 |
 |
- Search
Abstract
Objective
A Zero-profile device is a cervical stand-alone cage with integrated segmental fixation device. We characteristically evaluated the radiological changes as well as clinical outcomes in the application of Zero-profile devices compared with stand-alone cages and anterior cervical plates with iliac bone grafts for the cervical disease.
Methods
Retrospectively, total 60 patients at least more than one year follow-up were enrolled. Twenty patients were treated with Zero-profile devices (Group A), twenty patients with stand-alone cages (Group B) and twenty patients with anterior cervical plates and iliac bone grafts (Group C) for a single level cervical disease. The clinical outcomes were evaluated by Odom's criteria and Bazaz-Yoo dysphagia index. The radiologic parameters were by subsidence and the changes of the midpoint interbody height (IBH), the segmental kyphotic angle (SKA), the overall kyphotic angle (OKA) in index level.
Results
Although there was no significant clinical difference according to the Odom's criteria among them(p=0.766), post-operative dysphagia was significantly decreased in the Group A and B compared with the Group C (p=0.04). From the immediate postoperative to the last follow-up time, the mean change of IBH decrement and SKA increment were significant in the Group B compared with the Group A (p=0.025, p=0.033) and the Group C (p=0.001, p=0.000). The subsidence rate was not significant among all groups (p=0.338).
Smith and Robinson's technique had been the "gold standard" for the surgical treatment of cervical disc disease36). However, anterior cervical plates with iliac bone grafts may be associated with higher.
postoperative chronic iliac pain14,35) and higher rates of dysphagia10,11,19,30,39). For those reasons, stand-alone cervical cages have also been used to avoid these complications. The polyethyletherketone (PEEK) cage has good biomechanical properties and reduces the stress shielding effects. It is also easy to determine the cervical interbody fusion radiologically. However, the problems of cages are known as increasing subsidence and loss of cervical lordosis11,39). These results led to the development of a stand-alone cage with integrated fixation device for Zero-profile segmental stabilization (Synthes GmbH Swithzerland, Oberdorf, Switzerland).
Many authors reported that the clinical outcomes between the stand-alone cages and the anterior cervical plates for cervical disc disease were similar13,16,17,33). There are some articles about the Zero-profile devices3,4,8,12,15,18,23,24,29) or focusing dysphagia in the anterior cervical discectomy and fusion3,34,41). Some authors found the Zero-profile devices have lower incidence of dysphagia compared with titanium plate and cage29,34,41). However, we limit its use because of National Health Insurance allowance at the moment.
In addition, there is no direct comparative research about clinical and radiological outcomes among three groups, as far as we know: Zero-profile devices, stand-alone cages, and anterior cervical plates with iliac bone grafts for the cervical disease. Here, we wrote this paper to compare the clinical and radiological outcomes among them.
Retrospectively, we evaluated total sixty patients treated with a single level ACDF from January 2008 to June 2013 in a retrograde order. The demographic findings of the patients were summarized (Table 1). They were divided into three groups; Zero-profile devices in group A (n=20), standalone PEEK cages in group B (n=20) and cervical anterior plates with autologous iliac bone grafts in group C (n=20). The average follow-up durations of the group A, group B and group C were 13.2 months, 13.1 months and 13.6 months, respectively.
The inclusion criteria were; (1) signs and symptoms of cervical radiculopathy or cervical spondylotic myelopathy which was unresponsive to the conservative treatment, (2) single level disease confirmed by clinical symptom and imaging (Computed tomography scan or Magnetic resonance imaging), (3) complete continuous clinical and imaging data. The exclusion criteria were; (1) history of previous cervical spine surgery, (2) others cervical diseases, including infection, tumor, deformity or ossification of posterior longitudinal ligament, (3) requirement for simultaneous anterior and posterior surgery, or hybrid surgery.
All operative procedures were performed by one neurosurgeon. A standard anterior Smith approach was performed. After removing the disc material, the cartilage endplates were scraped with a curette and high speed electric drill. The posterior osteophytes were removed by Kerrison punches. Once neural decompression was performed, the height, length and depth were measured of the discectomy level. For fusion bed, milling procedure was performed with diamond drill. The patients were reconstructed with three different methods.
