 |
 |
- Search
| Neurospine > Volume 15(4); 2018 > Article |
|
|
Abstract
Objective
To evaluate the results of operative management of subaxial spine injuries managed with 2-level anterior cervical corpectomy and fusion with a cervical locking plate and autologous bone–filled titanium mesh cage.
Methods
This study included 23 patients with a subaxial spine injury who matched the inclusion criteria, underwent 2-level anterior cervical corpectomy and fusion at our institution between 2013 and 2016, and were followed up for neurological recovery, axial pain, fusion, pseudarthrosis, and implant failure.
Results
According to Allen and Ferguson classification, there were 9 cases of distractive extension; 4 of compressive extension; 3 each of compressive flexion, vertical compression, and distractive flexion; and 1 of lateral flexion. Sixteen patients had a score of 6 on the Subaxial Injury Classification system, and the rest had a score of more than 6. The mean follow-up period was 19 months (range, 12–48 months). Neurological recovery was observed in most of the patients (78.21%). All patients experienced relief of axial pain. None of the patients received a blood transfusion. Twenty-one patients (91.3%) showed solid fusion and 2 (8.69%) showed possible pseudarthrosis, with no complications related to the cage or plate.
Conclusion
Two-level anterior cervical corpectomy and fusion, along with stabilization with a cervical locking plate and autologous bone graft-filled titanium mesh cage, can be considered a feasible and safe method for treating specific subaxial spine injuries, with the benefits of high primary stability, anatomical reduction, and direct decompression of the spinal cord.
Cervical spine injury occurs in 3% of blunt trauma victims, but the results of spinal cord injuries can be devastating. The subaxial spine runs from C3 to C7 and is one of the most common sites of cervical spine injuries. In adults, approximately 63% of spinal cord injuries involve the cervical spine, of which 75% occur in the C3–7 region; of those injuries, 50% occur between C5 and C7. The most common causes of cervical trauma include motor vehicle accidents, falls from heights, violence, sports-related injuries, and a heavy object falling onto the head [1]. Subaxial spine injuries may range from minor strains to complete fracture dislocation, resulting in quadriplegia, functional loss, and permanent disability. The management of subaxial spine trauma is continuously evolving. The rapid development of cervical instrumentation and fusion techniques have led to changes in the treatment of subaxial trauma. Cervical trauma is treated outside specialty care centres by surgeons who have varying levels of experience with subaxial cervical spine trauma. These factors have led to the emergence of different management modalities in subaxial trauma [2]. Studies have described using both the anterior and posterior approach with stabilization done anteriorly, posteriorly, or combined. The posterior approach preserves the motion of the axis, but does not address instability on account of disc injury. The anterior approach has the advantage of short fusion and direct decompression of the spinal cord [3].
This study analysed our experiences with managing relevant subaxial cervical spine injuries with 2-level anterior cervical corpectomy and fusion. The focus of our study was to evaluate the outcomes and complications of 2-level anterior cervical corpectomy and fusion.
A total of 365 patients who underwent subaxial spine surgery and presented to the Emergency Department of our tertiary care teaching hospital between January 2013 and December 2016 were analysed, of whom 23 patients matched the inclusion criteria: injury involving 2 contiguous vertebrae between C3 and C7, no other spinal injury, no evidence of the neurological weakness prior to injury, no pathological fracture, no evidence of involvement of the axial skeleton in rheumatoid arthritis or ankylosing spondylitis. Patients matching the inclusion criteria underwent 2-level anterior cervical corpectomy and fusion, were followed up at our institution, and were included in this study. The exclusion criteria included multiple-level spine injuries, pathological fracture, and prior involvement of the cervical spine in any systemic disease. Ethical clearance was obtained from the institutional ethics committee and informed written consent was provided by all patients.
All cases of 2-level anterior cervical corpectomy and fusion were performed with a cervical locking plate and autograft bonefilled titanium mesh cage. This was preferred over anterior cervical discectomy and fusion (ACDF) and posterior fusion, as in 80% of cases the injury pattern was anterior to the cord, so it would be difficult to address it posteriorly, and ACDF would be suboptimal in the setting of fractured vertebrae. Nearly 82.6% of the patients had been injured in motor vehicle accidents. All patients complained of pain, and their neck movements were restricted. The preoperative assessment included securing the airway and managing life-threatening injuries, followed by stabilization of the cervical injury with a hard cervical collar. Neurological status was assessed according to the American Spinal Injury Association (ASIA) criteria. Radiological assessment was then performed with anteroposterior and lateral views and computed tomography (CT) with 3-dimensional reconstruction. According to the Allen and Ferguson classification, there were 9 cases of extension; 4 