INTRODUCTION
Neurofibromatosis type 1 (NF-1) is an autosomal dominant hereditary disease and up to half of patients, orthopedic disorders are present, especially scoliosis, which is the most common skeletal manifestation1,5,10,13,14). These spinal deformities usually divided into dystrophic and non-dystrophic groups depending on the absence or presence of three or more bony dystrophic elements9). The treatment outcome of dystrophic scoliosis in neurofibromatosis type 1 are less satisfactory than other scoliotic types due to the particular pathogenesis and clinical characteristics including neurofibromas adjacent to the spinal cord, poor bone quality with significant multiplanar spinal deformities6,14). Therefore, surgical treatment of dystrophic scoliosis usually includes circumferential fusion to enhance stability and to make solid fusion17). But in case of severe dysplastic scoliosis patients, especially pedicle dysplasia with massive dural ectasia, circumferential fusion is sometimes too risky to obtain. We report a successfully treated patient of deformity surgery using multiple iliac screws and Wisconsin wire.
CASE REPORT
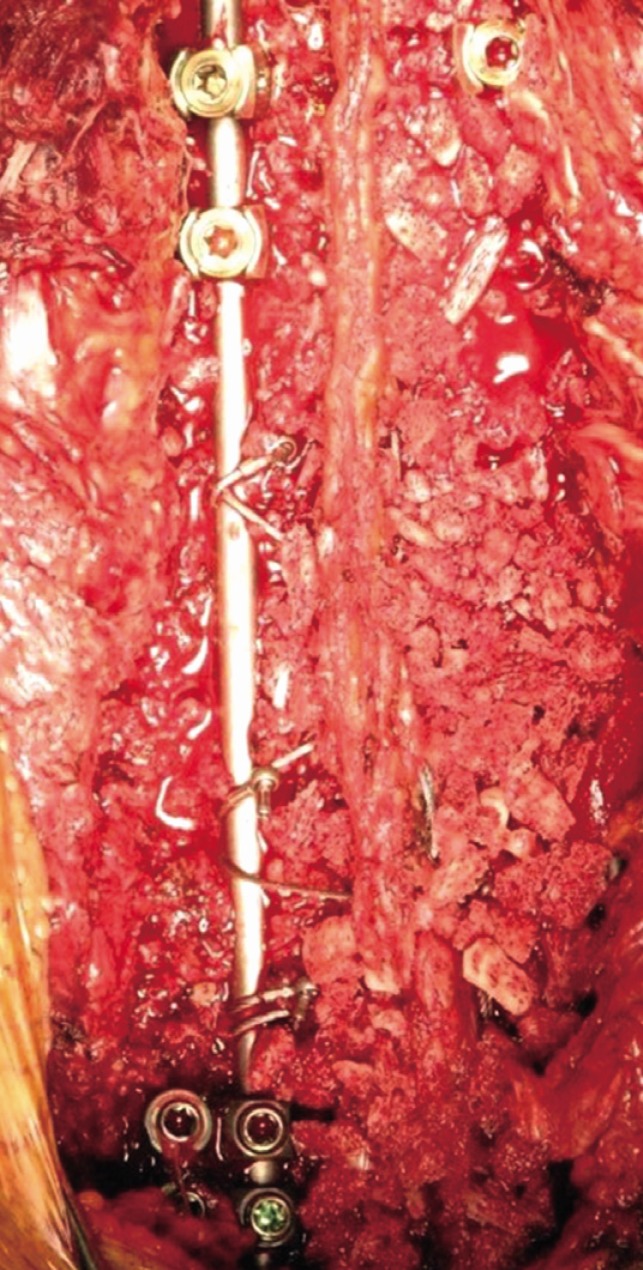
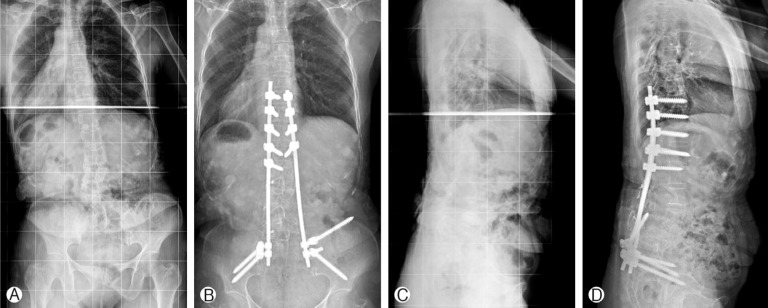
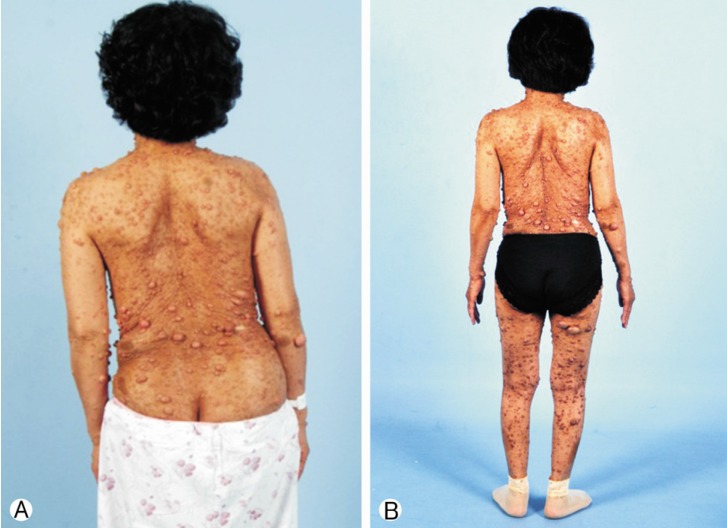
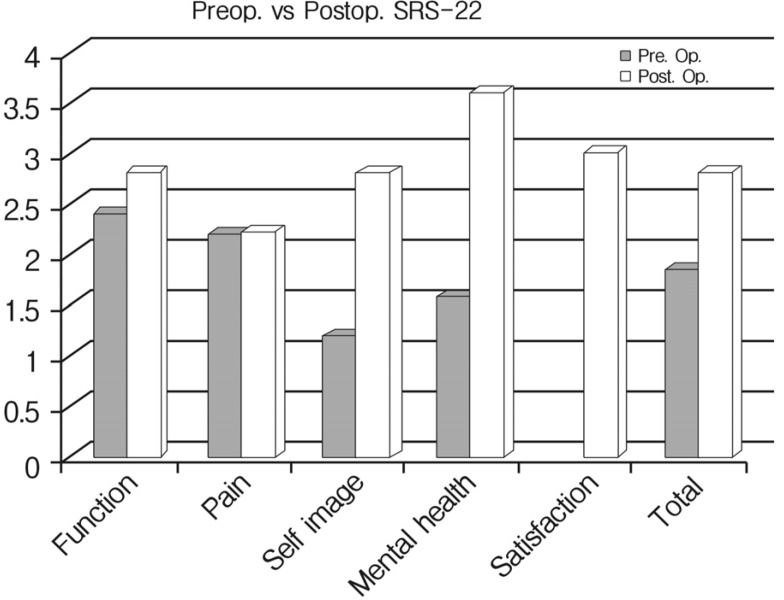
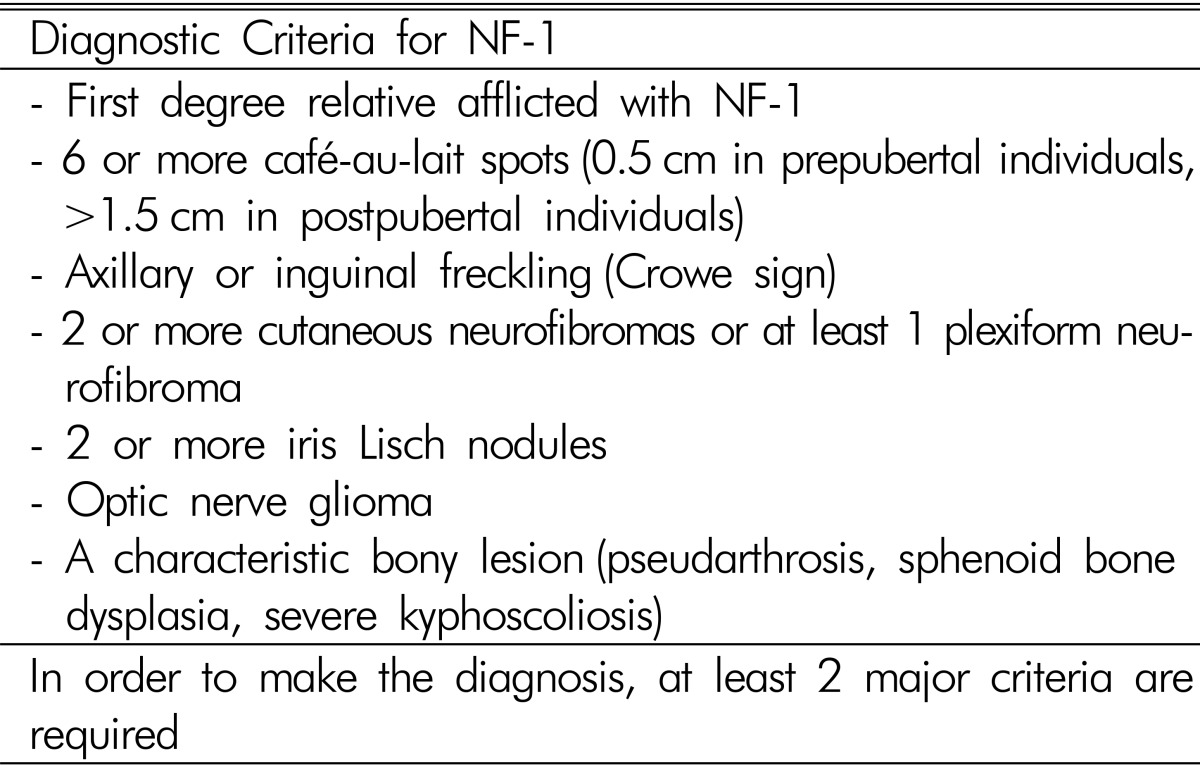
A 54-year-old female presented with low back pain and deformity of the spine for the past twenty years. Before one year to visit our clinic, back and buttock pain was gradually being aggravated especially when she lay down or sat up. On physical examination, multiple caf├®-au-lait spots and neurofibromas were found over her body. Plain radiographs and computerized tomographic (CT) myelogram confirmed the presence of scoliosis with truncal shift to the left side and bony scalloping from L2 to S2 with dural ectasia (Fig. 1). Cutaneous neurofibromas, caf├®-au-lait spots, and kyphoscoliosis were corresponded to the diagnostic criteria of NF-1 (Table 1). Bone mineral density examination showed severe osteoporosis (T- score: -4.9). Progressive truncal shifting and axial back