In the Group A, the interbody fusion was performed with Zero-profile devices with four screws were tightened into the adjacent cervical bony segment (Fig. 1A). In the Group B, the inter-body fusion was carried out with PEEK cages (Fig. 1B). The DBM was filled into the cage for fusion in the Group A and B. In the Group C, the inter-body fusion was accomplished with anterior cervical titanium plates and autologous tri-cortical iliac bone grafts fixed by four screws (Fig. 1C). We advised all patients to use of a cervical collar for a month after the surgery.
Clinical outcome was evaluated according to the Odom's criteria. These criteria provide the healthy status and daily activities limitations. Patients were rated as excellent, good, fair and poor. Excellent state is all preoperative symptoms relieved and abnormal findings improved; Good state is minimal persistence of preoperative symptoms; Fair state is definite relief of some preoperative symptoms, but other symptoms unchanged or slightly improved; Poor state is symptoms and signs unchanged or exacerbated. Furthermore, postoperative dysphagia and chronic donor site pain were observed.
Three radiographic parameters were estimated at the preoperative, the immediate postoperative and the last follow-up time (range: 12-15 months), finally. The lateral plain radiographs of the cervical spine were used for the measurement of the midpoint interbody height (IBH), the segmental kyphotic angle (SKA) and the overall kyphotic angle (OKA) in index level.
The IBH is defined as the distance between the midpoint of the superior end plate of upper vertebra and inferior end plate of lower vertebra of the affected segments. The SKA (α) is defined as the angle between the superior end plate of the upper vertebra and the inferior end plate of the lower vertebra of the affected segment. The OKA (β) is defined as the angle between the inferior endplate of C2 and the inferior endplate of C7 (Fig. 2).
Postoperative subsidence was defined as any settlement in the disc height of at least 3 mm on the lateral radiographs16).
Statistical analysis was achieved using SPSS for Mac (version 20.0, SPSS Inc, Chicago, IL, USA). Clinical and Radiological interval changes of subgroups were analyzed using the ANOVA test, Chi-Square test, Mann-Whitney U-test and Wilcoxon signed rank test. The statistical significance was defined as p<0.05.
Postoperatively, the majority of patients of all groups were good or excellent according to the Odom's criteria. There was no significant difference among them(p=0.766) (Table 3).
One (5.0%) patient complained of mild dysphagia 2 weeks after surgery in the Group A and B, however, the dysphagia disappeared after 2 months. There were six (30%) patients complained of dysphagia in the Group C. Four patients complained of mild dysphagia 2 weeks after surgery. Two patients complained of moderate dysphagia 2 months after surgery. After conservative treatment, such as oromotor fascilitation and feeding training, five patients had recovered after 2 months and one patient recovered after 6 months. The incidence of dysphagia of Group A and B was lower than Group C (p= 0.040) (Table 4).
In the Zero-profile devices group, the immediate postoperative IBH was increased compared with the preoperative time and then decreased at the last follow-up time (p=0.000, p=0.000), respectively. However, the mean IBH was increased from the preoperative to the last follow-up time (p=0.000). The immediate postoperative SKA was decreased compared with the preoperative time and then increased at the time of the last follow-up (p=0.001, p=0.000), respectively. However, the mean SKA was decreased from the preoperative to the last follow-up time (p=0.000). There were no significant interval changes of OKA as time goes on (Table 5).
In the stand-alone cages group, the immediate postoperative IBH was increased compared with preoperative time and then decreased at the last follow-up time (p=0.000, p=0.000), respectively. However, the mean IBH was decreased from the preoperative to the last follow-up time (p=0.000). The immediate postoperative SKA was decreased compared with the preoperative time and then increased at the time of the last follow-up (p=0.004, p=0.007), respectively. However, the mean SKA was increased from the preoperative to the last follow-up time (p=0.011). There were no significant changes of OKA in process of time (Table 5).
In the anterior cervical plates with autologous iliac bone graft group, the immediate postoperative IBH was increased compared with the preoperative time and then decreased at the last follow-up time (p=0.000, p=0.000), respectively. However, the mean IBH was somewhat decreased from the preoperative to the last follow-up time (p=0.000). The immediate postoperative SKA was decreased compared with the preoperative time and then somewhat increased at the time of the last follow-up (p=0.001, p=0.000), respectively. However, the mean SKA was decreased from the preoperative to the last follow-OKA as time as time goes by(Table 5).
The change of IBH showed significantly more decreased in the Group B than the Group A from the immediate postoperative to the last follow-up time and from the preoperative to the last follow-up time (p=0.025, p=0.000), respectively. The change of SKA showed significantly more increased in the Group B than the Group A from the immediate postoperative to the last follow-up time and from the preoperative to the last follow up time (p=0.033, p=0.025), respectively. The change of OKA showed significantly more increased in the Group B than the Group A from the preoperative to the last follow-up time (p=0.044) (Table 6).
