlation between the lateral recess and the vertebral artery.
Methods
On axial cuts of cervical magnetic resonance imaging from 108 patients, we measured the distance between the vertebral arteries and the medial border of the facet joints. The anatomical vertebro-facet distance (AVFD), surgical vertebro-facet distance (SVFD), and vertebro-facet angle (VFA) were measured.
Results
The mean AVFD values on the right side at the C3–4, C4–5, C5–6, and C6–7 levels showed statistically significant differences. On the right side, the mean SVFD values were equivalent to the AVFD values. The mean values of the VFA on the right side at all levels showed statistically significant differences. For all measurements, the greatest differences were seen between the C5–6 and C6–7 levels, and higher levels were associated with smaller distances from the lateral recess. The mean values of the AVFD on the right and left sides showed statistically significant differences at all levels, and the distances on the left were smaller than those on the right.
Conclusion
The vertebral artery is closer to the lateral recess at higher cervical levels than at lower cervical levels. The largest distances were found at the C5–6 and C6–7 levels, and the left vertebral arteries were closer to the lateral recess than the right vertebral arteries.
INTRODUCTION
The vertebral arteries arise from the postero-superior aspect of the both central subclavian arteries and reach both transverse processes of the C6 vertebra in 94.9% of individuals, or C4, C5, or C7 in 1.6%, 3.3%, and 0.3% of individuals, respectively [1]. Then, they enter and travel through the transverse foramina of each cervical vertebra. After crossing the transverse foramina of C1, the vertebral arteries proceed horizontally in grooves on the posterior arch of C1, and at the end of the groove turn obliquely, vertically, and medially toward the foramen magnum [2].
Vertebral artery injury during posterior cervical surgery is rare, but can cause complications such as massive hemorrhage, dissection, cerebral infarction, pseudo-aneurysm, and even death. The incidence of vertebral artery injury has been reported to range from 0.07% to 1.4% [3,4]. Its incidence is higher when the posterior approach is used (4.1%–8.2%) than when the anterior approach is used (0.3%–0.5%) [5-8]. Instrumented posterior surgery of the upper cervical spine is the commonest cause of vertebral artery injury [9,10]. Consequently, most clinical and anatomical studies have focused on avoiding vertebral artery injury in upper cervical surgery. However, vertebral artery injury can also occur during posterior cervical foraminotomy in the subaxial spine [3,11]. The incidence of vertebral artery injury is predicted to increase because a growing number of surgeons are performing endoscopic cervical foraminotomies [12,13]. Under these circumstances, the anatomical correlation of the vertebral artery with the lateral recess become very important. In a literature review, we could not find studies that focused on these anatomical correlations and ways to avoid vertebral artery injury during posterior cervical foraminotomy. Therefore, we measured the anatomical relationships between the vertebral artery and the lateral recess.
MATERIALS AND METHODS
1. Study Patients
This study is a retrospective review of 108 patients who underwent magnetic resonance imaging (MRI) from January 2018 through May 2018 at a single center (Gangnam Nanoori Hospital, Seoul, Korea). The patients were selected randomly, regardless of their symptoms and diseases. Fifty-six men and 52 women with a mean age of 46.3 years (range, 20–74 years) provided consent and were included in the study.
This study was approved by the Ethics Committee of Nanoori Hospital. Informed consent was obtained from the patients.
2. Imaging Analysis
The images in this study were from a GE Signa 1.5-T HDxT MRI Machine (GE Healthcare, Milwaukee, WI, USA). All measurements were taken on T2-weighted axial images arranged parallel to the intervertebral disc using an Infinitt PACS M6 Version (Infinitt Healthcare Co., Seoul, Korea). The images were obtained using a fast spin-echo sequence with an echo train length of 28, a bandwidth of 25 Hz, a repetition time of 3,000 msec, an echo time of 110 msec, a field of view of 160×160 mm, a number of excitations of 2, a slice thickness of 3 mm, and a slice gap of 0.5 mm.
We measured 3 values to characterize the anatomical relationship between the vertebral artery and the lateral recess. All values were measured on the right and left sides from the center of the C2–3, C3–4, C4–5, C5–6, and C6–7 intervertebral disc levels, as described below.
