 |
 |
- Search
|
|
||
Abstract
Objective
Methods
Results
Conclusion
ACKNOWLEDGEMENTS
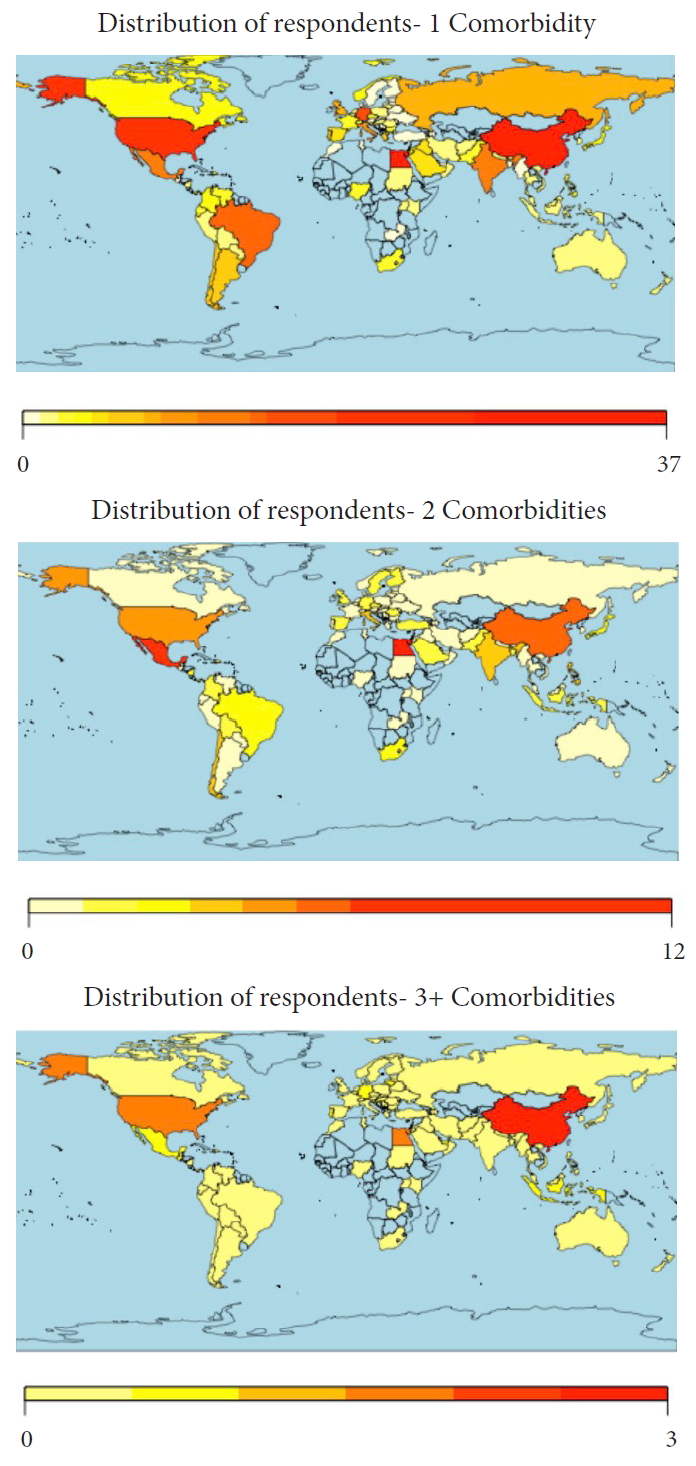
Fig.┬Ā1.
Table┬Ā1.
| Variable |
Overall |
Africa |
Asia |
Australia |
Europe |
Middle East |
North America |
South America/Latin America |
p-value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |||
| Age (yr) | ||||||||||||||||||
| ŌĆā | 25ŌĆō34 | 127 | 14.4 | 5 | 11.4 | 28 | 13.2 | 0 | 0.0 | 29 | 12.0 | 16 | 20.8 | 28 | 18.5 | 21 | 14.5 | 0.017* |
| 35ŌĆō44 | 338 | 38.4 | 21 | 47.7 | 66 | 31.0 | 1 | 12.5 | 97 | 40.1 | 25 | 32.5 | 63 | 41.7 | 65 | 44.8 | ||
| 45ŌĆō54 | 241 | 27.4 | 11 | 25.0 | 73 | 34.3 | 3 | 37.5 | 66 | 27.3 | 22 | 28.6 | 32 | 21.2 | 34 | 23.5 | ||
| 55ŌĆō64 | 149 | 16.9 | 5 | 11.4 | 44 | 20.7 | 4 | 50.0 | 42 | 17.4 | 14 | 18.2 | 20 | 13.3 | 20 | 13.8 | ||
| 65+ | 25 | 2.8 | 2 | 4.6 | 2 | 0.9 | 0 | 0.0 | 8 | 3.3 | 0 | 0.0 | 8 | 5.3 | 5 | 3.5 | ||
| Sex | ||||||||||||||||||
| Male | 812 | 93.8 | 42 | 100.0 | 203 | 95.8 | 8 | 100.0 | 213 | 91.0 | 74 | 96.1 | 140 | 94.0 | 132 | 91.7 | 0.144 | |
| Female | 54 | 6.2 | 0.0 | 0.0 | 9 | 4.3 | 0 | 0.0 | 21 | 9.0 | 3 | 3.9 | 9 | 6.0 | 12 | 8.3 | ||
| Specialty | ||||||||||||||||||
| Orthopaedics | 625 | 71 | 35 | 79.6 | 178 | 83.6 | 5 | 62.5 | 151 | 62.4 | 54 | 71.1 | 115 | 75.7 | 87 | 60.0 | < 0.001* | |
| Neurosurgery | 244 | 27.7 | 8 | 18.2 | 36 | 16.9 | 2 | 25.0 | 85 | 35.1 | 19 | 25.0 | 38 | 25.0 | 56 | 38.6 | ||
| Trauma | 102 | 11.6 | 5 | 11.4 | 18 | 8.5 | 0 | 0.0 | 54 | 22.3 | 9 | 11.8 | 2 | 1.3 | 14 | 9.7 | ||
| Other | 52 | 5.9 | 2 | 4.6 | 13 | 6.1 | 2 | 25.0 | 18 | 7.4 | 8 | 10.5 | 4 | 2.6 | 5 | 3.5 | ||
| Practice type | ||||||||||||||||||
| Academic/private combined | 198 | 22.5 | 13 | 29.6 | 29 | 13.6 | 4 | 50.0 | 47 | 19.4 | 28 | 36.4 | 23 | 15.1 | 54 | 37.2 | < 0.001* | |
| Academic | 400 | 45.4 | 20 | 45.5 | 127 | 59.6 | 1 | 12.5 | 115 | 47.5 | 23 | 29.9 | 91 | 59.9 | 23 | 15.9 | ||
| Private | 142 | 16.1 | 7 | 15.9 | 26 | 12.2 | 1 | 12.5 | 20 | 8.3 | 15 | 19.5 | 30 | 19.7 | 43 | 29.7 | ||
| Public/local hospital | 137 | 15.6 | 4 | 9.1 | 30 | 14.1 | 2 | 25.0 | 59 | 24.4 | 11 | 14.3 | 7 | 4.6 | 24 | 16.6 | ||
| Comorbidity | ||||||||||||||||||
| Obesity | 102 | 15.6 | 7 | 24.1 | 23 | 15.5 | 0 | 0.0 | 26 | 13.9 | 16 | 31.4 | 8 | 6.3 | 22 | 20.8 | < 0.001* | |
| Hypertension | 155 | 21.9 | 10 | 31.3 | 36 | 22.4 | 0 | 0.0 | 34 | 17.4 | 18 | 34.0 | 20 | 14.3 | 37 | 30.6 | 0.003* | |
| Current tobacco use | 75 | 11.9 | 2 | 8.3 | 32 | 20.4 | 0 | 0.0 | 23 | 12.5 | 7 | 16.7 | 2 | 1.6 | 9 | 9.7 | < 0.001* | |
| Respiratory illness | 35 | 6.0 | 3 | 12.0 | 5 | 3.9 | 1 | 14.3 | 9 | 5.3 | 2 | 5.4 | 6 | 4.8 | 9 | 9.7 | 0.390 | |
| Renal disease | 5 | 0.9 | 1 | 4.4 | 2 | 1.6 | 0 | 0.0 | 1 | 0.6 | 0 | 0.0 | 1 | 0.8 | 0 | 0.0 | 0.541 | |
| Cancer | 4 | 0.7 | 0 | 0.0 | 2 | 1.6 | 0 | 0.0 | 1 | 0.6 | 0 | 0.0 | 1 | 0.8 | 0 | 0.0 | 0.878 | |
| Cardiac disease | 25 | 4.3 | 3 | 12.0 | 4 | 3.1 | 1 | 14.3 | 7 | 4.2 | 2 | 5.4 | 3 | 2.4 | 5 | 5.6 | 0.300 | |
| Diabetes | 44 | 7.4 | 5 | 18.5 | 19 | 13.2 | 0 | 0.0 | 3 | 1.8 | 9 | 20.5 | 2 | 1.6 | 6 | 6.7 | < 0.001* | |
| 1 Comorbidity | 250 | 31.1 | 15 | 40.5 | 68 | 35.2 | 2 | 25.0 | 65 | 28.8 | 31 | 47.0 | 24 | 16.7 | 45 | 34.9 | < 0.001* | |
| 2 Comorbidities | 63 | 10.2 | 6 | 21.4 | 15 | 10.7 | 0 | 0.0 | 12 | 6.9 | 10 | 22.2 | 6 | 4.8 | 14 | 14.3 | 0.003* | |
| 3+ Comorbidities | 15 | 2.6 | 1 | 4.4 | 5 | 3.9 | 0 | 0.0 | 4 | 2.4 | 1 | 2.8 | 2 | 1.6 | 2 | 2.3 | 0.945 | |
| No comorbidities | 553 | 62.8 | 22 | 50.0 | 125 | 58.7 | 6 | 75.0 | 161 | 66.5 | 35 | 45.5 | 120 | 79.0 | 84 | 57.9 | < 0.001* | |
Table┬Ā2.