The change of IBH was significantly more decreased in the Group C than the Group B from the preoperative to the immediate postoperative time (p=0.036). However, it was significantly more decreased in the Group B than the Group C from the immediate postoperative to the last follow-up time (p=0.001).
The change of SKA showed significantly more increased in the Group B than the Group C from the immediate postoperative to the last follow-up time and from the preoperative to the last follow-up time (p=0.000, p=0.006), respectively. However, there was no significant difference of OKA between them(Table 6).
The change of IBH was significantly more increased in the Group A than the Group C from the preoperative to the immediate postoperative time and from the preoperative to the last follow-up time (p=0.001, p=0.004), respectively. However, there was no significant difference of SKA and OKA between them (Table 6).
The highest incidence of subsidence was in the Group B. However, there was no statistical significance among them in this study (p=0.338) (Table 7).
Degenerative conditions of the cervical disease are commonly treated by discectomy and subsequent interbody fusion. ACDF is the gold standard for the surgical management at the present. Although the cervical total arthroplasty is possible operative techniques25,32,40), the inclusion criteria are somewhat limited2). On the ACDF, the biomechanical stability is mandatory7,9,28,30,42).
Various types of cages have been used to perform ACDF, including titanium, carbon fiber reinforced polymer (CFRP), and polyetheretherketone (PEEK) cages. The radiolucent PEEK cages have superior biomechanical properties and a similar elastic coefficient to that of human bone, as well as a reduced stress shielding effect, which reduces the bone weakness and increases the fusion rate. However, graft extrusion was reported as 2% on the average. In our study, there was no graft extrusion, nor screw loosening.
Generally, anterior cervical plates using various interbody grafts enhance stabilizing properties and increase fusionrates1,12,22,31,47). However, this procedure using anterior plates is associated with various intraoperative and postoperative complications, especially dysphagia. It also demands iliac bone harvest which causes chronic iliac site pain5,37,38). Studies have demonstrated that the chronic pain rate can still be 18.7%, two years after iliac crest surgery14,35). Three patients (15%) of our Group C complained of chronic postoperative donor site pain. The incidence was lower than the previous other study14,35).
Meanwhile, the cervical stand-alone cage with integrated fixation for the Zero-profile segmental fixation devices has four screws for internal screw fixation and a one-step locking mechanism. This device is made of radiolucent PEEK polymer and has a radio-opaque titanium alloy plate to verify placement. This Zero-profile device acts as a stand-alone device for use in cervical interbody fusion4,8,12,15,18,23,24). Its design combines the functionality of a cervical interbody spacer and the benefits of an anterior cervical plate which limits the risk of damage to adjacent organs like vessels, soft tissues or nerves. Biomechanical testing has shown the stability of the Zero-profile device to be similar to that of established anterior cervical plate with cage34).
Many authors reported that the clinical outcomes between the stand-alone cage and the anterior cervical plate for cervical disc disease were similar13,16,17,33). This current study including Zero-profile devices found that there was no significant clinical difference for a single level cervical disease among them (Group A, B and C) according to the Odom's criteria (Table 3).
In ACDF, a common complication is chronic dysphagia with a general incidence of around 3-21% before the Zeroprofile devices era10,30). Wang et al.41) found that only one of twenty two patients (4.5%) using Zero-profile device and eight of the twenty five patients (32%) using anterior cervical titanium plate and cage complained of dysphagia. Azab et al.3) reported that 39 of 75 patients (76%) using Zero-profile device had mild dysphagia with symptom duration of 17±9 days. At 6 weeks' follow-up, 8 patients (10.5%) complained of mild dysphagia which resolved completely by 3 months in all of them.
Although the exact pathophysiologic mechanism of dysphagia after ACDF remains unknown, Lee et al.21) reported that dysphagia was related to the thickness of the titanium plate at the level of fusion. Fountas et al.10) explained postoperative dysphagia due to soft tissue edema, hematoma, esophageal injury and adhesion formations around implanted cervical plates. This Zero-profile device can be completely contained in the decompressed intervertebral space, avoiding the mechanical stimulus to the esophagus and other pre-vertebral soft tissues41). It may lessen the incidence of the dysphagia. In addition, the Zero-profile device is not placed across the anterior vertebral body, which reduces the dissection of pre-vertebral soft tissues and preserves as many normal anatomical tissues as possible41).