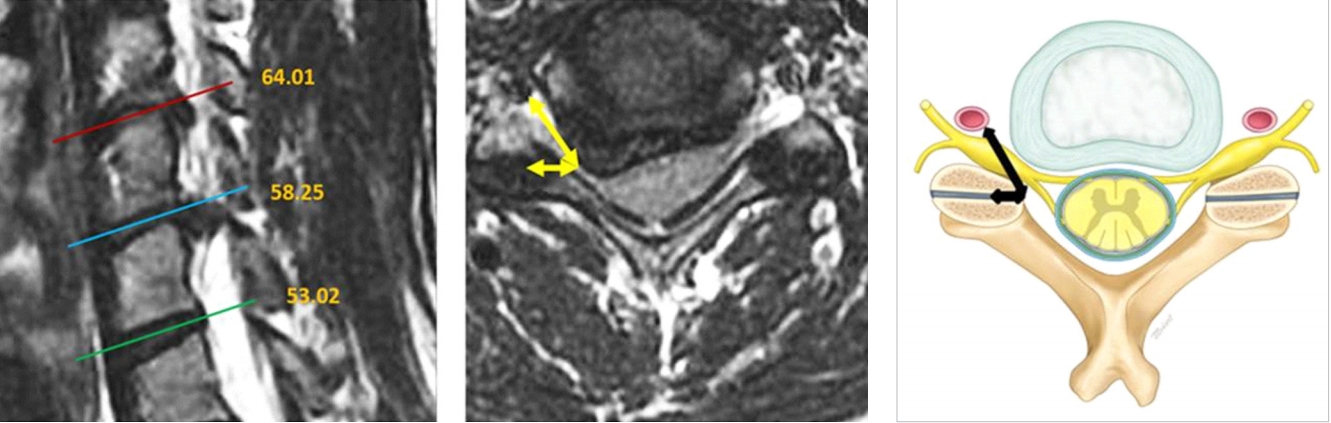
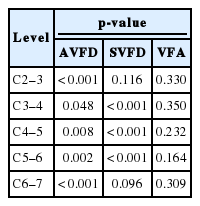
(1) Anatomical vertebro-facet distance (AVFD): The shortest linear distance was measured between the vertebral artery and the medial border of the facet joint (Fig. 1).
Anatomical Vertebro-Facet Distance (AVFD) measured the shortest distance between vertebral artery and medial border of facet joint.
(2) Surgical vertebro-facet distance (SVFD): The shortest distance was measured between a line tangential to the medial margin of the vertebral artery and another line tangential to the medial border of the facet joint (Fig. 2).
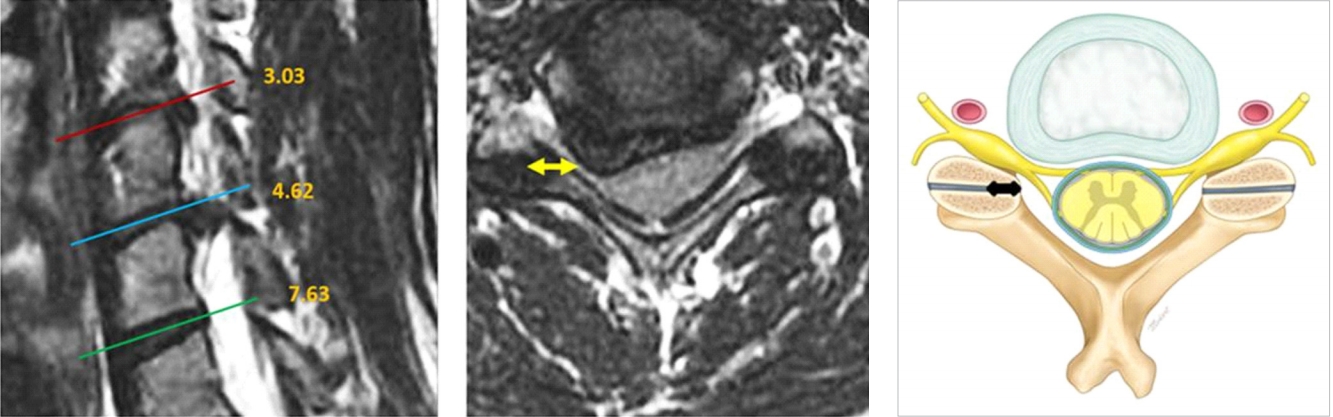
Surgical Vertebro-Facet Distance (SVFD) measured the shortest distance between vertical extension line of medial margin of vertebral artery and medial border of facet joint.