of compressive extension; 3 each of compressive flexion, vertical compression, and distractive flexion; and 1 of lateral flexion. Sixteen patients had a score of 6 and the rest had a score of more than 6 according to the Subaxial Injury Classification (SLIC) system [4,5]. In our study, associated injuries were common: 48% of patients had a head injury, 38% had upper limb injuries, 32% had lower limb injuries, 36% had a chest injury, and 24% had an abdominal injury. Due to the associated injuries and the time required to stabilize the patient, surgical treatment was delayed by 1 week. During that period, traction or a cervical collar was applied depending on the injury mechanism. After surgery, patients were started on static neck exercises from the third postoperative day and made to sit in bed starting on the first postoperative day.
Southwick and Robinson’s approach was used in all cases. An intravenous antibiotic (third- generation cephalosporin) and an intravenous injection of 1,000 mg of hydrocortisone were given at the time of induction of general anaesthesia to prevent surgical site infection. The patient was positioned supine on the operating table. A Crutchfield tong was applied anteriorly to the ear. The patient’s neck was slightly extended. The head was slightly rotated by about 10°–15° to the opposite side. The reverse Trendelenburg position of about 10° was used to decrease the dependency on the head and neck during surgery and to reduce venous plexus congestion, which helped us prevent postoperative haematoma. A longitudinal incision of about 3 cm was made below the mandible parallel to the sternocleidomastoid over the left side of the neck. The platysma was identified by the direction of its fibres. The platysma was incised in line with the skin incision using electrocautery. A plane was developed deep to the platysma with blunt dissection, in order to avoid injuries to the numerous superficial veins, such as the anterior jugular and small branches of the external jugular vein, which cross the field. If encountered, injured veins were ligated with a 2-0 silk suture.
Adequate mobilization of the platysma enabled visualization of the medial fascial border of the sternocleidomastoid. The muscle fascia itself was not violated, to avoid bleeding. Furthermore, the fascia helps keep the plane of dissection out of the carotid sheath. Medially, the trachea was palpated through the overlying strap muscles, which include the sternothyroid and sternohyoid. The muscles were contained within an investing fascial layer. Interfascial dissection between the strap muscles and the sternocleidomastoid was developed bluntly. Once through this layer, finer dissection continued in a posteromedial direction toward the spine. The carotid pulse was palpated and the artery displaced laterally at all times, which ensured that the dissection was medial to the carotid sheath. A handheld retractor was placed gently on the medial aspect to retract the trachea and oesophagus, which further helped to prevent postoperative dysphagia. Disc level and fractured vertebrae were identified with a bent needle in the disc space and seen under an image intensifier. Once the fractured vertebrae were confirmed, the disc above and below the fractured vertebrae was marked with electrocautery. A discectomy of the level above and below was done prior to corpectomy to keep the field relatively bloodless, as bleeding from a corpectomy makes discectomy difficult. Following discectomy, between the fractured vertebrae and normal vertebrae on both sides, corpectomies of the vertebrae were done. The vertebral body was removed up to the uncovertebral joints, which are one of the most reliable references for the lateral border of the vertebral body. The vertebral body was debulked and decompression was performed slowly and cautiously in a ventral to dorsal manner. The lateral border of the space was repeatedly referenced to the uncovertebral joints above and below the vertebral body to prevent injury to the vertebral artery. After removing the cancellous bone, the posterior wall was removed using a Kerrison rongeur, and utmost care was taken to prevent postoperative radiculopathy. The distance between the end plates was carefully measured with traction applied. The bone harvested from the vertebrae that underwent corpectomy was further broken down into small pieces and packed into a titanium mesh cage of a premeasured size. The rigid titanium mesh cage tightly packed with the salvaged bone was then placed in the corpectomy defect, and the traction was then released. The anterior cervical locking plate was stabilized on the body of the adjacent vertebra with stabilizing pins, and its position was confirmed on the image intensifier. When the position was correct, the anterior cervical locking plate was stabilized with a variable unicortical locking screw. The position of the screw was again confirmed using the image intensifier on both anteroposterior and lateral views. Finally, the locking screws were tightened. Wound closure was done in layers over a negative suction drain, and an antiseptic dressing and Philadelphia collar were applied. During surgery, the status of the disc, anterior longitudinal ligament, and posterior longitudinal ligament was assessed. Surgical wound closure was done in layers over a negative suction drain. Postoperatively, all patients were mobilized with a Philadelphia collar as soon as possible, by the first to second day. The first wound dressing with removal of the drain was performed on the second postoperative day. Postoperatively, routine anteroposterior and lateral views of the cervical spine were obtained to assess the placement of the cervical locking plate and cage (Figs. 1, 2). The negative suction drain was removed on the second postoperative day after wound inspection.