This study showed that the dysphagia incidence of Group A and Group B was 5%, respectively, while that of Group C was 20% in the early postoperative period and 10% in the medium period (Table 4).
After conservative treatment, five patients had recovered after 2 months and one patient recovered after 5 months. Our dysphagia incidence was consistent with other studies34,41).
On the other hand, the radiologic change of IBH and SKA of all groups had similar pattern as time passes. That is, the immediate postoperative IBH was increased from the preoperative time and then decreased at the time of the last follow-up (p=0.000 and p=0.000 in Group A, B and C), and the immediate postoperative SKA was decreased from the preoperative time and then increased at the time of the last follow-up (p=0.001 and p=0.000 in the Group A, p=0.004 and p=0.007 in Group B, p=0.001 and p=0.000 in Group C) (Table 5). However, they did not affect the OKA change as time passes (Table 5).
From the immediate postoperative to the last follow-up time, the change of IBH showed significantly more decreased in the Group B compared with the Group A and Group C (p=0.025, p=0.001), respectively. In addition, from the immediate postoperative to the last follow-up time, the change of SKA showed significantly more increased in the Group B compared with the Group A and Group C (p=0.033, p=0.000), respectively (Table 6). However, they all did not affect OKA among them(Table 6).
We think the radiologic comparison of intergroup at the preoperative time was not meaningful because of preoperative individual difference. What we want to highlight is the interval changes of each radiologic parameter.
Many studies reported that subsidence rate varies between 23.4-50.5%27,44). There has been reported the risk factors associated with subsidence. Nonsurgical risk factors are obesity, bone mineral density and smoking, while surgical factors were anteroposterior diameter of cage and intraoperative distraction46). However subsidence does not always result in poor prognosis or aggravation of symptoms, and mostly does not cause symptoms or morbidity33,43,45). In this study, the incidence of subsidence was 50.0% in the Group A, 70.0% in Group B, and 45.0% in Group C. There was no statistical significance among them between Group A and Group C(p=0.338) (Table 7).
In cases of subsidence, we frequently observed the final fusion was formed with some segmental kyphotic change that did not cause secondary symptom. They did not have to require re-operation.
However, the radiologic summation effect of IBH or subsidence20) and kyphotic change should be considered in multi-level procedure or kyphosis anticipated. For example, the anterior cervical plate with cage or autologous iliac bone graft has been known as the most preferable choice. However, selection of the Zero-profile devices may be suitable as well considering its similar radiologic result with anterior cervical plate and iliac bone graft group.
We performed computerized tomography (CT) scans to evaluate fusion in five patients of the Group A in twelve months after the operation that showed definitely bridging bone formation within the cage and around the cages at (Fig. 3). However measuring the distance between the tips of the spinous processes at the surgically treated level in flexion-extension lateral plain x-ray is most reliable and strict method for evaluating spine fusion apart from CT scan.
Although different cervical levels in this study may be pointed out the problems, we observed just the change of IBH, SKA and OKA by time period. Therefore, we think that their radiographic analysis was not influenced by the levels. The pitfalls of this study were followings; Firstly, small number of patients. Secondly, Zero-profile device has been used lately. Thirdly, we did not demonstrate fusion rate among them. Therefore, these short points may have our results be biased.
There was no significant difference according to the Odom's criteria in a single level cervical disease among three groups. However, the incidence of dysphagia is significantly lower in the Zero-profile device and stand-alone cage group compared with anterior cervical plate and iliac bone graft group(p=0.040). Naturally, the Zero-profile devices and stand-alone cage need not iliac bone harvest. The Zero-profile device group has similar radiologic result with anterior cervical plate and iliac bone graft group. Although, prospective randomized trials with more patients and longer follow-up in the Zeroprofile device are necessary to confirm its pros and cons, surgeon should select the prime device in the light of patients.
References
1. Anderson DG, Albert TJ. Bone grafting, implants, and plating options for anterior cervical fusions. Orthop Clin North Am 2002 33(2):317-328. PMID: 12389278.


2. Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR. The prevalence of indications and contraindications to cervical total disc replacement. Spine J 2008 8(5):711-716. PMID: 17983843.


3. Azab W, Abdel-Razek M, Ali A, Abdelrahman A, Salaheldin W, Nasim K, et al. Outcome evaluation of a zero-profile implant for anterior cervical diskectomy with fusion. Turk Neurosurg 2012 22(5):611-617. PMID: 23015339.


4. Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J 2007 16(9):1395-1400. PMID: 17221174.



5. Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 2006 58(3):502. -508. discussion 502-508. PMID: 16528190.


6. Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: A prospective study. Spine (Phila Pa 1976) 2002 27(22):2453-2458. PMID: 12435974.


7. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993 75(9):1298-1307. PMID: 8408151.


8. Caspar W, Geisler FH, Pitzen T, Johnson TA. Anterior cervical plate stabilization in one- and two-level degenerative disease: Overtreatment or benefit? J Spinal Disord 1998 11(1):1-11. PMID: 9493763.


9. Farey ID, McAfee PC, Davis RF, Long DM. Pseudarthrosis of the cervical spine after anterior arthrodesis. Treatment by posterior nerve-root decompression, stabilization, and arthrodesis. J Bone Joint Surg Am 1990 72(8):1171-1177. PMID: 2398087.


10. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007 32(21):2310-2317. PMID: 17906571.


11. Fowler BL, Dall BE, Rowe DE. Complications associated with harvesting autogenous iliac bone graft. Am J Orthop (Belle Mead NJ) 1995 24(12):895-903. PMID: 8776079.

12. Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: A metaanalysis of fusion rates. J Neurosurg Spine 2007 6(4):298-303. PMID: 17436916.


13. Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: Sequential changes in cage subsidence. J Clin Neurosci 2008 15(9):1017-1022. PMID: 18653347.


14. Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res 1997 (339):76-81. PMID: 9186204.


15. Herrmann AM, Geisler FH. Geometric results of anterior cervical plate stabilization in degenerative disease. Spine (Phila Pa 1976) 2004 29(11):1226-1234. PMID: 15167662.