(3) Vertebro-facet angle (VFA): The angle between AVFD and SVFD was measured (Fig. 3).
3. Statistical Analysis
Statistical analyses were performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Means and standard deviations (mean±standard deviation) were calculated, and statistical significance was assessed using the paired t-test. Differences between mean values at consecutive levels and between the right and left sides at the same level were compared. A p-value<0.05 was considered to indicate a statistically significant difference.
RESULTS
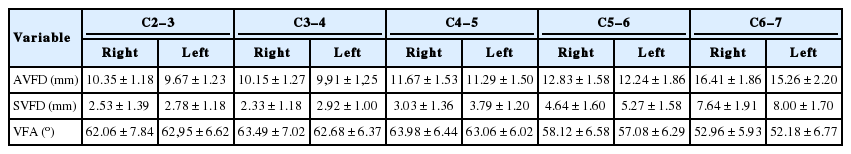
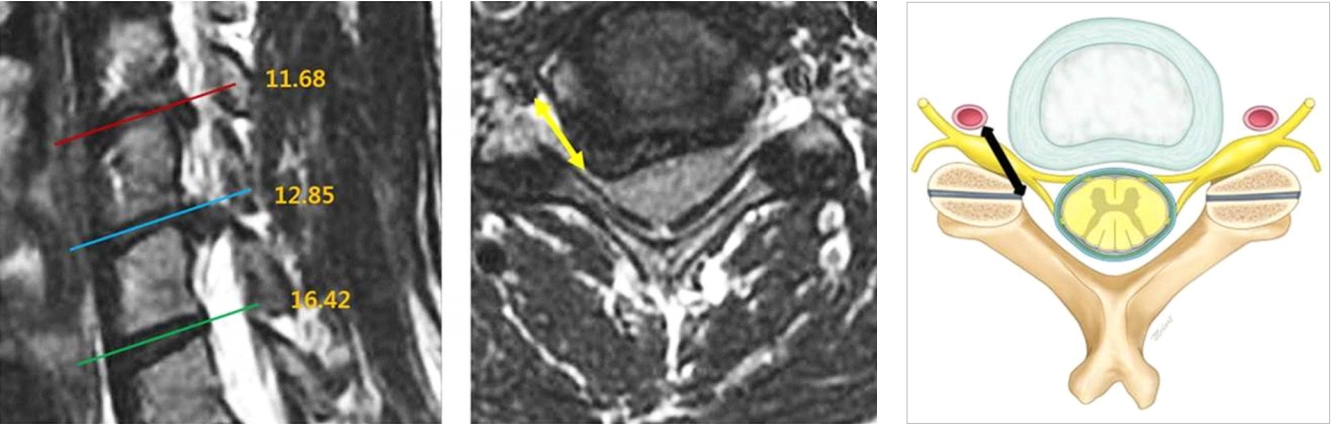
We calculated the mean AVFD, SVFD, and VFA on both sides (Table 1, Fig. 4). The mean AVFD showed statistically significant differences at the C3–4 (10.15±1.27 mm), C4–5 (11.67±1.53 mm), C5–6 (12.83±1.57 mm), and C6–7 (16.41±1.86 mm) levels (p<0.001 at all levels) (Table 2). The greatest difference was found between C5–6 (12.83±1.57 mm) and C6–7 (16.41±1.86 mm). At higher levels, the artery was closer to the lateral recess. The mean SVFD values on the right side showed statistically significant differences at the C3–4 (2.33±1.18 mm), C4–5 (3.03±1.36 mm), C5–6 (4.64±1.60 mm), and C6–7 (7.64±1.91 mm) levels (p<0.001 for all levels), and the greatest difference was found between C5-6 (4.64±1.57 mm) and C6-7 (7.64±1.91 mm).