The patients enrolled in our study were followed up for a mean of 17 months (range, 12–48 months). Patients were evaluated after 6 weeks, then at intervals of 3 months for the first 6 months and yearly thereafter. Static cervical exercises were advised after surgery. Cervical movements were allowed at 6 weeks. At follow-up, a detailed clinical and neurological examination was performed, and a radiological assessment was done. Fusion of the graft was assessed on plain radiographs, using the Bridwell fusion grade after 6 months and at 1 year, and then yearly thereafter. Neck-specific disability was measured using the Neck Disability Index (NDI) after 6 months and at 1 year postoperatively [6].
In our study, 23 patients underwent 2-level anterior cervical corpectomy and fusion, of whom 20 (86.9%) were male and 3 (13.1%) were female. All patients had pain in the neck and during neck movements. Nineteen patients had a neurological deficit (ASIA grade D, 56.52%; ASIA grade C, 26.09%). C5 and C6 corpectomies were done in 52.18% of patients, C4 and C5 corpectomies were performed in 39.14% of patients, C6 and C7 corpectomies were done in 4.34% of patients, and C3 and C4 corpectomies were performed in 4.34% of patients. Similarly, C4–5, C5–6, and C6–7 were the most common discectomy levels (52.18%). Intraoperatively, in 43.48% of cases, a prolapsed disc was observed, degenerated discs were found in 34.79% of patients, and 21.73% had ruptured discs. The anterior longitudinal ligament was disrupted in 56.52% of patients, and the posterior longitudinal ligament was found to have ruptured in 65.21% (Table 1). No intraoperative complications, such as injury to the trachea and oesophagus, bleeding and haematoma collection, or laryngeal nerve injury, were observed. No patients received a blood transfusion. All patients had transient dysphagia, which was assessed in the postoperative period; in such cases, patients complained of difficulty consuming solid food on the first postoperative day, but dysphagia resolved completely within 1 week. No patients had wound infection (Table 2). All patients experienced relief of axial pain, as assessed using a visual analogue scale. Four patients did not have a neurological deficit (ASIA grade E), and 18 patients showed neurological improvements in the postoperative period (ASIA grade E, 34.78%; ASIA grade D, 43.48%), while 1 patient did not show neurological recovery (ASIA grade C). However, none of the patients deteriorated neurologically in the postoperative period. Fusion of the graft was assessed radiologically according to the Bridwell fusion grading system (grade I, 69.56%; grade II, 21.73%; and grade III, 8.69%). No complications related to the cages or plates were observed. Pseudarthrosis was asymptomatic and not associated with implant-related complications (Table 3). Over the course of follow-up, the NDI score slowly decreased, and at the final follow-up, 73.93% patients had an NDI between 5% and 14%, 13.04% had an NDI between 0% and 4%, 4.34% had an NDI between 15% and 24%, 8.69% had an NDI between 25% and 34%, and none of the patients had an NDI above 34%.
The subaxial cervical spine has considerable mobility and close proximity to the more rigid thoracic region, making it prone to traumatic disruption. Subaxial cervical spine injuries are often misdiagnosed, which can lead to devastating events such as quadriplegia and severe permanent disability [7].
After stabilization of the patient, cervical spine injury screening should be done. The screening mainly depends on the resources available at the institution. Conventionally, the standard radiographic views for the cervical spine are anteroposterior, lateral, and open mouth views to evaluate the spine from the craniocervical junction to T1 (sensitivity, 70%). CT scans with coronal and sagittal views, as well as 3-dimensional reconstruction, provide detailed information about the cervical spine. CT allows excellent visualization of the craniocervical and cervicothoraxic junction (sensitivity, 99%; specificity, 100%). Overall, CT scans provide excellent resolution for bone, and can clearly visualize cervical spine injuries [8].
However, magnetic resonance imaging is a promising technology for assessing the discoligamentous complex, soft tissue injuries, and haematomas, which are important for surgical planning. However, the clinical evaluation of patients with a cervical spine injury is of paramount importance, despite advances in imaging modalities [9].