| Variable |
Obesity |
Hypertension |
Current tobacco use |
Respiratory illness |
Renal disease |
Cancer |
Cardiac disease |
Diabetes |
1 Comorbidity |
2 Comorbidities |
3+ Comorbidities |
No comorbidities |
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | ||
| COVID-19 diagnosis | |||||||||||||||||||||||||||||||||||||
| ŌĆā | Know someone diagnosed | 41 | 14.2 | 0.519 | 72 | 22.5 | 0.469 | 35 | 12.4 | 0.356 | 16 | 6.1 | 0.562 | 1 | 0.4 | 0.916 | 1 | 0.4 | 0.916 | 9 | 3.5 | 0.621 | 15 | 5.7 | 0.345 | 112 | 31.1 | 0.573 | 26 | 9.5 | 0.517 | 6 | 2.4 | 0.798 | 248 | 63.3 | 0.792 |
| Personally diagnosed | 3 | 37.5 | 0.079 | 1 | 16.7 | 0.781 | 1 | 16.7 | 0.665 | 0 | 0.0 | 0.592 | 0 | 0.0 | 0.892 | 0 | 0.0 | 0.892 | 1 | 16.7 | 0.116 | 0 | 0.0 | 0.547 | 3 | 37.5 | 0.647 | 0 | 0.0 | 0.448 | 1 | 16.7 | 0.020* | 5 | 55.6 | 0.608 | |
| COVID-19 testing | |||||||||||||||||||||||||||||||||||||
| Know how to get tested | 74 | 14.2 | 0.067 | 122 | 21.4 | 0.943 | 55 | 11.0 | 0.626 | 26 | 5.5 | 0.927 | 1 | 0.2 | 0.210 | 2 | 0.5 | 0.526 | 17 | 3.7 | 0.245 | 33 | 6.9 | 0.824 | 199 | 30.8 | 0.532 | 45 | 9.2 | 0.038* | 10 | 2.2 | 0.548 | 447 | 63.8 | 0.699 | |
| Personally tested | 6 | 13.0 | 0.641 | 7 | 14.9 | 0.254 | 1 | 2.4 | 0.065 | 3 | 7.0 | 0.648 | 0 | 0.0 | 0.688 | 0 | 0.0 | 0.688 | 2 | 4.8 | 0.824 | 2 | 4.8 | 0.590 | 13 | 24.5 | 0.339 | 4 | 9.1 | 0.776 | 0 | 0.0 | 0.307 | 40 | 70.2 | 0.277 | |
| Reason for testing | |||||||||||||||||||||||||||||||||||||
| Direct contact with COVID-19 positive patient | 4 | 30.8 | 0.448 | 6 | 27.3 | 0.210 | 1 | 10.0 | 0.050 | 1 | 25.0 | 0.503 | - | - | - | 1 | 2.7 | 0.242 | 3 | 7.7 | 0.696 | 2 | 5.3 | 0.492 | 8 | 18.2 | 0.013* | 5 | 12.2 | 0.820 | - | - | - | 36 | 73.5 | 0.045 | |
| Prophylactic | 2 | 15.4 | 0.300 | 1 | 4.6 | 0.679 | 2 | 20.0 | 0.158 | 0 | 0.0 | 0.585 | - | - | - | 0 | 0.0 | 0.784 | 1 | 14.3 | 0.387 | 1 | 14.3 | 0.481 | 5 | 45.5 | 0.328 | 1 | 14.3 | 0.799 | - | - | - | 6 | 50.0 | 0.357 | |
| Demonstrated symptoms | 6 | 46.2 | 0.918 | 11 | 50.0 | 0.846 | 6 | 60.0 | 0.461 | 3 | 75.0 | 0.285 | - | - | - | 0 | 0.0 | 0.342 | 2 | 4.7 | 0.496 | 2 | 4.7 | 0.330 | 24 | 36.9 | 0.252 | 3 | 6.8 | 0.201 | - | - | - | 41 | 60.3 | 0.629 | |
| Ask to be tested | 1 | 7.7 | 0.473 | 4 | 18.2 | 0.012* | 1 | 10.0 | 0.329 | 0 | 0.0 | 0.704 | - | - | - | 0 | 0.0 | 0.849 | 0 | 0.0 | 0.642 | 2 | 40.0 | 0.005 | 4 | 57.1 | 0.148 | 2 | 40.0 | 0.038* | - | - | - | 3 | 33.3 | 0.063 | |
| Current stressors | |||||||||||||||||||||||||||||||||||||
| Personal health | 49 | 50.0 | 0.035* | 78 | 53.1 | 0.002* | 27 | 39.7 | 0.866 | 15 | 48.4 | 0.280 | 1 | 50.0 | 0.742 | 2 | 100.0 | 0.076 | 16 | 69.6 | 0.003* | 17 | 7.6 | 0.541 | 110 | 47.0 | 0.030* | 37 | 59.7 | 0.001* | 5 | 38.5 | 0.989 | 206 | 57.5 | 0.003* | |
| Family health | 76 | 77.6 | 0.597 | 115 | 78.2 | 0.425 | 50 | 73.5 | 0.786 | 25 | 80.7 | 0.482 | 2 | 100.0 | 0.415 | 1 | 50.0 | 0.415 | 20 | 87.0 | 0.193 | 28 | 7.2 | 0.908 | 184 | 78.6 | 0.283 | 46 | 74.2 | 0.883 | 10 | 76.9 | 0.877 | 362 | 62.6 | 0.868 | |
| Community health | 36 | 36.7 | 0.120 | 61 | 41.5 | 0.422 | 34 | 50.0 | 0.456 | 9 | 29.0 | 0.078 | 1 | 50.0 | 0.892 | 1 | 50.0 | 0.892 | 13 | 56.5 | 0.287 | 22 | 8.4 | 0.176 | 92 | 39.3 | 0.129 | 30 | 48.4 | 0.635 | 7 | 53.9 | 0.537 | 241 | 65.1 | 0.328 | |
| Hospital capacity | 44 | 44.9 | 0.573 | 65 | 44.2 | 0.605 | 26 | 38.2 | 0.570 | 11 | 35.5 | 0.485 | 0 | 0.0 | 0.231 | 1 | 50.0 | 0.815 | 8 | 34.8 | 0.501 | 11 | 4.7 | 0.095 | 99 | 42.3 | 0.904 | 27 | 43.6 | 0.796 | 3 | 23.1 | 0.175 | 223 | 63.4 | 0.979 | |
| Timeline to resume clinical practice | 41 | 41.8 | 0.218 | 55 | 37.4 | 0.016* | 29 | 42.7 | 0.355 | 11 | 35.5 | 0.156 | 0 | 0.0 | 0.170 | 2 | 100.0 | 0.147 | 10 | 43.5 | 0.631 | 14 | 5.1 | 0.125 | 88 | 37.6 | 0.005* | 23 | 37.1 | 0.086 | 8 | 61.5 | 0.356 | 259 | 68.5 | 0.005* | |
| Government/leadership | 19 | 19.4 | 0.988 | 22 | 15.0 | 0.227 | 13 | 19.1 | 0.968 | 7 | 22.6 | 0.656 | 0 | 0.0 | 0.489 | 0 | 0.0 | 0.489 | 6 | 26.1 | 0.424 | 6 | 5.5 | 0.545 | 36 | 15.4 | 0.192 | 12 | 19.4 | 0.995 | 3 | 23.1 | 0.735 | 103 | 66.9 | 0.308 | |
| Return to nonessential activities | 11 | 11.2 | 0.450 | 22 | 15.0 | 0.784 | 10 | 14.7 | 0.888 | 4 | 12.9 | 0.855 | 0 | 0.0 | 0.567 | 2 | 100.0 | 0.001* | 3 | 13.0 | 0.889 | 4 | 5.1 | 0.505 | 31 | 13.3 | 0.761 | 7 | 11.3 | 0.548 | 3 | 23.1 | 0.359 | 75 | 64.7 | 0.745 | |
| Economic issues | 43 | 43.9 | 0.513 | 62 | 42.2 | 0.255 | 29 | 42.7 | 0.453 | 21 | 67.7 | 0.028* | 0 | 0.0 | 0.180 | 1 | 50.0 | 0.943 | 13 | 56.5 | 0.395 | 13 | 4.9 | 0.088 | 95 | 40.6 | 0.079 | 32 | 51.6 | 0.536 | 5 | 38.5 | 0.520 | 253 | 65.7 | 0.182 | |
| Other | 0 | 0.0 | 0.222 | 0 | 0.0 | 0.135 | 0 | 0.0 | 0.309 | 1 | 3.2 | 0.456 | 0 | 0.0 | 0.861 | 1 | 50.0 | < 0.001* | 0 | 0.0 | 0.554 | 1 | 11.1 | 0.607 | 3 | 1.3 | 0.814 | 0 | 0.0 | 0.331 | 0 | 0.0 | 0.656 | 8 | 72.7 | 0.514 | |
| Media perceptions | |||||||||||||||||||||||||||||||||||||
| Accurate coverage | 35 | 35.7 | 0.041* | 73 | 50.0 | 0.394 | 35 | 51.5 | 0.881 | 13 | 41.9 | 0.416 | 1 | 50.0 | 0.775 | 1 | 100.0 | 0.590 | 9 | 39.1 | 0.601 | 18 | 6.5 | 0.691 | 119 | 51.3 | 0.052 | 26 | 41.9 | 0.595 | 3 | 23.1 | 0.180 | 259 | 63.6 | 0.181 | |
| Excessive coverage | 53 | 54.1 | 54 | 37.0 | 21 | 30.9 | 14 | 45.2 | 1 | 50.0 | 0 | 0.0 | 10 | 43.5 | 12 | 6.3 | 88 | 37.9 | 23 | 37.1 | 7 | 53.9 | 180 | 60.4 | |||||||||||||
| Not enough coverage | 18 | 18.4 | 19 | 13.0 | 12 | 17.7 | 4 | 12.9 | 0 | 0.0 | 0 | 0.0 | 4 | 17.4 | 9 | 8.7 | 25 | 10.8 | 13 | 21.0 | 3 | 23.1 | 94 | 69.6 | |||||||||||||
| Current media sources | |||||||||||||||||||||||||||||||||||||
| International news - internet | 22 | 25.0 | 0.663 | 30 | 21.0 | 0.023* | 20 | 31.3 | 0.693 | 6 | 20.0 | 0.971 | 0 | 0.0 | 0.856 | 1 | 50.0 | 0.018* | 1 | 4.6 | 0.082 | 9 | 6.4 | 0.110 | 58 | 27.1 | 0.496 | 10 | 16.4 | 0.005* | 3 | 23.1 | 0.277 | 131 | 64.9 | 0.238 | |
| International news - television | 8 | 9.1 | 17 | 11.9 | 5 | 7.8 | 3 | 10.0 | 0 | 0.0 | 0 | 0.0 | 3 | 13.6 | 3 | 6.4 | 17 | 7.9 | 11 | 18.0 | 0 | 0.0 | 44 | 61.1 | |||||||||||||
| National/local news - internet | 25 | 28.4 | 29 | 20.3 | 20 | 31.3 | 11 | 36.7 | 1 | 50.0 | 0 | 0.0 | 6 | 27.3 | 6 | 3.8 | 55 | 25.7 | 11 | 18.0 | 5 | 38.5 | 153 | 68.3 | |||||||||||||
| National/local news - television | 21 | 23.9 | 43 | 30.1 | 9 | 14.1 | 6 | 20.0 | 1 | 50.0 | 0 | 0.0 | 9 | 40.9 | 9 | 8.0 | 49 | 22.9 | 23 | 37.7 | 1 | 7.7 | 104 | 58.8 | |||||||||||||
| Newspaper | 1 | 1.1 | 6 | 4.2 | 2 | 3.1 | 1 | 3.3 | 0 | 0.0 | 1 | 50.0 | 0 | 0.0 | 3 | 15.0 | 9 | 4.2 | 1 | 1.6 | 1 | 7.7 | 17 | 60.7 | |||||||||||||
| Social media | 11 | 12.5 | 18 | 12.6 | 8 | 12.5 | 3 | 10.0 | 0 | 0.0 | 0 | 0.0 | 3 | 13.6 | 21 | 15.3 | 26 | 12.2 | 5 | 8.2 | 3 | 23.1 | 41 | 54.7 | |||||||||||||
| Quarantined | 21 | 15.7 | 0.945 | 41.0 | 26.6 | 0.068 | 21 | 15.7 | 0.945 | 10.0 | 8.1 | 0.144 | 1 | 0.9 | 0.319 | 2 | 1.7 | 0.007* | 3 | 2.6 | 0.350 | 12 | 9.6 | 0.159 | 60 | 34.7 | 0.149 | 16 | 12.4 | 0.396 | 4 | 3.4 | 0.402 | 113 | 58.6 | 0.101 | |
| Perception of hospital effectiveness | |||||||||||||||||||||||||||||||||||||
| Acceptable/appropriate | 46 | 52.3 | 0.216 | 86 | 60.1 | 0.570 | 31 | 48.4 | 0.188 | 18 | 60.0 | 0.283 | 0 | 0.0 | 0.141 | 2 | 100.0 | 0.750 | 12 | 54.6 | 0.430 | 24 | 7.3 | 0.406 | 136 | 63.6 | 0.758 | 31 | 50.8 | 0.322 | 6 | 46.2 | 0.464 | 304 | 63.7 | 0.772 | |
| Excessive/unnecessary | 3 | 3.4 | 2 | 1.4 | 2 | 3.1 | 1 | 3.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 1.4 | 1 | 1.6 | 1 | 7.7 | 12 | 70.6 | |||||||||||||
| Disarray/disorganized | 13 | 14.8 | 10 | 7.0 | 9 | 14.1 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 4 | 18.2 | 1 | 2.3 | 16 | 7.5 | 7 | 11.5 | 2 | 15.4 | 43 | 63.2 | |||||||||||||
| Not enough action | 26 | 29.6 | 45 | 31.5 | 22 | 34.4 | 11 | 36.7 | 2 | 100.0 | 0 | 0.0 | 6 | 27.3 | 12 | 8.5 | 59 | 27.6 | 22 | 36.1 | 4 | 30.8 | 130 | 60.5 | |||||||||||||
| Perception of government effectiveness | |||||||||||||||||||||||||||||||||||||
| Acceptable/appropriate | 53 | 60.2 | 0.711 | 79 | 55.2 | 0.627 | 37 | 57.8 | 0.849 | 21 | 70.0 | 0.445 | 1 | 50.0 | 0.899 | 2 | 100.0 | 0.673 | 14 | 63.6 | 0.179 | 23 | 7.7 | 0.476 | 143 | 66.8 | 0.064 | 29 | 47.5 | 0.438 | 7 | 53.9 | 0.156 | 277 | 60.8 | 0.409 | |
| Excessive/unnecessary | 1 | 1.1 | 4 | 2.8 | 3 | 4.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 4 | 1.9 | 2 | 3.3 | 0 | 0.0 | 14 | 70.0 | |||||||||||||
| Disarray/disorganized | 11 | 12.5 | 22 | 15.4 | 7 | 10.9 | 3 | 10.0 | 0 | 0.0 | 0 | 0.0 | 5 | 22.7 | 2 | 3.5 | 22 | 10.3 | 6 | 9.8 | 4 | 30.8 | 56 | 63.6 | |||||||||||||
| Not enough action | 23 | 26.1 | 38 | 26.6 | 17 | 26.6 | 6 | 20.0 | 1 | 50.0 | 0 | 0.0 | 3 | 13.6 | 12 | 7.7 | 45 | 21.0 | 24 | 39.3 | 2 | 15.4 | 144 | 67.0 | |||||||||||||
Calculation of p-values was performed using a combination of chi-square and Fisher exact tests.