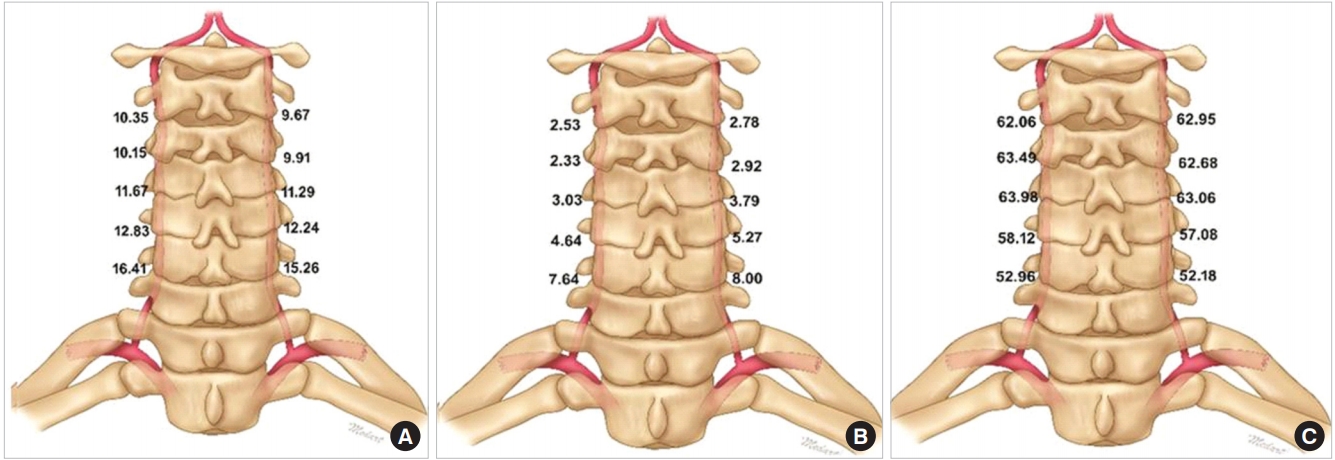
Schematic illustration of vertebral artery seen from posterior and measured values: (A) Mean AVFD (mm); (B) mean SVFD (mm); (C) mean VFA (°).
The mean VFA values on the right side were calculated, and the statistical significance of differences between adjacent levels was calculated. Statistically significant differences were found at all levels (p=0.046 for C2–3 and C3–4; at other levels p<0.001) and the greatest difference was found between C5–6 (58.12°±6.58°) and C6–7 (52.96°±5.93°). On the right side, the mean VFA increased from the C6–7 level to the C4–5 level, and then decreased from the C4–5 level to the C2–3 level.
The AVFD showed a statistically significant difference between the right side and left side at all levels, with the left-side values being smaller than the right-side values (p<0.001 for C2–3, p=0.048 for C3–4, p=0.008 for C4–5, p=0.002 for C5–6, and p<0.001 for C6–7) (Table 3). The SVFD also showed statistically significant differences between the right and left sides at C3–4, C4–5, and C5–6 (p<0.001, p<0.001, p<0.001, respectively). However, in contrast to the AVFD, the SVFD values on the right side were smaller than those on the left side. No statistically significant difference was found in the VFA between the right and left sides at any level (p=0.330 for C2–3, p=0.350 for C3–4, p=0.232 for C4–5, p=0.164 for C5–6, and p=0.309 for C6–7).
DISCUSSION
Few studies have investigated vertebral artery injury in posterior cervical foraminotomy. Lunardini et al. [3] reported that only 1.8% of vertebral artery injuries occurred during posterior foraminotomy. Many studies have reported the anatomical relationship of the uncinate process or longus colli muscle with the vertebral artery because these are used as anatomical landmarks in anterior cervical foraminotomy [14-17]. However, to the best of our knowledge, no previous study has investigated the location of the vertebral artery in relation to landmarks relevant for posterior cervical foraminotomy, such as the lamino-facet junction. Therefore, we measured the distance and angle between the vertebral artery and the medial border of the facet joint to characterize the anatomical correlations of the artery. We expect that our measurements will be helpful in the future for avoiding vertebral artery injury during posterior cervical foraminotomy.
The AVFD is the actual distance from the lateral recess to the vertebral artery. A few studies have reported the distance between the midline and vertebral artery, but we did not find any previous reports that presented measurements of the distance between the lateral recess and vertebral artery. The vertebral artery is located farthest from the midline at lower cervical levels (such as C6 and C7) and becomes closer to the midline at upper cervical levels (such as C3 and C4) [17,18]. Similar to the above studies, we found that the vertebral artery became closer to the lateral recess as the cervical level increased from C6–7 to C3–4 (Fig. 4).
