A New Shielding Curtain for Protection of Intraoperative Radiation During Minimally Invasive Spine Surgery
Article information
Abstract
Objective
Gradually increasing number of minimally invasive spine surgery (MISS), there is an increasing risk of radiation exposure to medical personnel during the surgery. We measured the radiation exposure of the operating room personnel during MISS, tried to find the riskiest person, and checked the effectiveness of a new lead-composite shielding curtain.
Methods
Radiation exposure of medical staffs (operator, first assistant, anesthesiologist, and scrub nurse) involved in MISS procedures of 35 patients without shielding curtain (nonshield group) and 35 patients with shielding curtain (shield group). The shielding curtain had 0.25-mm nominal lead equivalent and was mounted on 2 frame bars fixed on the operating table.
Results
In the nonshield group, radiation exposure was significantly higher in the order of operator > first assistant > scrub nurse > anesthesiologist (p < 0.001) during both anteroposterior (AP) and lateral views. In the shield group, the radiation exposure of the operator and the scrub nurse decreased significantly by 94.1% and 76.4% in AP view (p < 0.001), and by 96.3% and 73.9% in lateral view (p < 0.001), respectively.
Conclusion
Since the radiation dose of the operator was highest in a C-arm-guided MISS, there is a high priority need to protect the operator from the radiation exposure. The shielding curtain could most effectively reduce the radiation exposure of the operator.
INTRODUCTION
Recently, the use of minimally invasive spine surgery (MISS) is increasing due to its advantages of decreased neural injury, shorter hospital stay, reduced bleeding, less postoperative pain, and lower infection rate [1,2]. However, MISS uses fluoroscopy more often than open surgery, which exposes the medical staffs to radiation-induced complications such as cataract, leukemia, thyroid cancer, skin erythema, etc [3,4].
To minimize radiation exposure, several methods such as wearing protective devices (lead aprons, lead glasses, and thyroid shields), reducing the number of fluoroscopy imaging, keeping a distance from the X-ray source during imaging, and using O-arm navigation have been proposed [5]. However, all of these methods have some disadvantages, such as discomfort or fatigue of the operator during operation, decreased accuracy for instrumentation, adverse health effects of lead exposure, and high cost [6,7].
In this study, we measured the radiation exposure of the operating room personnel during MISS, tried to find a person receiving the highest dose of radiation, and evaluated the effectiveness of a new lead-composite radiation shielding curtain.
MATERIALS AND METHODS
From August 30, 2017 to December 31, 2017, the radiation exposure of medical staffs (operator, first assistant, anesthesiologist, and scrub nurse) involved in MISS on the lumbar spine of 70 patients performed by one surgeon was measured. Radiation dose (µSv/hr) was measured in MIS discectomy or fusion surgery. The fusion surgeries were divided into 1-, 2-, and 3-level fusion. Radiation exposure time was checked for each operation type. We measured body mass index (BMI) and bone mineral density (BMD) of the patients. Of the 70 patients, 35 patients underwent the MISS without the shielding curtain (nonshield group) and other 35 patients with the shielding curtain (shield group). In the shield group, the shielding curtain was mounted on the operator’s side preoperatively. We used C-arm fluoroscopy (SPINEL 3G, GEMSS MEDICAL, Seongnam, Korea) with the peak voltage (kVp), tube current (mA), and exposure time adjusted automatically at each time of the imaging. The operator and the first assistant were positioned opposing each other facing the patient, the anesthesiologist was positioned at the patient’s head, and the scrub nurse was positioned near patient’s legs next to the first assistant (Fig. 1). The radiation doses were measured as an absorbed dose rate (µSv/hr) with Raysafe X2 (Unfors RaySafe, Billdal, Sweden) 5 times during anteroposterior (AP) and lateral views, respectively, and were averaged in both groups. In the AP view, the X-ray source of the C-arm was located below the operating table. In the lateral view, the X-ray source was located on the operator’s side, and the detector on the first assistant's side. To check the protection rate of the shielding curtain, radiation doses for all medical staffs were measured at the waist level outside the lead apron during the C-arm imaging. This study was approved by the Institutional Review Board of Chung-Ang University Hospital (approval number: 1904-012-16263), and patient consent was not necessary for this research.

Positions of medical staffs during operation. The stars indicate the location of dosimeter measuring radiation exposure dose in anteroposterior (A) and lateral (B) views.