Comparisons are made between respondents with comorbidities and healthy individuals. Clinicians with no comorbidities were compared to those with one or more comorbidity. All percentages are calculated based upon the total number of responses received for each question and comorbidity combination.
COVID-19, coronavirus disease 2019.
Table┬Ā3.
| Variable |
Obesity |
Hypertension |
Current tobacco use |
Respiratory illness |
Renal disease |
Cancer |
Cardiac disease |
Diabetes |
1 Comorbidity |
2 Comorbidities |
3+ Comorbidities |
No comorbidities |
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | ||
| Still performing elective surgery | 18 | 18.6 | 0.348 | 33 | 24.5 | 0.500 | 21 | 21.0 | 0.001* | 1 | 1.3 | 0.060 | 0 | 0.0 | 0.543 | 0 | 0.0 | 0.543 | 4 | 4.8 | 0.749 | 10 | 11.2 | 0.087 | 56 | 41.5 | 0.003* | 11 | 12.2 | 0.670 | 3 | 3.7 | 0.468 | 79 | 53.0 | 0.006* | |
| Essential/emergency spine surgery | 74 | 14.2 | 0.055 | 123 | 21.5 | 0.308 | 59 | 11.6 | 0.841 | 25 | 5.3 | 0.387 | 2 | 0.4 | 0.611 | 2 | 0.4 | 0.611 | 18 | 3.9 | 0.336 | 35 | 7.2 | 0.504 | 187 | 29.4 | 0.141 | 52 | 10.4 | 0.448 | 12 | 2.6 | 0.674 | 449 | 64.1 | 0.154 | |
| Impact on clinical time spent | |||||||||||||||||||||||||||||||||||||
| ŌĆā | Increased | 3 | 3.3 | 0.283 | 10 | 6.9 | 0.889 | 5 | 7.6 | 0.865 | 2 | 6.5 | 0.829 | 0 | 0.0 | 0.832 | 0 | 0.0 | 0.832 | 1 | 4.6 | 0.809 | 0 | 0.0 | 0.181 | 12 | 5.4 | 0.587 | 3 | 4.8 | 0.878 | 1 | 7.7 | 0.492 | 30 | 65.2 | 0.703 |
| Decreased | 76 | 82.6 | 122 | 84.1 | 55 | 83.3 | 25 | 80.7 | 2 | 100.0 | 2 | 100.0 | 18 | 81.8 | 36 | 7.8 | 183 | 82.4 | 52 | 83.9 | 12 | 92.3 | 428 | 63.4 | |||||||||||||
| Stayed the same | 13 | 14.1 | 13 | 9.0 | 6 | 9.1 | 4 | 12.9 | 0 | 0.0 | 0 | 0.0 | 3 | 13.6 | 2 | 3.9 | 27 | 12.2 | 7 | 11.3 | 0 | 0.0 | 49 | 59.0 | |||||||||||||
| Perceived impact on resident/fellow training | |||||||||||||||||||||||||||||||||||||
| Not currently training residents/fellows | 31 | 34.1 | 0.813 | 45 | 31.0 | 0.838 | 28 | 42.4 | 0.267 | 11 | 35.5 | 0.839 | 0 | 0.0 | 0.680 | 1 | 50.0 | 0.951 | 7 | 33.3 | 0.588 | 15 | 8.1 | 0.677 | 70 | 31.4 | 0.476 | 22 | 35.5 | 0.089 | 6 | 50.0 | 0.167 | 170 | 63.4 | 0.791 | |
| Hurts training experience | 49 | 53.9 | 84 | 57.9 | 30 | 45.5 | 16 | 51.6 | 2 | 100.0 | 1 | 50.0 | 11 | 52.4 | 18 | 6.0 | 129 | 57.9 | 33 | 53.2 | 4 | 33.3 | 284 | 63.1 | |||||||||||||
| Improves training experience | 4 | 4.4 | 6 | 4.1 | 2 | 3.0 | 2 | 6.5 | 0 | 0.0 | 0 | 0.0 | 2 | 9.5 | 2 | 10.0 | 6 | 2.7 | 6 | 9.7 | 0 | 0.0 | 18 | 60.0 | |||||||||||||
| No overall impact | 7 | 7.7 | 10 | 6.9 | 6 | 9.1 | 2 | 6.5 | 0 | 0.0 | 0 | 0.0 | 1 | 4.8 | 3 | 10.0 | 18 | 8.1 | 1 | 1.6 | 2 | 16.7 | 27 | 56.3 | |||||||||||||
| Warning patients if the surgeon is COVID-19 positive | |||||||||||||||||||||||||||||||||||||
| Absolutely | 66 | 74.2 | 0.298 | 102 | 70.3 | 0.343 | 49 | 74.2 | 0.200 | 28 | 90.3 | 0.209 | 2 | 100.0 | 0.886 | 1 | 50.0 | 0.084 | 17 | 77.3 | 0.717 | 23 | 5.7 | 0.026* | 160 | 72.4 | 0.380 | 41 | 67.2 | 0.369 | 11 | 84.6 | 0.134 | 383 | 64.4 | 0.273 | |
| Likely | 8 | 9.0 | 21 | 14.5 | 6 | 9.1 | 3 | 9.7 | 0 | 0.0 | 0 | 0.0 | 3 | 13.6 | 6 | 8.0 | 27 | 12.2 | 10 | 16.4 | 0 | 0.0 | 69 | 65.1 | |||||||||||||
| Less likely | 6 | 6.7 | 7 | 4.8 | 7 | 10.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 6 | 20.0 | 14 | 6.3 | 3 | 4.9 | 2 | 15.4 | 24 | 55.8 | |||||||||||||
| Not at all | 9 | 10.1 | 15 | 10.3 | 4 | 6.1 | 0 | 0.0 | 0 | 0.0 | 1 | 50.0 | 2 | 9.1 | 3 | 8.8 | 20 | 9.1 | 7 | 11.5 | 0 | 0.0 | 31 | 53.5 | |||||||||||||
| Research activities impacted | |||||||||||||||||||||||||||||||||||||
| No research engagement | 31 | 36.5 | 0.091 | 42 | 29.4 | 0.006* | 20 | 31.3 | 0.731 | 12 | 41.4 | 0.394 | 0 | 0.0 | 0.316 | 1 | 50.0 | 0.443 | 9 | 40.9 | 0.427 | 7 | 5.5 | 0.134 | 59 | 27.8 | 0.211 | 20 | 33.3 | 0.084 | 6 | 46.2 | 0.549 | 121 | 58.7 | 0.031* | |
| Complete stop | 13 | 15.3 | 19 | 13.3 | 12 | 18.8 | 4 | 13.8 | 1 | 50.0 | 0 | 0.0 | 2 | 9.1 | 10 | 11.5 | 35 | 16.5 | 8 | 13.3 | 2 | 15.4 | 77 | 63.1 | |||||||||||||
| Decrease in productivity | 20 | 23.5 | 57 | 39.9 | 19 | 29.7 | 6 | 20.7 | 0 | 0.0 | 0 | 0.0 | 7 | 31.8 | 15 | 9.0 | 69 | 32.6 | 23 | 38.3 | 3 | 23.1 | 152 | 61.5 | |||||||||||||
| No change | 15 | 17.7 | 21 | 14.7 | 7 | 10.9 | 3 | 10.3 | 1 | 50.0 | 0 | 0.0 | 3 | 13.6 | 4 | 5.8 | 34 | 16.0 | 8 | 13.3 | 1 | 7.7 | 65 | 60.2 | |||||||||||||
| Increase in productivity | 6 | 7.1 | 4 | 2.8 | 6 | 9.4 | 4 | 13.8 | 0 | 0.0 | 1 | 50.0 | 1 | 4.6 | 1 | 1.6 | 15 | 7.1 | 1 | 1.7 | 1 | 7.7 | 63 | 78.8 | |||||||||||||
| Surgery Impact | |||||||||||||||||||||||||||||||||||||
| Advise against | 67 | 16.0 | 0.533 | 102 | 22.5 | 0.990 | 43 | 10.9 | 0.383 | 26.0 | 6.9 | 0.108 | 2 | 0.6 | 0.360 | 2 | 0.6 | 0.360 | 14 | 3.8 | 0.498 | 28 | 7.4 | 0.668 | 153 | 30.3 | 0.628 | 46 | 11.6 | 0.416 | 10 | 2.8 | 0.610 | 352 | 62.8 | 0.993 | |
| Proceed with standard precautions | 15 | 20.3 | 0.971 | 25 | 22.3 | 0.668 | 16 | 32.7 | 0.051 | 4 | 14.8 | 0.479 | 0 | 0.0 | 0.474 | 0 | 0.0 | 0.474 | 1 | 6.7 | 0.190 | 4 | 4.7 | 0.347 | 49 | 28.5 | 0.036* | 8 | 16.0 | 0.458 | 0 | 0.0 | 0.110 | 81 | 58.7 | 0.229 | |
| Absent during intubation/extubation | 37 | 43.5 | 0.465 | 46 | 36.2 | 0.020* | 19 | 32.8 | 0.030* | 13 | 44.8 | 0.753 | 0 | 0.0 | 0.177 | 0 | 0.0 | 0.177 | 4 | 23.5 | 0.049* | 13 | 5.6 | 0.348 | 76 | 38.8 | 0.033* | 22 | 39.3 | 0.226 | 3 | 27.3 | 0.177 | 221 | 68.6 | 0.014* | |
| Additional PPE during surgery | 47 | 51.7 | 0.508 | 71 | 49.0 | 0.171 | 33 | 50.0 | 0.407 | 16 | 51.6 | 0.681 | 1 | 50.0 | 0.878 | 0 | 0.0 | 0.116 | 13 | 59.1 | 0.733 | 24 | 8.0 | 0.353 | 113 | 50.7 | 0.239 | 31 | 50.8 | 0.497 | 7 | 53.9 | 0.911 | 277 | 64.7 | 0.212 | |
Calculation of p-values was performed using a combination of chi-square and Fisher exact tests.
Comparisons are made between respondents with comorbidities and healthy individuals. Clinicians with no comorbidities were compared to those with one or more comorbidity. All percentages are calculated based upon the total number of responses received for each question and comorbidity combination.
COVID-19, coronavirus disease 2019; PPE, personal protective equipment.