pain made us decide to undergo a deformity correction surgery. With prone position on Jackson table, posterior segmental spinal instrumentation and fusion was performed from T9 to the pelvis. Dural ectasia and osseous dysplasia precluded the use of pedicle screws from L2 to the pelvis. Because insufficient insertion points for pedicle screws, we used multiple iliac screws and modified Wisconsin interspinous segmental wiring technique to obtain adequate fixation points and to achieve solid fusion. Thirteen total fixation points were established with eight bilateral pedicle screws from T9 to T12, unilateral screws on L1 and four iliac screws. Wisconsin wires (titanium cable) were applied to link the spinous process to the left side rod with help of miniplates to prevent bone cutting by the cable (Fig. 2). After decortication of posterior bony element of spine, autologous bone chips and demineralized bone matrix mixed allograft bone chips were implanted. After deformity correction surgery, thoracic-lumbo-sacral orthosis was applied for three months in order to protect excessive strains and prevent dislodgement of the implants. Corrected spinal curve was well preserved during one-year follow-up period with solid fusion without neurologic deficit (Fig. 3 and 4). Ultimate follow-up Scoliosis Research Society-22r score was significantly improved comparing to that of preoperative score (Fig. 5).
DISCUSSION
Spinal deformity is a common feature of neurofibromatosis type 1 and the dystrophic lesion like dural ectasia aggravates the deformity more rapidly that provokes severe spinal instability and structural problems. Although the deformity is severe, there were no neurologic deficits as a result of a widened spinal canal due to the ectatic thecal sac16). Dystrophic scoliotic curves less than 20┬░ should be closely observed with short intervals to identify sudden and rapid progression8). For patients with 20-40┬░ scoliosis with less than 50┬░ of kyphosis, posterior spinal arthrodesis using segmental fixation with either multiple sublaminar wires or rod-hook constructs and the application of plentiful bone graft is strongly indicated14).