16. Huh J, Oh JY, Chough CK, Cho CB, Joo WI, Park HK. Polyetheretherketone cage filled with beta-tricalcium phosphate versus autogenous tricortical iliac bone graft in anterior cervical discectomy and fusion. Korean J Spine 2011 8(3):165-171.

17. Joo YH, Lee JW, Kwon KY, Rhee JJ, Lee HK. Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc 2010 48(4):342-346. PMID: 21113362.



18. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002 50(2):229. -236. discussion 236-228. PMID: 11844257.


19. Kasimatis GB, Panagiotopoulos E, Gliatis J, Tyllianakis M, Zouboulis P, Lambiris E. Complications of anterior surgery in cervical spine trauma: An overview. Clin Neurol Neurosurg 2009 111(1):18-27. PMID: 18977582.


20. Kim S, Chun HJ, Yi HJ, Bak KH, Kim DW, Lee YK. Long-term follow-up radiologic and clinical evaluation of cylindrical cage for anterior interbody fusion in degenerative cervical disc disease. J Korean Neurosurg Soc 2012 52(2):107-113. PMID: 23091668.



21. Lee MJ, Bazaz R, Furey CG, Yoo J. Influence of anterior cervical plate design on dysphagia: A 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 2005 18(5):406-409. PMID: 16189451.


22. Malloy KM, Hilibrand AS. Autograft versus allograft in degenerative cervical disease. Clin Orthop Relat Res 2002 (394):27-38. PMID: 11795743.

23. Mobbs RJ, Rao P, Chandran NK. Anterior cervical discectomy and fusion: Analysis of surgical outcome with and without plating. J Clin Neurosci 2007 14(7):639-642. PMID: 17532499.


24. Moftakhar R, Trost GR. Anterior cervical plates: A historical perspective. Neurosurg Focus 2004 16(1):E8PMID: 15264786.

25. Nabhan A, Ahlhelm F, Pitzen T, Steudel WI, Jung J, Shariat K, et al. Disc replacement using pro-disc c versus fusion: A prospective randomised and controlled radiographic and clinical study. Eur Spine J 2007 16(3):423-430. PMID: 17106665.


26. Oh HS, Shim CS, Kim JS, Lee SH. Clinical and radiological comparison of femur and fibular allografts for the treatment of cervical degenerative disc diseases. J Korean Neurosurg Soc 2013 53(1):6-12. PMID: 23439721.



27. Oh K, Lee CK, You NK, Kim SH, Cho KH. Radiologic changes of anterior cervical discectomy and fusion using allograft and plate augmentation: comparison of using fixed and variable type screw. Korean J Spine 2013 10(3):160-164. PMID: 24757479.



28. Phillips FM, Carlson G, Emery SE, Bohlman HH. Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976) 1997 22(14):1585-1589. PMID: 9253093.


29. Qi M, Chen H, Liu Y, Zhang Y, Liang L, Yuan W. The use of a zero-profile device compared with an anterior plate and cage in the treatment of patients with symptomatic cervical spondylosis: A preliminary clinical investigation. Bone Joint J 2013 95(4):543-547. PMID: 23539708.


30. Riley LH Jr, Robinson RA, Johnson KA, Walker AE. The results of anterior interbody fusion of the cervical spine. Review of ninety-three consecutive cases. J Neurosurg 1969 30(2):127-133. PMID: 5780880.


31. Romner B, Due-Tonnessen BJ, Egge A, Anke IM, Trumpy JH. Modified robinson-smith procedure for the treatment of cervical radiculopathy. Acta Neurol Scand 1994 90(3):197-120. PMID: 7847061.


32. Sasso RC, Smucker JD, Hacker RJ, Heller JG. Clinical outcomes of bryan cervical disc arthroplasty: A prospective, randomized, controlled, multicenter trial with 24-month follow-up. J Spinal Disord Tech 2007 20(7):481-491. PMID: 17912124.


33. Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 2006 4(6):447-453. PMID: 16776355.


34. Scholz M, Reyes PM, Schleicher P, Sawa AG, Baek S, Kandziora F, et al. A new stand-alone cervical anterior interbody fusion device: Biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976) 2009 34(2):156-160. PMID: 19139665.


35. Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 2003 28(2):134-139. PMID: 12544929.


36. Smith GW, Robinson RA. The treatment of certain cervicalspine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958 40-a(3):607-624. PMID: 13539086.


37. Song KJ, Lee KB. A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci 2006 13(2):181-187. PMID: 16459086.


38. Summers BN, Eisenstein SM. Donor site pain from the ilium. A complication of lumbar spine fusion. J Bone Joint Surg Br 1989 71(4):677-680. PMID: 2768321.


39. Thorell W, Cooper J, Hellbusch L, Leibrock L. The long-term clinical outcome of patients undergoing anterior cervical discectomy with and without intervertebral bone graft placement. Neurosurgery 1998 43(2):268. -273. discussion 273-264. PMID: 9696079.


40. Wang Y, Cai B, Zhang XS, Xiao SH, Wang Z, Lu N, et al. [Clinical outcomes of single level bryan cervical disc arthroplasty: A prospective controlled study]. Zhonghua Wai Ke Za Zhi 2008 46(5):328-332. PMID: 18785525.

41. Wang ZD, Zhu RF, Yang HL, Gan MF, Zhang SK, Shen MJ, et al. The application of a zero-profile implant in anterior cervical discectomy and fusion. J Clin Neurosci 2014 21(3):462-466. PMID: 24262773.


42. White AA 3rd, Southwick WO, Deponte RJ, Gainor JW, Hardy R. Relief of pain by anterior cervical-spine fusion for spondylosis. A report of sixty-five patients. J Bone Joint Surg Am 1973 55(3):525-534. PMID: 4703205.


43. Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: A retrospective study. Eur Spine J 2012 21(7):1374-1382. PMID: 22205113.


44. Yamagata T, Takami T, Uda T, Ikeda H, Nagata T, Sakamoto S, et al. Outcomes of contemporary use of rectangular titanium stand-alone cages in anterior cervical discectomy and fusion: Cage subsidence and cervical alignment. J Clin Neurosci 2012 19(12):1673-1678. PMID: 23084624.


45. Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (peek) cage. Clin Orthop Surg 2011 3(1):16-23. PMID: 21369474.



46. Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976) 1991 16(7):726-729. PMID: 1925745.