Table┬Ā4.
| Variable |
Obesity |
Hypertension |
Current tobacco use |
Respiratory illness |
Renal disease |
Cancer |
Cardiac disease |
Diabetes |
1 Comorbidity |
2 Comorbidities |
3+ Comorbidities |
No comorbidities |
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | No. | % | p-value | ||
| Belief that future guidelines are needed | |||||||||||||||||||||||||||||||||||||
| ŌĆā | Yes | 81 | 97.6 | 0.525 | 130 | 94.9 | 0.595 | 57 | 90.5 | 0.336 | 25 | 89.3 | 0.187 | 2 | 100.0 | 0.948 | 2 | 100.0 | 0.948 | 21 | 95.5 | 0.932 | 35 | 7.3 | 0.008* | 195 | 93.8 | 0.309 | 55 | 96.5 | 0.418 | 12 | 92.3 | 0.825 | 448 | 63.1 | 0.313 |
| No | 0 | 0.0 | 2 | 1.5 | 1 | 1.6 | 1 | 3.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 40.0 | 4 | 1.9 | 1 | 1.8 | 0 | 0.0 | 3 | 37.5 | |||||||||||||
| Unsure | 2 | 2.4 | 5 | 3.7 | 5 | 7.9 | 2 | 7.1 | 0 | 0.0 | 0 | 0.0 | 1 | 4.6 | 0 | 0.0 | 9 | 4.3 | 1 | 1.8 | 1 | 7.7 | 21 | 65.6 | |||||||||||||
| Perceived impact in 1 year | |||||||||||||||||||||||||||||||||||||
| No change | 13 | 13.4 | 0.643 | 24 | 22.2 | 0.948 | 11 | 11.6 | 0.953 | 6 | 6.7 | 0.623 | 0 | 0.0 | 0.511 | 0 | 0.0 | 0.511 | 5 | 5.6 | 0.553 | 7 | 7.7 | 0.859 | 40 | 32.3 | 0.647 | 4 | 4.6 | 0.040* | 5 | 5.6 | 0.057 | 84 | 63.2 | 0.963 | |
| Heighted awareness of hygiene | 50 | 79.4 | 0.828 | 73 | 78.5 | 0.941 | 31 | 75.6 | 0.711 | 14 | 70.0 | 0.394 | 2 | 100.0 | 0.455 | 2 | 100.0 | 0.455 | 12 | 70.6 | 0.464 | 23 | 7.4 | 0.883 | 105 | 73.9 | 0.313 | 37 | 90.2 | 0.069 | 7 | 63.6 | 0.255 | 286 | 65.8 | 0.717 | |
| Increase use of PPE | 47 | 61.0 | 0.060 | 67 | 55.8 | 0.214 | 30 | 58.8 | 0.204 | 12 | 48.0 | 0.892 | 2 | 100.0 | 0.153 | 2 | 100.0 | 0.153 | 12 | 60.0 | 0.354 | 18 | 8.0 | 0.455 | 98 | 56.0 | 0.143 | 35 | 66.0 | 0.022* | 5 | 41.7 | 0.597 | 206 | 59.9 | 0.045* | |
| Ask patients to reschedule if sick | 40 | 50.6 | 0.064 | 53 | 41.4 | 0.698 | 28 | 49.1 | 0.164 | 11 | 42.3 | 0.776 | 2 | 100.0 | 0.081 | 1 | 50.0 | 0.762 | 10 | 47.6 | 0.458 | 13 | 7.0 | 0.784 | 81 | 42.6 | 0.462 | 24 | 44.4 | 0.484 | 7 | 53.9 | 0.298 | 173 | 60.7 | 0.291 | |
| Increase nonoperative measures prior to surgery | 19 | 24.1 | 0.163 | 38 | 28.8 | 0.004* | 20 | 33.9 | 0.003* | 5 | 19.2 | 0.816 | 1 | 50.0 | 0.228 | 1 | 50.0 | 0.228 | 6 | 27.3 | 0.241 | 10 | 11.4 | 0.101 | 52 | 26.9 | 0.006* | 17 | 30.4 | 0.020* | 3 | 23.1 | 0.600 | 78 | 52.0 | 0.002* | |
| Increase digital options for communication | 39 | 47.0 | 0.404 | 46 | 33.6 | 0.074 | 24 | 38.1 | 0.547 | 13 | 46.4 | 0.650 | 2 | 100.0 | 0.098 | 1 | 50.0 | 0.821 | 5 | 22.7 | 0.072 | 18 | 8.3 | 0.436 | 91 | 43.8 | 0.683 | 19 | 33.3 | 0.205 | 5 | 38.5 | 0.795 | 199 | 63.4 | 0.850 | |
| How likely to attend a conference in 1 year | |||||||||||||||||||||||||||||||||||||
| Likely | 54 | 65.1 | 0.232 | 90 | 66.2 | 0.626 | 39 | 61.9 | 0.490 | 19 | 67.9 | 0.997 | 2 | 100.0 | 0.627 | 1 | 50.0 | 0.678 | 13 | 59.1 | 0.004* | 21 | 6.1 | 0.325 | 132 | 63.8 | 0.384 | 34 | 59.7 | 0.341 | 9 | 69.2 | 0.478 | 321 | 64.7 | 0.295 | |
| Not likely | 3 | 3.6 | 8 | 5.9 | 7 | 11.1 | 2 | 7.1 | 0 | 0.0 | 0 | 0.0 | 6 | 27.3 | 3 | 7.9 | 14 | 6.8 | 4 | 7.0 | 2 | 15.4 | 35 | 63.6 | |||||||||||||
| Unsure | 26 | 31.3 | 38 | 27.9 | 17 | 27.0 | 7 | 25.0 | 0 | 0.0 | 1 | 50.0 | 3 | 13.6 | 13 | 10.2 | 61 | 29.5 | 19 | 33.3 | 2 | 15.4 | 115 | 58.4 | |||||||||||||
| Timeframe to resume elective surgery | |||||||||||||||||||||||||||||||||||||
| < 2 Weeks | 5 | 5.5 | 0.720 | 5 | 3.5 | 0.279 | 4 | 6.1 | 0.399 | 0 | 0.0 | 0.396 | 0 | 0.0 | 0.850 | 0 | 0.0 | 0.843 | 3 | 13.6 | 0.058 | 1 | 6.3 | 0.902 | 14 | 6.3 | 0.175 | 2 | 3.3 | 0.359 | 0 | 0.0 | 0.923 | 15 | 48.4 | 0.178 | |
| 2ŌĆō4 Weeks | 16 | 17.6 | 29 | 20.1 | 9 | 13.6 | 6 | 19.4 | 0 | 0.0 | 1 | 50.0 | 3 | 13.6 | 8 | 8.8 | 41 | 18.5 | 9 | 14.8 | 3 | 23.1 | 83 | 61.0 | |||||||||||||
| 1ŌĆō2 Months | 15 | 16.5 | 24 | 16.7 | 8 | 12.1 | 4 | 12.9 | 0 | 0.0 | 0 | 0.0 | 1 | 4.6 | 5 | 5.5 | 29 | 13.1 | 10 | 16.4 | 2 | 15.4 | 86 | 67.7 | |||||||||||||
| > 2 Months | 3 | 3.3 | 4 | 2.8 | 2 | 3.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 8.0 | 9 | 4.1 | 1 | 1.6 | 0 | 0.0 | 23 | 69.7 | |||||||||||||
| No current stoppage | 11 | 12.1 | 21 | 14.6 | 10 | 15.2 | 1 | 3.2 | 0 | 0.0 | 0 | 0.0 | 3 | 13.6 | 5 | 9.6 | 26 | 11.7 | 11 | 18.0 | 1 | 7.7 | 47 | 55.3 | |||||||||||||
| Unknown | 41 | 45.1 | 61 | 42.4 | 33 | 50.0 | 20 | 64.5 | 2 | 100.0 | 1 | 50.0 | 12 | 54.6 | 17 | 6.3 | 103 | 46.4 | 28 | 45.9 | 7 | 53.9 | 254 | 64.8 | |||||||||||||
| Anticipated # weeks to resume baseline activity | |||||||||||||||||||||||||||||||||||||
| < 2 Weeks | 10 | 11.8 | 0.450 | 13 | 9.3 | 0.041* | 10 | 15.6 | 0.805 | 1 | 3.5 | 0.403 | 0 | 0.0 | 0.307 | 0 | 0.0 | 0.160 | 3 | 13.6 | 0.216 | 3 | 4.4 | 0.082 | 24 | 11.5 | 0.126 | 6 | 10.0 | 0.267 | 1 | 7.7 | 0.876 | 65 | 67.7 | 0.039* | |
| 2ŌĆō4 Weeks | 24 | 28.2 | 43 | 30.7 | 15 | 23.4 | 9 | 31.0 | 0 | 0.0 | 0 | 0.0 | 8 | 36.4 | 12 | 11.1 | 58 | 27.8 | 19 | 31.7 | 4 | 30.8 | 96 | 54.2 | |||||||||||||
| 4ŌĆō6 Weeks | 19 | 22.4 | 34 | 24.3 | 15 | 23.4 | 6 | 20.7 | 0 | 0.0 | 2 | 100.0 | 5 | 22.7 | 13 | 10.6 | 49 | 23.4 | 15 | 25.0 | 3 | 23.1 | 110 | 62.2 | |||||||||||||
| 6ŌĆō8 Weeks | 13 | 15.3 | 21 | 15.0 | 10 | 15.6 | 5 | 17.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 4.3 | 32 | 15.3 | 7 | 11.7 | 2 | 15.4 | 67 | 62.0 | |||||||||||||
| > 8 Weeks | 19 | 22.4 | 29 | 20.7 | 14 | 21.9 | 8 | 27.6 | 2 | 100.0 | 0 | 0.0 | 6 | 27.3 | 6 | 4.1 | 46 | 22.0 | 13 | 21.7 | 3 | 23.1 | 139 | 69.2 | |||||||||||||
| % Telecommunication clinical visits/wk | |||||||||||||||||||||||||||||||||||||
| 0ŌĆō25 | 51 | 55.4 | 0.355 | 77 | 53.1 | 0.147 | 42 | 63.6 | 0.025* | 18 | 58.1 | 0.326 | 1 | 50.0 | 0.845 | 0 | 0.0 | 0.168 | 9 | 40.9 | 0.599 | 20 | 7.7 | 0.009* | 112 | 50.2 | 0.323 | 36 | 59.0 | 0.047* | 9 | 69.2 | 0.389 | 241 | 60.6 | 0.068 | |
| 26ŌĆō50 | 11 | 12.0 | 26 | 17.9 | 11 | 16.7 | 2 | 6.5 | 0 | 0.0 | 0 | 0.0 | 4 | 18.2 | 11 | 14.1 | 38 | 17.0 | 12 | 19.7 | 1 | 7.7 | 67 | 56.8 | |||||||||||||
| 51ŌĆō75 | 5 | 5.4 | 12 | 8.3 | 4 | 6.1 | 1 | 3.2 | 0 | 0.0 | 0 | 0.0 | 4 | 18.2 | 2 | 3.6 | 18 | 8.1 | 5 | 8.2 | 0 | 0.0 | 54 | 70.1 | |||||||||||||
| 76ŌĆō100 | 25 | 27.2 | 30 | 20.7 | 9 | 13.6 | 10 | 32.3 | 1 | 50.0 | 2 | 100.0 | 5 | 22.7 | 4 | 2.7 | 55 | 24.7 | 8 | 13.1 | 3 | 23.1 | 142 | 68.3 | |||||||||||||
Calculation of p-values was performed using a combination of chi-square and Fisher exact tests.
Comparisons are made between respondents with comorbidities and healthy individuals. Clinicians with no comorbidities were compared to those with one or more comorbidity. All percentages are calculated based upon the total number of responses received for each question and comorbidity combination.
PPE, personal protective equipment.