Many systems have been proposed to classify subaxial cervical spine trauma. One of the most commonly used is the Allen and Ferguson classification, but it does not take into account critical variables, such as ligamentous and neurological injuries, and it has high intraobserver variability. Based on these potential weaknesses, the Spinal Trauma Study Group proposed a new classification system, the SLIC (Table 4). This system is based on 3 major characteristics that should be taken into account in the decision-making process: (1) injury morphology, (2) integrity of the discoligamentous complex, and (3) the neurological status of the patient. Each of these 3 factors is classified in isolation, with a final score resulting from the summation of these 3 variables. The system recommends treatment based on the final severity score. A score of fewer than 4 points supports conservative treatment, while a score of 5 or more points supports surgical treatment. A patient with a score of 4 points may be treated conservatively or surgically, depending on the surgeon’s experience, the patient’s preference, and additional comorbid conditions [5]. Subaxial spine trauma management ranges from conservative to cervical orthosis to surgery. Operative management has been described using both the anterior and posterior approach, with stabilization done anteriorly, posteriorly, or combined. The anterior approach is less traumatic and enables decompression, reduction of dislocated facet joints, interbody grafting with reconstruction, and maintenance of lordosis. Although fusion rates are high with the use of an autograft, autografts are associated with significant graft site morbidity, whereas the use of allografts, which are devoid of any donor site problems, is associated with high rates of pseudarthrosis, a slower rate of fusion, and a higher likelihood of infection. To overcome these problems associated with both allografts and autografts, titanium mesh cages filled with local bone saved from corpectomy can be used. These cages have the advantages of immediate anterior column stability, a shorter operation time, maintenance of intervertebral disc height and lordotic angle, avoidance of morbidity associated with autologous bone graft (iliac crest) harvesting, good biocompatibility, and a comparable fusion rate to that obtained using autogenous tricortical iliac bone [3,10].
Although multiple discectomies are an alternative means of decompression in cases associated with posttraumatic prolapsed intervertebral discs, corpectomy addresses spinal canal stenosis due to degenerative spondylotic changes, and the fusion rate is higher, since only 2 fusion surfaces are present [11,12].
In contrast, the posterior approach may be injurious to adjacent levels. Such injuries have been postulated to cause late deformities, with concerns regarding the rate of wound infection and the inability to address a disrupted disc prior to reduction [13].
We used a left-sided approach in order to reduce the risk to the recurrent laryngeal nerve. On the left, the nerve enters the thorax within the carotid sheath, loops under the aortic arch, and ascends into the neck next to the trachea and oesophagus, whereas on the right side, it leaves the carotid sheath at a higher level and courses anteriorly behind the thyroid. Blunt dissection using a finger and blunt artery forceps is key to decrease soft tissue trauma.
In the postoperative period, dysphagia is a very common complication associated with the anterior approach; however, it usually resolves spontaneously within 2–3 days [14]. Postoperative dysphagia may be due to endotracheal intubation, retraction of the oesophagus, and soft tissue inflammation. Preoperative systemic steroid treatment leads to a reduction of dysphagia severity, with no increase in infectious complications [15]. During this period, a liquid diet and gargling with lukewarm water are advised. Tasiou et al. [16] reported soft tissue haematoma in 2 of 114 patients, and we placed a negative suction drain in all anterior cervical surgical procedures as a standard protocol to prevent the development of haematoma. Such drains are also helpful for detecting cerebrospinal fluid leaks, although we did not encounter this complication in our study.
Subaxial spine trauma management is continuously evolving. The widespread availability of high-resolution multiplanar CT has enabled improved diagnostic accuracy and efficiency, while also allowing for early surgical interventions, which have been shown to result in improved outcomes in the setting of spinal cord injury. In addition, although the SLIC classification system has shown some promise in its reliability and reproducibility in diagnosing fractures and guiding management, its use has not become universal due to disagreements regarding the morphological classification of injuries. In general, subaxial cervical spine injuries are typically complex, and standardization of treatment is not always feasible. The surgeon must consider in each case not only the subaxial injury itself, but also an individual patient’s comorbidities, the surgeon’s experience, and the available resources when determining the most appropriate management strategy.
In our experience, 2-level anterior cervical corpectomy and fusion with a cervical locking plate and autologous bone-filled titanium mesh cage is a feasible and safe method for treating subaxial spine injuries for which 2-level corpectomy is indicated. It has the benefits of high primary stability, anatomical reduction, and direct decompression of the spinal cord. Solid fusion with good functional outcomes, combined with a low rate of complications, was achieved in all cases following anterior cervical decompression, fusion, and stabilization with a cervical locking plate and autologous bone-filled titanium mesh cage. A randomized trial of longer duration with a greater number of patients would be more appropriate for obtaining definitive conclusions, and this is the main limitation of our study.
Fig. 1.
Allen and Ferguson classification – vertical compression injury: preoperative radiographs (A, B), preoperative computed tomography scan (sagital section) (C), and postoperative radiographs (D, E).