Apart from this selective group of patients that can be treated with isolated posterior instrumented fusion, for most dystrophic NF spine, circumferential fusion with anterior column support shows high fusion rate, good curve correction, and good functional outcome12,15,18,19,20). Thus, previous literatures recommend circumferential fusion and instrumentation as the most reliable surgical option in patients of thoracic kyphosis that exceeds 50 degrees17). Anterior autologous strut graft could reinforce the vertebral column followed by posterior instrumentation with copious amount of autologous iliac crest bone11,12). Nevertheless, the lack of the sufficient anterior bony structure from the dural ectasia and concerns for inevitable dural injury and uncontrollable leakage of cerebrospinal fluid made us decide posterior only surgery in this particular case. Because of dysplastic pedicle, we could not use the pedicle screws from L2 to sacrum. Moreover, anterior spinal fusion was not feasible. Thus, multiple iliac screws were inevitably needed to obtain more fixation points to enhance stability. Multiple iliac screws were previously introduced as a method for spinopelvic reconstruction after sacrectomy.
After rod implantation, we used modified Wisconsin interspinous segmental wiring technique connecting the spinous processes and the rod using titanium cable and miniplates7). Because of the disadvantages of the sublaminar wiring such as poor anchoring, and an increased risk of neurological injury, the usefulness of Wisconsin wiring has been recognized for better stabilization and avoiding the neurologic injury4,7,17). Moreover, considering her osteoporosis, we modified the Wisconsin interspinous segmental wiring technique using miniplates to prevent bone cutting by the cable.
There were some successful deformity correction and fusion cases by using recombinant human bone morphogenetic protein (rh-BMP)2,3). However, in Republic of Korea, rh-BMP is not officially available yet. Thus, we used autologous local bone, allograft bone chip and demineralized bone matrix for fusion.