Table┬Ā5.
| Assessed survey responses |
Age |
Female sex |
Orthopaedics |
Neurosurgery |
Trauma |
Academic Practice |
Private practice |
Public/local practice |
Obese |
Hypertension |
Current tobacco use |
Respiratory illness |
Cardiac disease |
Diabetes |
|||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Reasons for COVID-19 testing | |||||||||||||||||||||||||||||||||||||||||||
| ŌĆā | Personally tested for COVID-19 | 0.99 | 0.74ŌĆō1.33 | 0.962 | 2.56 | 1.04ŌĆō6.29 | 0.041* | 2.71 | 0.55ŌĆō13.27 | 0.219 | 3.47 | 0.72ŌĆō16.71 | 0.121 | 1.98 | 0.91ŌĆō4.28 | 0.083 | 1.35 | 0.69ŌĆō2.65 | 0.386 | 0.42 | 0.13ŌĆō1.34 | 0.143 | 0.55 | 0.19ŌĆō1.55 | 0.259 | 1.06 | 0.43ŌĆō2.59 | 0.902 | 0.79 | 0.33ŌĆō1.89 | 0.603 | 0.18 | 0.02ŌĆō1.33 | 0.093 | 1.05 | 0.23ŌĆō4.76 | 0.949 | 1.93 | 0.41ŌĆō9.09 | 0.404 | 0.85 | 0.19ŌĆō3.79 | 0.834 |
| Direct contact with COVID-19 positive patient | 1.03 | 0.70ŌĆō1.51 | 0.873 | 0.82 | 0.20ŌĆō3.34 | 0.782 | 0.21 | 0.02ŌĆō2.43 | 0.210 | 0.30 | 0.03ŌĆō3.51 | 0.340 | 1.76 | 0.51ŌĆō6.14 | 0.374 | 1.11 | 0.41ŌĆō3.03 | 0.835 | 1.64 | 0.41ŌĆō6.59 | 0.488 | 1.89 | 0.53ŌĆō6.74 | 0.324 | 0.50 | 0.13ŌĆō1.98 | 0.325 | 0.59 | 0.18ŌĆō1.88 | 0.370 | 0.14 | 0.02ŌĆō1.20 | 0.073 | 0.75 | 0.06ŌĆō10.04 | 0.825 | 2.04 | 0.33ŌĆō12.61 | 0.441 | 1.03 | 0.17ŌĆō6.23 | 0.971 | |
| Prophylactic | 3.05 | 1.22ŌĆō7.63 | 0.017* | 1.00 | 1.00ŌĆō1.00 | - | 108.44 | 0.85ŌĆō13,777.31 | 0.058 | 126.17 | 0.92ŌĆō17289.75 | 0.054 | 18.97 | 2.39ŌĆō150.68 | 0.005* | 0.92 | 0.17ŌĆō4.99 | 0.919 | 0.07 | 0.00ŌĆō6.09 | 0.247 | 0.07 | 0.00ŌĆō1.51 | 0.090 | 3.79 | 0.49ŌĆō29.12 | 0.200 | 0.18 | 0.01ŌĆō2.27 | 0.183 | 9.90 | 1.10ŌĆō89.14 | 0.041* | 1.00 | 1.00ŌĆō1.00 | - | 0.54 | .01ŌĆō42.62 | 0.780 | 1.26 | 0.09ŌĆō18.54 | 0.866 | |
| Demonstrated symptoms | 0.82 | 0.56ŌĆō1.18 | 0.280 | 1.46 | 0.40ŌĆō5.28 | 0.564 | 2.00 | 0.23ŌĆō17.69 | 0.532 | 1.38 | 0.16ŌĆō12.01 | 0.770 | 0.32 | 0.08ŌĆō1.17 | 0.085 | 0.82 | 0.32ŌĆō2.08 | 0.670 | 0.93 | 0.24ŌĆō3.59 | 0.918 | 0.72 | 0.21ŌĆō2.45 | 0.604 | 1.21 | 0.33ŌĆō4.37 | 0.772 | 1.42 | 0.48ŌĆō4.22 | 0.526 | 1.73 | 0.44ŌĆō6.86 | 0.433 | 3.46 | 0.25ŌĆō46.99 | 0.352 | 0.47 | 0.07ŌĆō3.03 | 0.428 | 0.35 | 0.06ŌĆō2.14 | 0.258 | |
| Ask to be tested | 0.70 | 0.29ŌĆō1.69 | 0.430 | 3.53 | 0.28ŌĆō44.17 | 0.328 | - | - | - | - | - | - | 1.00 | 1.00ŌĆō1.00 | - | 1.49 | 0.14ŌĆō15.86 | 0.741 | 1.00 | 1.00ŌĆō1.00 | - | 6.48 | 0.41ŌĆō102.85 | 0.185 | 2.36 | 0.17ŌĆō32.46 | 0.522 | 7.55 | 0.99ŌĆō57.45 | 0.051 | 1.75 | 0.13ŌĆō22.97 | 0.672 | 1.00 | 1.00ŌĆō1.00 | - | 1.00 | 1.00ŌĆō1.00 | - | 3.58 | 0.38ŌĆō34.15 | 0.267 | |
| Current stressors | |||||||||||||||||||||||||||||||||||||||||||
| Personal health | 1.10 | 0.95ŌĆō1.28 | 0.199 | 0.72 | 0.39ŌĆō1.35 | 0.307 | 0.59 | 0.26ŌĆō1.32 | 0.196 | 0.69 | 0.30ŌĆō1.57 | 0.379 | 1.11 | 0.70ŌĆō1.77 | 0.657 | 0.97 | 0.68ŌĆō1.38 | 0.855 | 0.73 | 0.47ŌĆō1.16 | 0.185 | 1.26 | 0.79ŌĆō2.03 | 0.335 | 1.33 | 0.86ŌĆō2.07 | 0.199 | 1.50 | 1.01ŌĆō2.23 | 0.046* | 0.81 | 0.48ŌĆō1.37 | 0.428 | 1.55 | 0.72ŌĆō3.34 | 0.264 | 2.49 | 0.98ŌĆō6.30 | 0.055 | 0.81 | 0.41ŌĆō1.59 | 0.531 | |
| Family health | 1.16 | 0.94ŌĆō1.43 | 0.168 | 0.29 | 0.15ŌĆō0.56 | < 0.001* | 1.23 | 0.43ŌĆō3.50 | 0.699 | 1.45 | 0.50ŌĆō4.25 | 0.494 | 1.24 | 0.65ŌĆō2.35 | 0.513 | 1.12 | 0.69ŌĆō1.81 | 0.644 | 1.23 | 0.65ŌĆō2.33 | 0.521 | 1.00 | 0.53ŌĆō1.86 | 0.988 | 1.24 | 0.65ŌĆō2.38 | 0.515 | 0.95 | 0.55ŌĆō1.67 | 0.869 | 0.52 | 0.28ŌĆō0.97 | 0.039* | 1.69 | 0.48ŌĆō5.96 | 0.412 | 1.15 | 0.32ŌĆō4.12 | 0.834 | 0.79 | 0.33ŌĆō1.93 | 0.609 | |
| Community health | 0.96 | 0.83ŌĆō1.12 | 0.627 | 1.14 | 0.63ŌĆō2.06 | 0.675 | 2.31 | 1.00ŌĆō5.34 | 0.050 | 2.12 | 0.91ŌĆō4.97 | 0.082 | 1.77 | 1.11ŌĆō2.81 | 0.017* | 0.71 | 0.50ŌĆō1.01 | 0.058 | 0.91 | 0.58ŌĆō1.42 | 0.665 | 0.67 | 0.42ŌĆō1.08 | 0.102 | 0.65 | 0.42ŌĆō1.03 | 0.066 | 0.89 | 0.60ŌĆō1.33 | 0.578 | 1.41 | 0.84ŌĆō2.37 | 0.189 | 0.48 | 0.20ŌĆō1.11 | 0.087 | 1.94 | 0.81ŌĆō4.67 | 0.139 | 1.89 | 0.97ŌĆō3.71 | 0.063 | |
| Hospital capacity | 0.97 | 0.83ŌĆō1.12 | 0.662 | 1.15 | 0.63ŌĆō2.11 | 0.644 | 1.08 | 0.48ŌĆō2.44 | 0.852 | 1.18 | 0.52ŌĆō2.69 | 0.700 | 1.63 | 1.02ŌĆō2.59 | 0.041* | 1.42 | 1.00ŌĆō2.03 | 0.053 | 0.61 | 0.38ŌĆō0.99 | 0.044* | 2.28 | 1.42ŌĆō3.68 | 0.001* | 1.28 | 0.82ŌĆō2.00 | 0.284 | 1.39 | 0.92ŌĆō2.08 | 0.114 | 0.75 | 0.44ŌĆō1.29 | 0.298 | 0.97 | 0.43ŌĆō2.15 | 0.932 | 0.71 | 0.28ŌĆō1.79 | 0.470 | 0.51 | 0.24ŌĆō1.06 | 0.071 | |
| Timeline to resume clinical practice | 0.94 | 0.81ŌĆō1.08 | 0.371 | 1.45 | 0.80ŌĆō2.62 | 0.217 | 1.06 | 0.48ŌĆō2.32 | 0.887 | 0.96 | 0.43ŌĆō2.14 | 0.928 | 0.95 | 0.60ŌĆō1.51 | 0.837 | 0.94 | 0.66ŌĆō1.33 | 0.716 | 1.12 | 0.72ŌĆō1.74 | 0.622 | 0.70 | 0.43ŌĆō1.12 | 0.133 | 0.89 | 0.57ŌĆō1.38 | 0.591 | 0.77 | 0.52ŌĆō1.15 | 0.209 | 0.95 | 0.56ŌĆō1.59 | 0.838 | 0.56 | 0.25ŌĆō1.26 | 0.158 | 1.20 | 0.50ŌĆō2.85 | 0.685 | 0.77 | 0.38ŌĆō1.52 | 0.447 | |
| Government/leadership | 0.94 | 0.78ŌĆō1.13 | 0.507 | 2.05 | 1.08ŌĆō3.91 | 0.028* | 2.19 | 0.76ŌĆō6.29 | 0.145 | 1.79 | 0.62ŌĆō5.15 | 0.278 | 0.98 | 0.55ŌĆō1.74 | 0.945 | 1.57 | 0.97ŌĆō2.54 | 0.068 | 1.48 | 0.82ŌĆō2.68 | 0.198 | 1.47 | 0.79ŌĆō2.72 | 0.226 | 1.14 | 0.66ŌĆō1.97 | 0.647 | 0.85 | 0.50ŌĆō1.46 | 0.565 | 0.85 | 0.50ŌĆō1.46 | 0.565 | 1.16 | 0.45ŌĆō2.96 | 0.758 | 1.81 | 0.67ŌĆō4.88 | 0.241 | 0.84 | 0.34ŌĆō2.12 | 0.716 | |
| Return to nonessential activities | 1.01 | 0.82ŌĆō1.25 | 0.923 | 1.33 | 0.61ŌĆō2.89 | 0.470 | 1.35 | 0.46ŌĆō3.99 | 0.586 | 1.13 | 0.38ŌĆō3.39 | 0.829 | 1.77 | 0.99ŌĆō3.17 | 0.052 | 1.66 | 0.96ŌĆō2.86 | 0.067 | 1.70 | 0.88ŌĆō3.29 | 0.117 | 1.29 | 0.63ŌĆō2.64 | 0.493 | 0.75 | 0.38ŌĆō1.48 | 0.407 | 1.32 | 0.76ŌĆō2.30 | 0.324 | 1.32 | 0.76ŌĆō2.30 | 0.324 | 1.04 | 0.35ŌĆō3.09 | 0.945 | 0.89 | 0.25ŌĆō3.18 | 0.858 | 0.66 | 0.22ŌĆō1.94 | 0.448 | |
| Economic issues | 0.85 | 0.73ŌĆō0.99 | 0.032* | 0.70 | 0.38ŌĆō1.30 | 0.262 | 1.78 | 0.77 ,4.07 | 0.175 | 1.70 | 0.73ŌĆō3.93 | 0.216 | 0.95 | 0.59ŌĆō1.51 | 0.823 | 0.55 | 0.38ŌĆō0.78 | 0.001* | 1.26 | 0.80ŌĆō1.98 | 0.314 | 0.51 | 0.31ŌĆō0.82 | 0.006* | 0.81 | 0.52ŌĆō1.27 | 0.359 | 0.87 | 0.58ŌĆō1.312 | 0.514 | 0.87 | 0.58ŌĆō1.31 | 0.514 | 2.97 | 1.27ŌĆō6.96 | 0.012* | 1.86 | 0.77ŌĆō4.50 | 0.170 | 0.61 | 0.30ŌĆō1.26 | 0.184 | |
| Clinical practice | |||||||||||||||||||||||||||||||||||||||||||