Fig. 2.
Allen and Ferguson classification – compressive flexion injury: preoperative radiographs (A, B), preoperative sagital and axial sections of computed tomography scan (C, D), postpoperative radiographs (E, F).
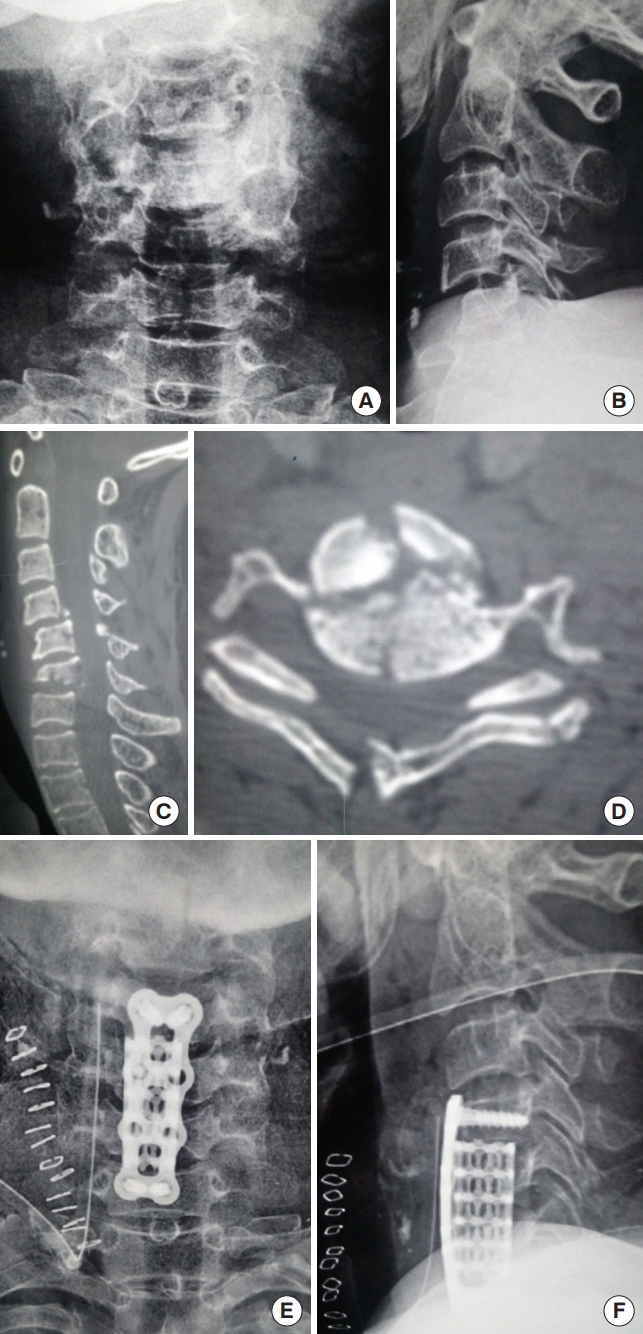
Table 1.
Patient characteristics, injury pattern and outcome
| No. | Age (yr) | Sex | Mode of trauma | Allen and Ferguson classification | SLIC score | Preop ASIA grade | Intraoperative disc status | ALL status | PLL status | Corpectomy level | Postoperative ASIA grade | Neck Disability Index at final follow-up (%) | Bridwell fusion grade |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 30 | M | Fall* | Distractive extension | 6 | D | Degenerated | Torn | Intact | C4, C5 | E | 17 | 1 |
| 2 | 50 | M | Fall* | Compressive extension | 6 | E | Prolapsed | Intact | Torn | C5, C6 | E | 5.5 | 1 |
| 3 | 55 | M | Fall* | Distractive extension | 6 | C | Prolapsed | Torn | Intact | C4, C5 | D | 12 | 1 |
| 4 | 54 | M | Fall* | Distractive extension | 6 | E | Prolapsed | Torn | Torn | C4, C5 | E | 4 | 1 |
| 5 | 38 | M | Fall* | Vertical compression | 8 | D | Ruptured | Torn | Torn | C6, C7 | E | 4 | 2 |
| 6 | 59 | F | Fall* | Distractive extension | 6 | D | Prolapsed | Torn | Torn | C5, C6 | E | 10 | 1 |
| 7 | 54 | F | Fall* | Distractive flexion | 10 | D | Ruptred | Torn | Torn | C5, C6 | D | 8.5 | 2 |
| 8 | 17 | M | RSA | Vertical compression | 8 | D | Ruptured | Intact | Torn | C4, C5 | E | 2 | 1 |
| 9 | 67 | M | RSA | Distractive extension | 9 | C | Degenerated | Torn | Torn | C5, C6 | D | 5 | 1 |
| 10 | 53 | M | RSA | Compressive extension | 6 | C | Degenerated | Torn | Intact | C5, C6 | D | 26 | 1 |
| 11 | 43 | M | Fall* | Distractive extension | 6 | D | Prolapsed | Torn | Intact | C5, C6 | E | 7 | 1 |
| 12 | 75 | M | Fall* | Distractive extension | 6 | D | Degenerated | Torn | Intact | C4, C5 | E | 7.5 | 1 |