1. Shielding curtain
A shielding curtain made of a lead-composite X-ray protective sheet of 0.25-mm nominal lead equivalent, fabricated by department of Chemical Engineering, Keimyung University, was used for the study. The polyurethane solution (23wt%) was prepared by mixing n,n-dimethylformamide (Duksan Chemical, Incheon, Korea), with polyurethane (Songwon, Seoul, Korea), followed by the addition of lead powder (67wt%) and nano-metal powder (10wt%) (300 mesh, 99.8%, CNPC Powder Group Co. Ltd, Shanghai, China) to the mixture to form the final solution. The final solution was then cast onto Oxford fabric (P/250D OX, Yeonil, Seoul, Korea), washed and dried to form the final protective sheet. The shielding curtain sized 0.8 m× 0.8 m with a density of 2.39 kg/m2 (total weight= 1.53 kg) and was mounted on 2 frame bars fixed on the operating table at the operator side (Fig. 2). The shielding curtain was not sterilized, and a surgical drape was placed on it to prevent contamination during lateral view.
2. Statistical analysis
To compare radiation exposure among the operating room personnel, we performed analysis of variance and conducted a post hoc analysis. We calculated a radiation protection rate between nonshield and shield groups and confirmed the statistical significance by the Student t-test. The results were expressed as mean values± standard deviation, and p-value of < 0.05 was considered statistically significant.
RESULTS
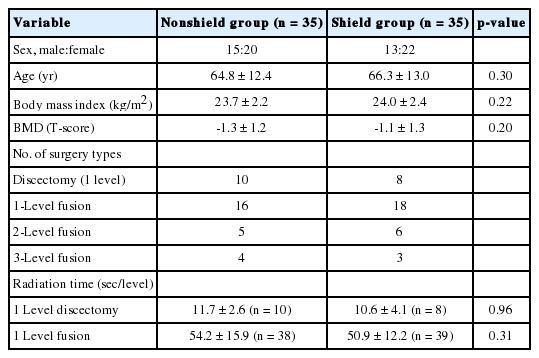
This study enrolled 35 patients in the nonshield group and 35 in the shield group. There were no significant differences in sex ratio, mean age, BMI, BMD and radiation exposure time between the groups (Table 1).
1. Radiation exposure in the nonshield group
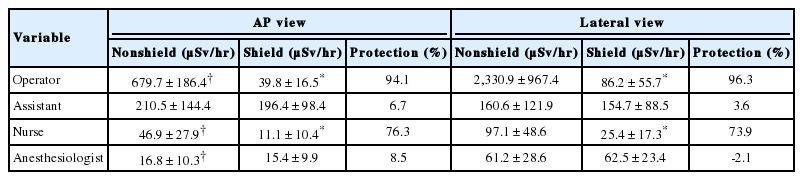
Radiation exposure during AP view in the nonshield group was significantly higher in the following order: operator (679.7± 186.4 µSv/hr), first assistant (210.5± 144.4 µSv/hr), scrub nurse (46.9 ± 27.9 µSv/hr), and anesthesiologist (16.8 ± 10.3 µSv/hr) (p< 0.001). Radiation exposure during lateral view in the nonshield group was significantly higher in the following order: operator (2,330.9± 967.4 µSv/hr), first assistant (160.6± 121.9 µSv/hr), scrub nurse (97.1± 48.6 µSv/hr), and anesthesiologist (61.2± 28.6 µSv/hr) (p< 0.001) (Table 2). In particular, the operator’s radiation exposure was approximately 14.5 times greater than that of the first assistant who had the second largest radiation exposure. Except for the first assistant, the radiation exposures of the operator, the scrub nurse, and the anesthesiologist were significantly higher in lateral view compared with AP view (p < 0.001). The operator received radiation about 3.43 times higher during lateral view compared to AP view, which were -0.76, 2.07, and 3.65 times for the 1st assistant, scrub nurse, and anesthesiologist, respectively.
2. Radiation exposure in the shield group
During AP view, the results of the shield group were as follows: operator (39.8± 16.5 μSv/hr), first assistant (196.4± 98.4 μSv/hr), scrub nurse (11.1± 10.4 μSv/hr), and anesthesiologist (15.4± 9.9 μSv/hr). During lateral view, those in the shield group were as follows: operator (86.2 ± 55.7 μSv/hr), first assistant (154.7± 88.5 μSv/hr), scrub nurse (25.4± 17.3 μSv/hr), and anesthesiologist (62.5± 23.4 μSv/hr) (Table 2). There were statistically significant decreases in radiation exposure to the operator and scrub nurse compared with nonshield group in both AP and lateral view (p< 0.001). The radiation protection rate in the AP view was 94.1% and 76.4% for the operator and the scrub nurse, respectively. There was no statistically significant decrease in radiation exposure for the first assistant and anesthesiologist. Similarly, the radiation protection rate of lateral view was 96.3% and 73.9% for the operator and the scrub nurse, respectively. For the first assistant and the anesthesiologist, there was no significant protective effect by the shielding curtain.