| Quarantine | 1.03 | 0.86ŌĆō1.23 | 0.735 | 2.07 | 1.08ŌĆō3.95 | 0.028* | 1.35 | 0.52ŌĆō3.52 | 0.542 | 2.28 | 0.87ŌĆō5.98 | 0.094 | 0.80 | 0.44ŌĆō1.47 | 0.472 | 0.66 | 0.44ŌĆō1.00 | 0.049* | 0.91 | 0.55ŌĆō1.52 | 0.731 | 0.54 | 0.30ŌĆō0.97 | 0.038* | 0.83 | 0.48ŌĆō1.41 | 0.483 | 1.29 | 0.82ŌĆō2.04 | 0.277 | 1.29 | 0.82ŌĆō2.04 | 0.277 | 1.88 | 0.84ŌĆō4.24 | 0.127 | 0.42 | 0.11ŌĆō1.56 | 0.196 | 1.56 | 0.74ŌĆō3.27 | 0.240 | |
| Still performing elective surgery | 1.13 | 0.93ŌĆō1.37 | 0.218 | 0.44 | 0.15ŌĆō1.27 | 0.128 | 1.23 | 0.40 ,3.83 | 0.718 | 0.78 | 0.25ŌĆō2.45 | 0.665 | 0.32 | 0.14ŌĆō0.72 | 0.006* | 2.18 | 1.33ŌĆō3.55 | 0.002* | 0.82 | 0.40ŌĆō1.66 | 0.575 | 1.56 | 0.80ŌĆō3.04 | 0.191 | 1.17 | 0.65ŌĆō2.09 | 0.604 | 1.24 | 0.76ŌĆō2.02 | 0.396 | 1.24 | 0.76ŌĆō2.02 | 0.396 | 0.16 | 0.02ŌĆō1.22 | 0.077 | 0.92 | 0.29ŌĆō2.91 | 0.887 | 1.26 | 0.57ŌĆō2.77 | 0.569 | |
| Essential/emergency spine surgery | 0.91 | 0.73ŌĆō1.14 | 0.407 | 0.52 | 0.24ŌĆō1.14 | 0.103 | 1.44 | 0.45ŌĆō4.63 | 0.536 | 2.22 | 0.66ŌĆō7.44 | 0.196 | 0.77 | 0.40ŌĆō1.49 | 0.446 | 2.35 | 1.33ŌĆō4.15 | 0.003* | 0.79 | 0.43ŌĆō1.45 | 0.446 | 0.82 | 0.43ŌĆō1.57 | 0.556 | 0.61 | 0.33ŌĆō1.12 | 0.113 | 0.88 | 0.48ŌĆō1.59 | 0.663 | 0.88 | 0.48ŌĆō1.59 | 0.663 | 0.69 | 0.25ŌĆō1.93 | 0.477 | 0.97 | 0.30ŌĆō3.18 | 0.962 | 1.90 | 0.55ŌĆō6.58 | 0.310 | |
| Advise against | 1.01 | 0.85ŌĆō1.19 | 0.940 | 0.79 | 0.42ŌĆō1.51 | 0.475 | 0.74 | 0.29ŌĆō1.87 | 0.524 | 0.52 | 0.21ŌĆō1.33 | 0.174 | 1.57 | 0.90ŌĆō2.74 | 0.113 | 0.82 | 0.55ŌĆō1.21 | 0.323 | 1.73 | 0.99ŌĆō3.03 | 0.054 | 0.64 | 0.39ŌĆō1.08 | 0.094 | 1.15 | 0.69ŌĆō1.92 | 0.598 | 0.89 | 0.58ŌĆō1.38 | 0.605 | 0.89 | 0.58ŌĆō1.38 | 0.605 | 1.90 | 0.70ŌĆō5.12 | 0.205 | 0.60 | 0.24ŌĆō1.53 | 0.288 | 1.20 | 0.56ŌĆō2.58 | 0.642 | |
| Proceed with standard precautions | 1.11 | 0.91ŌĆō1.35 | 0.265 | 0.26 | 0.08ŌĆō0.87 | 0.067 | 1.15 | 0.41 ,3.26 | 0.583 | 1.46 | 0.51ŌĆō4.18 | 0.287 | 1.66 | 0.94ŌĆō2.93 | 0.244 | 0.95 | 0.60ŌĆō1.51 | 0.936 | 0.65 | 0.34ŌĆō1.27 | 0.114 | 1.40 | 0.77ŌĆō2.53 | 0.234 | 0.92 | 0.50ŌĆō1.69 | 0.795 | 1.07 | 0.64ŌĆō1.81 | 0.604 | 1.07 | 0.64ŌĆō1.81 | 0.604 | 0.85 | 0.29ŌĆō2.55 | 0.543 | 0.19 | 0.03ŌĆō1.49 | 0.133 | 0.53 | 0.18ŌĆō1.56 | 0.176 | |
| Absent during intubation/extubation | 0.84 | 0.72ŌĆō0.98 | 0.076 | 0.73 | 0.39ŌĆō1.36 | 0.805 | 0.80 | 0.33ŌĆō1.89 | 0.966 | 0.84 | 0.35ŌĆō2.04 | 0.974 | 1.03 | 0.64ŌĆō1.66 | 0.618 | 1.27 | 0.88ŌĆō1.84 | 0.135 | 1.04 | 0.65ŌĆō1.68 | 0.825 | 1.22 | 0.74ŌĆō2.00 | 0.191 | 1.11 | 0.70ŌĆō1.77 | 0.751 | 0.76 | 0.50ŌĆō1.16 | 0.307 | 0.76 | 0.50ŌĆō1.16 | 0.307 | 1.00 | 0.45ŌĆō2.22 | 0.980 | 0.42 | 0.14ŌĆō1.29 | 0.268 | 0.96 | 0.47ŌĆō1.97 | 0.974 | |
| Additional PPE during surgery | 0.91 | 0.78ŌĆō1.06 | 0.214 | 1.51 | 0.81ŌĆō2.84 | 0.198 | 1.55 | 0.67ŌĆō3.63 | 0.307 | 2.00 | 0.84ŌĆō4.72 | 0.115 | 0.86 | 0.54ŌĆō1.37 | 0.525 | 1.20 | 0.84ŌĆō1.71 | 0.319 | 0.72 | 0.45ŌĆō1.13 | 0.155 | 1.27 | 0.78ŌĆō2.06 | 0.336 | 0.94 | 0.60ŌĆō1.48 | 0.786 | 0.85 | 0.57ŌĆō1.27 | 0.420 | 0.85 | 0.57ŌĆō1.27 | 0.420 | 0.87 | 0.40ŌĆō1.87 | 0.720 | 1.66 | 0.67ŌĆō4.13 | 0.273 | 1.76 | 0.87ŌĆō3.55 | 0.114 | |
| % Telecommunication clinical visits/wk | 0.94 | 0.81ŌĆō1.08 | 0.380 | 1.69 | 0.95ŌĆō3.01 | 0.077 | 0.68 | 0.32ŌĆō1.46 | 0.328 | 0.85 | 0.40ŌĆō1.84 | 0.689 | 0.99 | 0.64ŌĆō1.54 | 0.972 | 1.78 | 1.27ŌĆō2.49 | 0.001* | 1.08 | 0.70ŌĆō1.67 | 0.732 | 0.71 | 0.44ŌĆō1.14 | 0.153 | 0.97 | 0.63ŌĆō1.49 | 0.874 | 0.88 | 0.61ŌĆō1.27 | 0.489 | 0.88 | 0.61ŌĆō1.27 | 0.489 | 0.89 | 0.42ŌĆō1.91 | 0.768 | 1.67 | 0.76ŌĆō3.66 | 0.200 | 0.67 | 0.36ŌĆō1.26 | 0.218 | |
| Perceived impact in 1 year | |||||||||||||||||||||||||||||||||||||||||||
| No change | 1.08 | 0.88ŌĆō1.33 | 0.449 | 0.69 | 0.29ŌĆō1.64 | 0.403 | 0.98 | 0.33ŌĆō2.89 | 0.974 | 1.15 | 0.38ŌĆō3.42 | 0.806 | 0.98 | 0.51ŌĆō1.86 | 0.943 | 1.53 | 0.90ŌĆō2.60 | 0.117 | 1.41 | 0.73ŌĆō2.73 | 0.309 | 2.67 | 1.42ŌĆō5.03 | 0.002* | 0.84 | 0.44ŌĆō1.60 | 0.591 | 0.93 | 0.54ŌĆō1.61 | 0.808 | 0.93 | 0.54ŌĆō1.61 | 0.808 | 1.57 | 0.60ŌĆō4.07 | 0.358 | 1.24 | 0.43ŌĆō3.58 | 0.695 | 1.13 | 0.47ŌĆō2.71 | 0.789 | |
| Heighted awareness of hygiene | 0.89 | 0.76ŌĆō1.04 | 0.292 | 1.23 | 0.65ŌĆō2.33 | 0.427 | 1.58 | 0.68ŌĆō3.69 | 0.790 | 1.59 | 0.67ŌĆō3.76 | 0.984 | 1.05 | 0.64ŌĆō1.72 | 0.964 | 0.77 | 0.52ŌĆō1.12 | 0.149 | 0.65 | 0.40ŌĆō1.06 | 0.207 | 0.43 | 0.26ŌĆō0.72 | 0.001* | 1.20 | 0.74ŌĆō1.96 | 0.604 | 0.81 | 0.53ŌĆō1.23 | 0.676 | 0.81 | 0.53ŌĆō1.23 | 0.676 | 0.76 | 0.34ŌĆō1.71 | 0.273 | 1.14 | 0.47ŌĆō2.78 | 0.713 | 1.30 | 0.64ŌĆō2.64 | 0.946 | |
| Increase use of PPE | 0.92 | 0.79ŌĆō1.08 | 0.318 | 0.98 | 0.53ŌĆō1.83 | 0.950 | 0.84 | 0.36ŌĆō1.93 | 0.678 | 1.23 | 0.53ŌĆō2.87 | 0.625 | 1.06 | 0.65ŌĆō1.72 | 0.828 | 0.68 | 0.47ŌĆō0.99 | 0.042* | 0.49 | 0.30ŌĆō0.79 | 0.004* | 0.61 | 0.37ŌĆō1.00 | 0.051 | 1.51 | 0.94ŌĆō2.44 | 0.089 | 1.14 | 0.75ŌĆō1.74 | 0.527 | 1.14 | 0.75ŌĆō1.74 | 0.835 | 0.86 | 0.38ŌĆō1.97 | 0.727 | 1.58 | 0.65ŌĆō3.85 | 0.315 | 1.05 | 0.52ŌĆō2.10 | 0.893 | |
| Ask patients to reschedule if sick | 1.17 | 0.99ŌĆō1.37 | 0.026* | 1.00 | 0.53ŌĆō1.89 | 0.938 | 0.85 | 0.37ŌĆō1.97 | 0.883 | 0.97 | 0.42ŌĆō2.28 | 0.938 | 1.28 | 0.78ŌĆō2.09 | 0.240 | 0.99 | 0.68ŌĆō1.45 | 0.932 | 0.99 | 0.61ŌĆō1.61 | 0.912 | 1.07 | 0.65ŌĆō1.77 | 0.816 | 1.53 | 0.95ŌĆō2.46 | 0.111 | 0.87 | 0.57ŌĆō1.34 | 0.442 | 0.87 | 0.57ŌĆō1.34 | 0.442 | 1.01 | 0.44ŌĆō2.30 | 0.931 | 1.14 | 0.47ŌĆō2.77 | 0.909 | 0.81 | 0.40ŌĆō1.67 | 0.491 | |
| Increase nonoperative measures prior to surgery | 0.98 | 0.80ŌĆō1.20 | 0.994 | 1.45 | 0.70ŌĆō3.02 | 0.291 | 0.74 | 0.28ŌĆō1.94 | 0.709 | 1.01 | 0.38ŌĆō2.70 | 0.822 | 1.27 | 0.71ŌĆō2.30 | 0.381 | 0.83 | 0.53ŌĆō1.31 | 0.490 | 0.55 | 0.29ŌĆō1.04 | 0.071 | 0.88 | 0.48ŌĆō1.60 | 0.622 | 1.00 | 0.56ŌĆō1.80 | 0.976 | 1.59 | 0.97ŌĆō2.61 | 0.085 | 1.59 | 0.97ŌĆō2.61 | 0.085 | 0.71 | 0.23ŌĆō2.18 | 0.516 | 1.48 | 0.54ŌĆō4.08 | 0.529 | 1.35 | 0.61ŌĆō2.97 | 0.467 | |
| Increase digital options for communication | 1.14 | 0.97ŌĆō1.34 | 0.112 | 1.34 | 0.72ŌĆō2.49 | 0.352 | 1.07 | 0.46ŌĆō2.52 | 0.871 | 1.36 | 0.57ŌĆō3.22 | 0.491 | 1.14 | 0.70ŌĆō1.87 | 0.591 | 1.08 | 0.74ŌĆō1.57 | 0.685 | 0.67 | 0.41 ,1.09 | 0.107 | 0.80 | 0.49ŌĆō1.33 | 0.393 | 1.39 | 0.86ŌĆō2.25 | 0.180 | 0.58 | 0.38ŌĆō0.90 | 0.015* | 0.58 | 0.38ŌĆō0.90 | 0.015* | 0.97 | 0.42ŌĆō2.25 | 0.949 | 0.42 | 0.15ŌĆō1.20 | 0.105 | 1.57 | 0.78ŌĆō3.16 | 0.210 | |
| Other perceptions | |||||||||||||||||||||||||||||||||||||||||||