| 13 | 64 | M | Fall* | Compressive flexion | 6 | E | Degenerated | Intact | Torn | C5, C6 | E | 9.5 | 1 |
| 14 | 57 | M | Fall* | Compressive flexion | 9 | D | Ruptured | Torn | Torn | C4, C5 | D | 5.5 | 1 |
| 15 | 48 | M | Fall* | Lateral flexion | 6 | D | Prolapsed | Intact | Intact | C3, C4 | D | 8.5 | 2 |
| 16 | 50 | M | Fall* | Compressive flexion | 7 | D | Ruptured | Intact | Torn | C4, C5 | E | 11 | 2 |
| 17 | 64 | M | Fall* | Compressive extension | 6 | D | Degenerated | Intact | Intact | C4, C5 | D | 10.5 | 3 |
| 18 | 60 | M | Fall* | Distractive flexion | 9 | C | Degenrated | Intact | Torn | C3, C4 | C | 25.5 | 3 |
| 19 | 40 | M | Fall* | Distractive flexion | 6 | D | Prolapsed | Intact | Torn | C5, C6 | D | 7.5 | 2 |
| 20 | 40 | M | Fall* | Vertical compression | 6 | D | Degenerated | Intact | Torn | C4, C5 | D | 6.5 | 1 |
| 21 | 19 | M | RSA | Distractive extension | 6 | C | Prolapsed | Torn | Torn | C5, C6 | E | 8.5 | 1 |
| 22 | 30 | F | Fall* | Compressive extension | 6 | E | Prolapsed | Intact | Torn | C5 ,C6 | E | 5.5 | 1 |
| 23 | 55 | M | Fall* | Distractive extension | 6 | C | Prolapsed | Torn | Intact | C5 ,C6 | D | 12 | 1 |
Table 2.
Complications following surgery (n=23)
| Variable | Percentage |
|---|---|
| Dysphagia | 100 |
| Radiculopathy | 0 |
| Cerebrospinal fluid leak | 0 |
| Surgical site infection | 0 |
| Postoperative bleeding/haematoma | 0 |
| Laryngeal nerve injury | 0 |
Table 3.
Outcomes of the patients in this study (n=23)
| Variable | Percentage |
|---|---|
| Neurological recovery | 78.21 |
| Axial pain relief | 100 |
| Fusion | |
| Grade I | 69.56 |
| Grade II | 21.73 |
| Pseudarthrosis | 8.69 |
| Implant failure | 0 |
Table 4.
Subaxial cervical spine injury classification scale
REFERENCES
2. Joaquim AF, Lawrence B, Daubs M, et al. Evaluation of the subaxial injury classification system. J Craniovertebr Junction Spine 2011 2:67-72.