DISCUSSION
As the minimally invasive technique has been developed and widely used in spine surgery, the use of C-arm fluoroscopy is being increased to improve the accuracy of equipment, and the number of medical staffs experiencing complications due to low-dose ionizing radiation increases as well [8]. There are a number of studies reporting significant exposure of radiation in MISS [3, 9-11], as well as a study reporting a 5-fold increase in the incidence of lifetime cancer of orthopedic surgeons compared to general practitioners [12].
Wearing protector is the most common protection method, but it has an adverse effect on the human body because the fatigue of the operator is increased due to its heavy weight [6,7]. To overcome these drawbacks, we have developed a new protection method using a shielding curtain with low lead content, which can be attached to an operating table.
The important point in this process was the question of who should be protected more. According to previous study, the operator with the closest distance from the radiation source has the most radiation exposure than the other operating room personnel [13]. Likewise, in our study, the radiation exposure was the highest for the operator both in AP and lateral views, and was reduced in the order of the first assistant, scrub nurse, and anesthesiologist. Especially, since the operator received 14.5 times more radiation than the first assist who is the second exposure, we considered the protection of the operator was the most urgent issue.
Radiation exposure, the chromosomal aberrations, chromosomal damage, and cancer risk increase [14,15]. Therefore, it is desirable to keep radiation exposure as low as possible. The shielding curtain seemed to be effective for protection against ionizing radiation. Because the shielding curtain is simply mounted on the operating table, the operator does not have to wear heavy protective devices. It also has the advantage of being able to protect against all parts of the body. The International Commission on Radiological Protection (ICRP) defined the occupational radiation exposure dose limit as 20,000 μSv/yr [16]. According to our data, when the radiation exposure dose was calculated roughly as the average of AP and lateral views with shielding curtain, 22,453 and 8,058 fusion levels per year for surgeon and first assistant, respectively, seem to be the maximum number according to the ICRP guideline. In addition, it does not interfere with the use of C-arm and has advantages over the O-arm and navigation equipment in terms of cost. It is expected that the combination of shielding curtains with conventional protective efforts will minimize the radiation exposure more effectively.
The shielding curtain used in our study is a lead-composite protector with a shielding effect of 0.25-mm lead equivalent, which is relatively light weight and contains less lead. In previous studies, it was reported that wearable lead protector showed radiation protection by 92%–98% [17-19]. The shielding curtain reduced the radiation exposure of the operator, who received the greatest radiation, by 94.14% and 96.30% in AP and lateral view, respectively. The protection rate of the shielding curtain used in our study showed results similar to previous studies performed using a wearable protector.
The radiation exposure was higher in the lateral view than in the AP view for the medical staffs except the first assistant with or without shielding curtain. In the first assistant, the radiation exposure was reduced in the lateral view because the distance to the generator increased and direct radiation was blocked by the patient’s body as the generator went to the opposite side. In the AP view without shielding curtain, the radiation dose to the operator was significantly higher than the assistant. The reason of that phenomenon seems to be the greater distance from the generator to the assistant because the operator stand just in front of the generator and the assistant is located at the side of the C-arm arc. The C-arm arc itself also seems to protect some radiation to the assistant. During the lateral view, the radiation exposure was increased in the operator because the C-arm generator is located on the operator side, and it also increased in the scrub nurse and the anesthesiologist because of the increased direct radiation exposure. The shielding curtain showed high protection rates for the operator in both AP and lateral view since the shielding curtain was mounted on the operator side. Scrub nurse also showed significant protection rate by the shielding curtain because a part of shielding curtain covered the patient’s leg side.
There are several limitations in our study. The shielding curtain also showed disadvantages: more time for mounting the shielding curtain, more effort for rotation of the C-arm to Lat view due to the weight of the shielding curtain, and has a risk of infection when used without sterilization. However, such disadvantages are expected to be overcome by improving design of curtain stands, reducing weight of the shield by using lead-free material. Although there was no infection during the study, developing a sterilizable or disposable curtain would be helpful for infection prevention. In our study, the amount of radiation varied according to the patient’s body size because the C-arm was used in the automatic brightness control mode. We measured the exposure in AP view and lateral view respectively, and did not compare the total exposure. Therefore, we had to focus on the shielding effectiveness and comparison among medical staff rather than the absolute value of the radiation dose. The shielding curtain used in our study showed an effective protection for the operator, but the protection of the other personnel was less effective. Although shielding curtain may have a shielding effect on most of the body, our study only measured radiation exposure at the waist level. A further study will be necessary to determine the shielding effect on the whole body by measuring the radiation exposure to other parts of body. Since this is a retrospective study with a relatively small scale, we planned a larger scale and prospective study as a next step.
CONCLUSION
Operator was the most exposed to radiation, and the shielding curtain was a very effective method to protect the operator from radiation during surgery. Shielding curtains reduce the fatigue of the operator by mounting on an operating table. If the mounting method and the design of the shielding curtain are improved, it is expected that it will be an effective measure of radiation protection.
Notes
The authors have nothing to disclose.