| Media perceptions | 1.02 | 0.89ŌĆō1.17 | 0.810 | 0.59 | 0.33ŌĆō1.05 | 0.071 | 0.57 | 0.28ŌĆō1.19 | 0.133 | 0.75 | 0.36ŌĆō1.58 | 0.455 | 1.30 | 0.84ŌĆō2.01 | 0.244 | 1.17 | 0.84ŌĆō1.63 | 0.353 | 1.23 | 0.81ŌĆō1.87 | 0.340 | 1.17 | 0.75ŌĆō1.83 | 0.492 | 1.28 | 0.84ŌĆō1.96 | 0.248 | 1.20 | 0.83ŌĆō1.73 | 0.345 | 1.20 | 0.83ŌĆō1.73 | 0.345 | 1.44 | 0.69ŌĆō2.98 | 0.329 | 1.10 | 0.48ŌĆō2.54 | 0.815 | 0.66 | 0.35ŌĆō1.25 | 0.204 | |
| Perception of hospital effectiveness | 1.51 | 1.29ŌĆō1.77 | < 0.001* | 0.61 | 0.34ŌĆō1.10 | 0.103 | 1.47 | 0.62ŌĆō3.46 | 0.381 | 1.17 | 0.49ŌĆō2.80 | 0.724 | 1.28 | 0.78ŌĆō2.09 | 0.335 | 1.98 | 1.38ŌĆō2.85 | < 0.001* | 2.01 | 1.25ŌĆō3.23 | 0.004* | 1.00 | 0.62ŌĆō1.60 | 0.994 | 0.72 | 0.46ŌĆō1.14 | 0.162 | 0.72 | 0.48ŌĆō1.08 | 0.108 | 0.72 | 0.48ŌĆō1.08 | 0.108 | 1.23 | 0.57ŌĆō2.67 | 0.601 | 0.46 | 0.19ŌĆō1.10 | 0.083 | 1.05 | 0.53ŌĆō2.09 | 0.883 | |
| Perception of government effectiveness | 1.19 | 1.02ŌĆō1.38 | 0.024* | 0.61 | 0.34ŌĆō1.08 | 0.088 | 0.87 | 0.41 ,1.88 | 0.728 | 0.80 | 0.37ŌĆō1.74 | 0.570 | 1.17 | 0.73ŌĆō1.87 | 0.511 | 1.13 | 0.79ŌĆō1.61 | 0.496 | 1.12 | 0.71ŌĆō1.78 | 0.626 | 0.85 | 0.53ŌĆō1.36 | 0.498 | 0.99 | 0.63ŌĆō1.55 | 0.961 | 0.67 | 0.45ŌĆō0.99 | 0.047* | 0.67 | 0.45ŌĆō0.99 | 0.047* | 1.59 | 0.71ŌĆō3.57 | 0.259 | 0.76 | 0.31ŌĆō1.85 | 0.550 | 1.08 | 0.56ŌĆō2.07 | 0.828 | |
| Warning patients if the surgeon is COVID-19 positive | 1.46 | 1.22ŌĆō1.74 | < 0.001* | 0.82 | 0.43ŌĆō1.59 | 0.564 | 1.34 | 0.52ŌĆō3.44 | 0.548 | 1.76 | 0.67ŌĆō4.65 | 0.255 | 1.10 | 0.65ŌĆō1.87 | 0.709 | 0.57 | 0.37ŌĆō0.88 | 0.010* | 0.87 | 0.49ŌĆō1.54 | 0.633 | 0.55 | 0.32ŌĆō0.96 | 0.037* | 0.88 | 0.52ŌĆō1.49 | 0.629 | 0.58 | 0.37ŌĆō0.91 | 0.017* | 0.58 | 0.37ŌĆō0.91 | 0.017* | 5.23 | 1.20ŌĆō22.83 | 0.028* | 0.96 | 0.33ŌĆō2.79 | 0.940 | 0.50 | 0.25ŌĆō0.99 | 0.048* | |
COVID-19, coronavirus disease 2019; OR, odds ratio; CI, confidence interval; PPE, personal protective equipment.
All multivariate models were assessed using the same set of independent factors and included baseline demographics, practice-specific variables, and medical comorbidities. Renal disease and cancer were excluded from assessment due to low study prevalence.
Multivariate logistic regression was used to assess survey responses with simple binary outcomes where ordinal logistic regression was implemented for questions with ordinal scales.
Table┬Ā6.
| Assessed survey responses |
Age |
Female sex |
Orthopaedics |
Neurosurgery |
Trauma |
Academic Practice |
Private practice |
Public/local practice |
Number of comorbidities |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | ||
| Reasons for COVID-19 testing | ||||||||||||||||||||||||||||
| ŌĆā | Personally tested for COVID-19 | 1.02 | 0.76ŌĆō1.35 | 0.917 | 2.47 | 1.01ŌĆō6.00 | 0.047* | 2.51 | 0.56ŌĆō11.29 | 0.230 | 3.06 | 0.69ŌĆō13.50 | 0.140 | 1.95 | 0.91ŌĆō4.18 | 0.087 | 1.32 | 0.68ŌĆō2.59 | 0.413 | 0.45 | 0.14ŌĆō1.40 | 0.168 | 0.58 | 0.21ŌĆō1.62 | 0.298 | 0.80 | 0.51ŌĆō1.28 | 0.357 |
| Direct contact with COVID-19 positive patient | 1.05 | 0.72ŌĆō1.51 | 0.804 | 0.78 | 0.20ŌĆō3.02 | 0.723 | 0.31 | 0.03ŌĆō3.37 | 0.339 | 0.39 | 0.04ŌĆō4.13 | 0.432 | 1.64 | 0.50ŌĆō5.31 | 0.412 | 1.11 | 0.42ŌĆō2.94 | 0.830 | 1.86 | 0.48ŌĆō7.22 | 0.368 | 1.85 | 0.54ŌĆō6.29 | 0.328 | 0.70 | 0.38ŌĆō1.28 | 0.244 | |
| Prophylactic | 2.04 | 1.01ŌĆō4.13 | 0.048* | 1.00 | 1.00ŌĆō1.00 | - | 44.29 | 0.80ŌĆō2446.18 | 0.064 | 57.56 | 1.10ŌĆō3012.99 | 0.045* | 11.98 | 1.78ŌĆō80.77 | 0.011* | 0.65 | 0.13ŌĆō3.16 | 0.592 | 0.08 | 0.00ŌĆō3.43 | 0.187 | 0.12 | 0.01ŌĆō1.82 | 0.125 | 1.26 | 0.45ŌĆō3.54 | 0.662 | |
| Demonstrated symptoms | 0.81 | 0.57ŌĆō1.15 | 0.246 | 1.59 | 0.45ŌĆō5.61 | 0.472 | 1.56 | 0.19ŌĆō12.63 | 0.677 | 1.24 | 0.15ŌĆō9.89 | 0.842 | 0.41 | 0.12ŌĆō1.39 | 0.154 | 0.84 | 0.34ŌĆō2.09 | 0.710 | 0.88 | 0.24ŌĆō3.26 | 0.849 | 0.69 | 0.21ŌĆō2.30 | 0.549 | 0.99 | 0.57ŌĆō1.73 | 0.971 | |
| Ask to Be Tested | 0.98 | 0.47ŌĆō2.05 | 0.954 | 2.82 | 0.25ŌĆō32.26 | 0.405 | - | - | - | - | - | - | 1.00 | 1.00ŌĆō1.00 | - | 2.11 | 0.22ŌĆō20.13 | 0.516 | 1.00 | 1.00ŌĆō1.00 | - | 3.79 | 0.27ŌĆō53.95 | 0.326 | 2.70 | 0.98ŌĆō7.41 | 0.054 | |
| Current Stressors | ||||||||||||||||||||||||||||
| Personal health | 1.12 | 0.97ŌĆō1.29 | 0.123 | 0.73 | 0.39ŌĆō1.35 | 0.313 | 0.60 | 0.27ŌĆō1.34 | 0.211 | 0.70 | 0.31ŌĆō1.57 | 0.387 | 1.11 | 0.70ŌĆō1.77 | 0.647 | 0.95 | 0.67ŌĆō1.36 | 0.795 | 0.77 | 0.49ŌĆō1.21 | 0.259 | 1.27 | 0.79ŌĆō2.03 | 0.320 | 1.32 | 1.07ŌĆō1.63 | 0.009* | |
| Family health | 1.18 | 0.96ŌĆō1.44 | 0.114 | 0.29 | 0.15ŌĆō0.57 | < 0.001* | 1.35 | 0.47ŌĆō3.90 | 0.579 | 1.56 | 0.52ŌĆō4.64 | 0.425 | 1.29 | 0.68ŌĆō2.44 | 0.440 | 1.09 | 0.68ŌĆō1.77 | 0.711 | 1.28 | 0.68ŌĆō2.41 | 0.444 | 0.99 | 0.53ŌĆō1.84 | 0.970 | 0.89 | 0.68ŌĆō1.18 | 0.421 | |
| Community health | 0.98 | 0.85ŌĆō1.13 | 0.821 | 1.12 | 0.62ŌĆō2.02 | 0.714 | 2.25 | 0.98ŌĆō5.14 | 0.056 | 2.02 | 0.87ŌĆō4.68 | 0.102 | 1.74 | 1.10ŌĆō2.76 | 0.018* | 0.73 | 0.51ŌĆō1.03 | 0.074 | 0.88 | 0.57ŌĆō1.37 | 0.576 | 0.70 | 0.44ŌĆō1.12 | 0.135 | 1.01 | 0.82ŌĆō1.24 | 0.941 | |
| Hospital capacity | 0.98 | 0.84ŌĆō1.13 | 0.747 | 1.15 | 0.63ŌĆō2.09 | 0.650 | 1.07 | 0.48ŌĆō2.40 | 0.868 | 1.18 | 0.52ŌĆō2.67 | 0.693 | 1.60 | 1.01ŌĆō2.54 | 0.045* | 1.39 | 0.97ŌĆō1.98 | 0.071 | 0.62 | 0.38ŌĆō1.00 | 0.049* | 2.19 | 1.37ŌĆō3.51 | 0.001* | 1.02 | 0.82ŌĆō1.26 | 0.880 | |
| Timeline to resume clinical practice | 0.94 | 0.81ŌĆō1.08 | 0.358 | 1.44 | 0.80ŌĆō2.60 | 0.227 | 1.04 | 0.47ŌĆō2.29 | 0.917 | 0.95 | 0.43ŌĆō2.11 | 0.898 | 0.96 | 0.61ŌĆō1.52 | 0.876 | 0.94 | 0.66ŌĆō1.33 | 0.721 | 1.11 | 0.72ŌĆō1.72 | 0.640 | 0.71 | 0.44ŌĆō1.14 | 0.160 | 0.83 | 0.68ŌĆō1.03 | 0.087 | |
| Government/leadership | 0.93 | 0.78ŌĆō1.12 | 0.456 | 2.04 | 1.07ŌĆō3.89 | 0.029* | 2.22 | 0.76ŌĆō6.46 | 0.144 | 1.83 | 0.63ŌĆō5.33 | 0.268 | 1.00 | 0.56ŌĆō1.78 | 0.990 | 1.57 | 0.97ŌĆō2.54 | 0.066 | 1.52 | 0.84ŌĆō2.75 | 0.165 | 1.53 | 0.82ŌĆō2.82 | 0.178 | 1.02 | 0.78ŌĆō1.33 | 0.894 | |
| Return to nonessential activities | 1.03 | 0.84ŌĆō1.25 | 0.809 | 1.34 | 0.62ŌĆō2.90 | 0.461 | 1.32 | 0.44ŌĆō3.89 | 0.620 | 1.12 | 0.37ŌĆō3.36 | 0.846 | 1.75 | 0.98ŌĆō3.12 | 0.057 | 1.65 | 0.96ŌĆō2.84 | 0.069 | 1.67 | 0.87ŌĆō3.23 | 0.125 | 1.26 | 0.61ŌĆō2.57 | 0.532 | 1.02 | 0.76ŌĆō1.38 | 0.884 | |