The vertebral artery most commonly enters the transverse foramen of C6 (94.9%), followed in order by C5, C4, and C7.1 In our study, the mean AVFD at the C6–7 level was 16.41±1.86 mm on the right side and 15.26±2.20 mm on the left side. The mean AVFD at the C5–6 level was 12.83±1.58 mm on the right side and 12.24±1.86 mm on the left side. This difference exists because the artery enters into the transverse foramen of C6 from the antero-lateral aspect. Thus, the vertebral artery approaches the lateral recess rapidly at the C5–6 level, meaning that surgeons should be especially cautious regarding the location of the vertebral artery at this level and above.
The lamino-facet junction is an important landmark in posterior cervical foraminotomy. Identification of this landmark is followed by resection of the medial aspect of the facet, which may include one-third to half of the facet because segmental hypermobility of the cervical spine occurs if a foraminotomy involves resection of more than 50% of the facet [19-21]. The SVFD is the distance that dictates the exact amount of facet resection that can be performed safely. On the right side, the SVFD was 7.64±1.91 mm at the C6–7 level, but 4.64±1.60 mm at C5–6 and 2.33±1.18 mm at C3–4. These measurements show that the vertebral artery at the C5–6 level and higher is very close to the lateral recess and the facet, which means that during posterior cervical foraminotomy at C5–6 or above, the vertebral artery is usually hidden ventral to the exposed nerve root. Therefore, surgeons should be careful when manipulating the cervical nerve root at the C5–6 level and above because of the proximity of the artery to the lateral recess and the nerve root.
The VFA represents the angle of approach of the vertebral artery towards the lateral facet, which is especially relevant when performing endoscopic foraminotomy. Endoscopic surgery requires frequently changing the angle of the endoscope to visualize structures better. Small and flexible instruments such as radiofrequency ablation devices can easily enter the ventro-lateral side of the nerve root and injury the vertebral artery. Therefore, it is important to know the angle between the vertebral artery and facet joint. In our study, the mean VFA rapidly increased moving upwards from C6–7 (52.96°±5.93°) to C4–5 (63.98°±6.44°), followed by slight decreases at C3–4 (63.49°±7.02°) and C2–3 (62.06°±7.84°) on the right side. Posterior cervical foraminotomy at C4–5 should be carried out with caution because the vertebral artery approaches the lateral recess at a very steep angle.
In the present study, the AVFD was smaller on the left side than on the right side at all levels, but no difference was found between the VFAs on the right and left sides. Previous studies have compared the distance between the vertebral artery and various anatomical landmarks on both sides, including a report showing that the left vertebral artery was closer to the superior ridge of the uncinate process [14]. Another group reported that the left vertebral artery was closer to the midline than the right vertebral artery [18]. We suggest that these results may be related to the diameter of the vertebral artery, because previous studies have reported that the left vertebral artery had a larger diameter than the right vertebral artery [14,18,22,23]. Another study reported that approximately 70% of patients had a left-dominant vertebral artery [24]. These results may explain the measured distances between the vertebral artery and fixed anatomical landmarks.
This study had certain limitations. First, we could not exclude the possibility of selection bias because this was a single-center retrospective study. Second, the sample of patients may not have been representative of the entire population of various races or nationalities. Third, measurement errors may have occurred because the MRI axial cut in the measurements used in our study had a 3.5-mm slice gap, and measurement variability could have existed across different individuals. Nonetheless, this study is meaningful as the first attempt to describe the anatomical relationship of the lateral recess and vertebral artery. A multicenter study with a better design and larger sample size would yield more reliable insights into the topic. In addition, a meta-analysis of previous studies would remove the effect of investigator bias and produce a better understanding of the issue.
CONCLUSION
This study demonstrated the anatomical relationship of the vertebral artery with the lateral recess. The distance from the lateral recess to the vertebral artery decreased from lower cervical levels (such as C6–7) to upper cervical levels (C3–4 level), and the greatest difference was found between the C5–6 and C6–7 levels. The vertebral artery was closer on the left side than on the right side. The angle of the vertebral artery to the lateral recess increased sharply from C6–7 to C4–5 and then slightly decreased from C4–5 to C2–3. During posterior cervical foraminotomy, surgeons should consider this information to avoid injuring the vertebral artery.
Notes
The authors have nothing to disclose.
Acknowledgements
We would like to acknowledge scientific team members Ms. Jae Eun Park, Mr. Kyeong-Rae Kim, and Mr. Sang Hyuck Yoon for providing assistance in acquiring full text articles and managing digital works.