47. Zdeblick TA, Phillips FM. Interbody cage devices. Spine (Phila Pa 1976) 2003 28(15 Suppl):S2-S7. PMID: 12897467.


Fig. 1
(A) Post-operative radiographs showing the Zero-profile device for a single level cervical disease. (B) Post-operative radiographs showing stand-alone cage for a single level cervical disease. (C) Post-operative radiographs showing anterior cervical plate with autologous bone graft for a single level cervical disease.
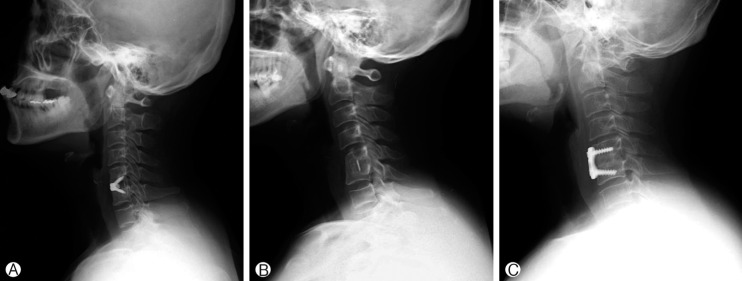
Fig. 2
Postoperative radiographs illustrating the interbody height (IBH), the segmental kyphotic angle (SKA=α), and the overall kyphotic angle (OKA=β).
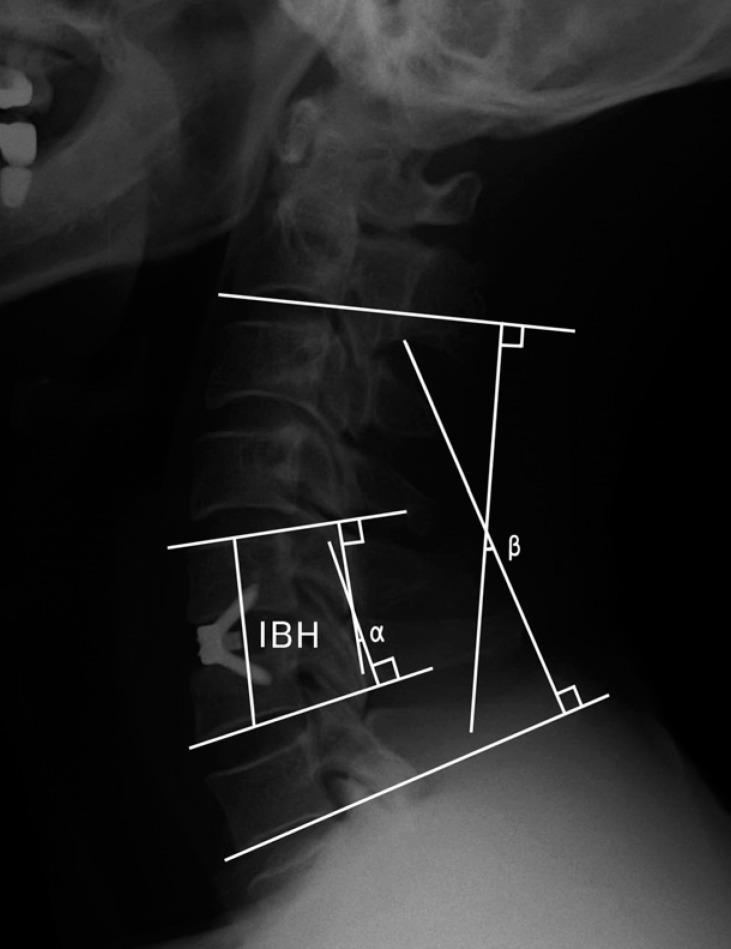
Fig. 3
Coronal cervical CT scan of a patient with Zero-profile device on the C6/7 level illustrating bridging bone formation.

Table 1.
Demographic data of the enrolled patients
Table 2.
Dysphagia scoring system
| Symptom Severity | Liquid food | Solid food |
|---|---|---|
| None | None | None |
| Mild | None | Rare |
| Moderate | None or rare | Occasionally (only with specific food) |
| Severe | None or rare | Frequent (majority of solids) |
Table 3.
Clinical outcome according to Odom’s criteria
| Group A (N=20) | Group B (N=20) | Group C (N=20) | p-value | |
|---|---|---|---|---|
| Excellent | 15 | 14 | 16 | 0.766 |
| Good | 5 | 6 | 4 | |
| Fair | 0 | 0 | 0 | |
| Poor | 0 | 0 | 0 |
Table 4.
Incidence of dysphagia
|
p-value |
||||||
|---|---|---|---|---|---|---|
| Group A (N=20) | Group B (N=20) | Group C (N=20) | Group A vs Group B | Group B vs Group C | Group A vs Group C | |
| Dysphagia n (%) | 1 (5.0) | 1 (5.0) | 6 (30.0) | 1.000 | 0.040 | 0.040 |
Table 5.
The mean values and the comparison of the preoperative, the immediate postoperative and the last follow-up time
Table 6.
The comparison of intergroup

- TOOLS
-
METRICS

-
- 25 Crossref
- Scopus
- 8,292 View
- 119 Download
- Related articles in NS
-
Journal Impact Factor 3.2

