| Economic issues | 0.85 | 0.74ŌĆō0.98 | 0.029* | 0.72 | 0.39ŌĆō1.33 | 0.296 | 1.77 | 0.78ŌĆō4.03 | 0.170 | 1.71 | 0.75ŌĆō3.92 | 0.206 | 0.97 | 0.61ŌĆō1.54 | 0.890 | 0.55 | 0.39ŌĆō0.78 | 0.001* | 1.31 | 0.84ŌĆō2.05 | 0.229 | 0.53 | 0.33ŌĆō0.84 | 0.008* | 0.92 | 0.75ŌĆō1.14 | 0.457 | |
| Clinical Practice | ||||||||||||||||||||||||||||
| Quarantine | 1.02 | 0.86ŌĆō1.21 | 0.786 | 2.10 | 1.10ŌĆō4.01 | 0.025* | 1.34 | 0.52ŌĆō3.44 | 0.541 | 2.29 | 0.89ŌĆō5.91 | 0.086 | 0.78 | 0.43ŌĆō1.43 | 0.429 | 0.67 | 0.45ŌĆō1.01 | 0.056 | 0.89 | 0.54ŌĆō1.47 | 0.645 | 0.52 | 0.29ŌĆō0.93 | 0.028* | 1.19 | 0.94ŌĆō1.51 | 0.143 | |
| Still performing elective surgery | 1.10 | 0.91ŌĆō1.32 | 0.324 | 0.44 | 0.15ŌĆō1.28 | 0.131 | 1.13 | 0.35ŌĆō3.64 | 0.836 | 0.74 | 0.23ŌĆō2.42 | 0.620 | 0.33 | 0.14ŌĆō0.74 | 0.007* | 2.21 | 1.36ŌĆō3.59 | 0.001* | 0.77 | 0.38ŌĆō1.55 | 0.466 | 1.61 | 0.83ŌĆō3.12 | 0.156 | 1.32 | 1.02ŌĆō1.71 | 0.032* | |
| Essential/emergency spine surgery | 0.92 | 0.74ŌĆō1.14 | 0.453 | 0.51 | 0.24ŌĆō1.12 | 0.096 | 1.41 | 0.45ŌĆō4.35 | 0.555 | 2.15 | 0.66ŌĆō7.00 | 0.202 | 0.75 | 0.39ŌĆō1.44 | 0.392 | 2.37 | 1.35ŌĆō4.18 | 0.003* | 0.76 | 0.42ŌĆō1.38 | 0.364 | 0.82 | 0.44ŌĆō1.54 | 0.539 | 0.91 | 0.68ŌĆō1.24 | 0.558 | |
| Advise against | 0.99 | 0.84ŌĆō1.16 | 0.856 | 0.80 | 0.42ŌĆō1.52 | 0.498 | 0.77 | 0.30ŌĆō1.97 | 0.584 | 0.54 | 0.21ŌĆō1.40 | 0.208 | 1.57 | 0.90ŌĆō2.73 | 0.113 | 0.82 | 0.56ŌĆō1.22 | 0.329 | 1.74 | 1.00ŌĆō3.03 | 0.051 | 0.64 | 0.38ŌĆō1.06 | 0.082 | 0.99 | 0.79ŌĆō1.25 | 0.966 | |
| Proceed with standard precautions | 1.07 | 0.89ŌĆō1.30 | 0.393 | 0.26 | 0.08ŌĆō0.88 | 0.065 | 1.10 | 0.39ŌĆō3.10 | 0.691 | 1.47 | 0.52ŌĆō4.21 | 0.308 | 1.63 | 0.93ŌĆō2.87 | 0.247 | 0.95 | 0.60ŌĆō1.51- | 0.946 | 0.63 | 0.32ŌĆō1.21 | 0.090 | 1.37 | 0.76ŌĆō2.47 | 0.242 | 0.96 | 0.73ŌĆō1.27 | 0.879 | |
| Absent during intubation/extubation | 0.83 | 0.72ŌĆō0.97 | 0.059 | 0.72 | 0.39ŌĆō1.34 | 0.767 | 0.84 | 0.36ŌĆō1.96 | 0.961 | 0.89 | 0.38ŌĆō2.10 | 0.927 | 1.03 | 0.64ŌĆō1.65 | 0.611 | 1.27 | 0.88ŌĆō1.83 | 0.139 | 1.06 | 0.66ŌĆō1.70 | 0.850 | 1.20 | 0.73ŌĆō1.95 | 0.222 | 0.78 | 0.62ŌĆō0.97 | 0.060 | |
| Additional PPE during surgery | 0.93 | 0.80ŌĆō1.07 | 0.298 | 1.49 | 0.79ŌĆō2.79 | 0.217 | 1.61 | 0.69ŌĆō3.75 | 0.269 | 2.00 | 0.85ŌĆō4.72 | 0.114 | 0.86 | 0.54ŌĆō1.38 | 0.533 | 1.20 | 0.84 ,1.71 | 0.315 | 0.72 | 0.46ŌĆō1.14 | 0.164 | 1.29 | 0.79ŌĆō2.08 | 0.307 | 0.95 | 0.77ŌĆō1.17 | 0.637 | |
| % Telecommunication clinical visits/wk | 0.96 | 0.84ŌĆō1.10 | 0.556 | 1.66 | 0.93ŌĆō2.96 | 0.085 | 0.68 | 0.32ŌĆō1.46 | 0.325 | 0.83 | 0.39ŌĆō1.79 | 0.639 | 0.99 | 0.64ŌĆō1.54 | 0.961 | 1.74 | 1.25ŌĆō2.43 | 0.001* | 1.11 | 0.72ŌĆō1.71 | 0.651 | 0.72 | 0.45ŌĆō1.15 | 0.168 | 0.82 | 0.67ŌĆō1.00 | 0.050* | |
| Perceived impact in 1 year | ||||||||||||||||||||||||||||
| No change | 1.09 | 0.90ŌĆō1.33 | 0.375 | 0.70 | 0.30ŌĆō1.65 | 0.417 | 1.00 | 0.35ŌĆō2.92 | 0.994 | 1.16 | 0.39ŌĆō3.42 | 0.792 | 0.97 | 0.51ŌĆō1.84 | 0.936 | 1.53 | 0.90ŌĆō2.59 | 0.118 | 1.44 | 0.75ŌĆō2.78 | 0.278 | 2.67 | 1.43ŌĆō5.00 | 0.002* | 0.96 | 0.72ŌĆō1.27 | 0.771 | |
| Heighted awareness of hygiene | 0.88 | 0.76ŌĆō1.03 | 0.264 | 1.22 | 0.64ŌĆō2.30 | 0.467 | 1.66 | 0.71ŌĆō3.86 | 0.831 | 1.63 | 0.69ŌĆō3.85 | 0.938 | 1.06 | 0.65ŌĆō1.75 | 0.924 | 0.76 | 0.52ŌĆō1.12 | 0.149 | 0.65 | 0.40ŌĆō1.05 | 0.174 | 0.44 | 0.27ŌĆō0.72 | 0.001* | 0.96 | 0.77ŌĆō1.19 | 0.712 | |
| Increase use of PPE | 0.92 | 0.79ŌĆō1.07 | 0.486 | 0.97 | 0.52ŌĆō1.81 | 0.880 | 0.85 | 0.37ŌĆō1.95 | 0.697 | 1.24 | 0.53ŌĆō2.88 | 0.670 | 1.07 | 0.66ŌĆō1.75 | 0.694 | 0.68 | 0.47ŌĆō0.98 | 0.099 | 0.50 | 0.31ŌĆō0.80 | 0.011* | 0.62 | 0.38ŌĆō1.01 | 0.110 | 1.22 | 0.98ŌĆō1.52 | 0.083 | |
| Ask patients to reschedule if sick | 1.13 | 0.97ŌĆō1.32 | 0.066 | 0.99 | 0.52ŌĆō1.87 | 0.950 | 0.84 | 0.37ŌĆō1.94 | 0.816 | 0.99 | 0.42ŌĆō2.30 | 0.950 | 1.32 | 0.81ŌĆō2.15 | 0.198 | 0.99 | 0.67ŌĆō1.44 | 0.929 | 1.00 | 0.62ŌĆō1.62 | 0.923 | 1.10 | 0.67ŌĆō1.81 | 0.724 | 1.08 | 0.87ŌĆō1.34 | 0.624 | |
| Increase nonoperative measures prior to surgery | 1.00 | 0.83ŌĆō1.21 | 0.879 | 1.43 | 0.69ŌĆō2.98 | 0.306 | 0.68 | 0.26ŌĆō1.80 | 0.562 | 0.94 | 0.35ŌĆō2.52 | 0.964 | 1.24 | 0.69ŌĆō2.23 | 0.451 | 0.85 | 0.54ŌĆō1.33 | 0.533 | 0.55 | 0.30ŌĆō1.04 | 0.072 | 0.88 | 0.48ŌĆō1.59 | 0.643 | 1.38 | 1.07ŌĆō1.78 | 0.017 | |
| Increase digital options for communication | 1.08 | 0.93ŌĆō1.26 | 0.329 | 1.34 | 0.72ŌĆō2.48 | 0.359 | 1.15 | 0.49ŌĆō2.65 | 0.751 | 1.45 | 0.62ŌĆō3.39 | 0.397 | 1.16 | 0.71ŌĆō1.89 | 0.547 | 1.08 | 0.75ŌĆō1.56 | 0.687 | 0.65 | 0.40ŌĆō1.06 | 0.082 | 0.81 | 0.49ŌĆō1.33 | 0.398 | 0.88 | 0.71ŌĆō1.10 | 0.275 | |
| Other Perceptions | ||||||||||||||||||||||||||||
| Media perceptions | 1.01 | 0.88ŌĆō1.16 | 0.868 | 0.60 | 0.34ŌĆō1.06 | 0.078 | 0.58 | 0.28ŌĆō1.20 | 0.142 | 0.76 | 0.36ŌĆō1.60 | 0.470 | 1.30 | 0.84ŌĆō2.01 | 0.242 | 1.16 | 0.84ŌĆō1.62 | 0.369 | 1.27 | 0.83ŌĆō1.93 | 0.273 | 1.17 | 0.75ŌĆō1.82 | 0.497 | 1.12 | 0.92ŌĆō1.37 | 0.247 | |
| Perception of hospital effectiveness | 1.49 | 1.28ŌĆō1.74 | < 0.001* | 0.62 | 0.34ŌĆō1.12 | 0.115 | 1.60 | 0.68ŌĆō3.77 | 0.283 | 1.27 | 0.53ŌĆō3.04 | 0.592 | 1.26 | 0.77ŌĆō2.06 | 0.362 | 1.99 | 1.39ŌĆō2.85 | < 0.001* | 1.95 | 1.22ŌĆō3.11 | 0.005* | 0.98 | 0.61ŌĆō1.57 | 0.939 | 0.74 | 0.60ŌĆō0.91 | 0.005* | |
| Perception of government effectiveness | 1.14 | 0.99ŌĆō1.32 | 0.073 | 0.62 | 0.35ŌĆō1.10 | 0.105 | 0.89 | 0.42ŌĆō1.92 | 0.770 | 0.84 | 0.39ŌĆō1.82 | 0.653 | 1.19 | 0.75ŌĆō1.90 | 0.467 | 1.15 | 0.81ŌĆō1.63 | 0.449 | 1.13 | 0.71ŌĆō1.78 | 0.608 | 0.87 | 0.55ŌĆō1.39 | 0.572 | 0.93 | 0.76ŌĆō1.14 | 0.483 | |
| Warning patients if the surgeon is COVID-19 positive | 1.40 | 1.18ŌĆō1.67 | < 0.001* | 0.87 | 0.45ŌĆō1.67 | 0.676 | 1.33 | 0.52ŌĆō3.40 | 0.549 | 1.83 | 0.70ŌĆō4.79 | 0.220 | 1.20 | 0.71ŌĆō2.01 | 0.503 | 0.57 | 0.38ŌĆō0.88 | 0.010* | 0.93 | 0.52ŌĆō1.64 | 0.792 | 0.57 | 0.33ŌĆō0.99 | 0.047* | 0.74 | 0.58ŌĆō0.93 | 0.010* | |
All multivariate models were assessed using the same set of independent factors and included baseline demographics, practice, specific variables, and number of medical comorbidities.
Multivariate logistic regression was used to assess survey responses with simple binary outcomes where ordinal logistic regression was implemented for questions with ordinal scales.
COVID-19, coronavirus disease 2019; OR, odds ratio; CI, confidence interval; PPE, personal protective equipment.
REFERENCES

- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