3. Park HW, Lee JK, Moon SJ, et al. The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976) 2009 34:E591-5.


4. Aarabi B, Walters BC, Dhall SS, et al. Subaxial cervical spine injury classification systems. Neurosurgery 2013 72 Suppl 2:170-86.



5. Vaccaro AR, Hulbert RJ, Patel AA, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007 32:2365-74.


6. Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 1991 14:409-15.

7. Joaquim AF, Patel A. Occipito-cervical trauma: evaluation, classification and treatment. Contemp Neurosurg 2010 32:1-6.



8. Schenarts PJ, Diaz J, Kaiser C, et al. Prospective comparison of admission computed tomographic scan and plain films of the upper cervical spine in trauma patients with altered mental status. J Trauma 2001 51:663-8.


9. Kaiser ML, Whealon MD, Barrios C, et al. The current role of magnetic resonance imaging for diagnosing cervical spine injury in blunt trauma patients with negative computed tomography scan. Am Surg 2012 78:1156-60.


10. Wang JC, McDonough PW, Endow KK, et al. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2000 25:41-5.



11. Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993 75:1298-307.


12. Cauthen JC, Kinard RE, Vogler JB, et al. Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine (Phila Pa 1976) 1998 23:188-92.


13. Koller H, Reynolds J, Zenner J, et al. Mid- to long-term outcome of instrumented anterior cervical fusion for subaxial injuries. Eur Spine J 2009 18:630-53.



14. Jain V, Thakur MK, Thakur A, et al. Functional outcome in unstable Hangman's fracture managed with anterior approach: a prospective study. J Craniovertebr Junction Spine 2017 8:350-3.




- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























