 |
 |
- Search
|
|
||
Abstract
Adult cervical deformity (ACD) has been shown to have a substantial impact on quality of life and overall health, with moderate to severe deformities resulting in significant disability and dysfunction. Fortunately, surgical management and correction of cervical sagittal imbalance can offer significant benefits and improvement in pain and disability. ACD is a heterogenous disease and specific surgical correction strategies should reflect deformity type (driver of deformity) and patient-related factors. Spinal rigidity is one of the most important considerations as soft tissue releases and osteotomies play a crucial role in cervical deformity correction. For ankylosed, fixed, and severe deformity, 3-column osteotomy (3CO) is often warranted. A 3CO can be done through combined anteriorposterior (vertebral body resection) and posterior-only approaches (open or closed wedge pedicle subtraction osteotomies [PSOs]). This article reviews the literature for currently published studies that report results on the use of 3CO for ACD, with a special concentration on posterior based 3CO (open and closed wedge PSO). More specifically, this review discusses the indications, radiographic corrective ability, and associated complications.
The most common etiologies of adult cervical deformity (ACD) include: remote traumatic injuries, inflammatory spondyloarthropathies, degenerative (arthritic) disease, myopathies, and iatrogenic causes (e.g., postlaminectomy kyphosis or fusion) [1-5]. ACD patients can experience difficulties with maintaining horizontal gaze, gait, and dysphagia, all potentially leading to inability to perform activities of daily living (ADLs) [6]. Secondary to this symptomology, studies have shown that severity of cervical deformity is directly associated with reduced health-related quality of life (HRQoL) scores [7]. Cervical sagittal plane deformity with cervical sagittal vertical axis (cSVA) greater than 4 cm has been shown to be a the critical threshold in which patients begin to have significant pain and disability [7]. In fact, ACD has been shown to be associated with disability scores (based on HRQoL questionnaires) similar to illnesses such as blindness, renal failure, and stroke [8].
There is an ongoing accumulation of evidence that, like in adult spinal deformity (ASD), ACD surgery is able to achieve excellent radiographic correction and provide significant improvement in pain and disability based on HRQoL scores [9-11]. Postoperative cSVA and chin brow vertical angle (CBVA) are 2 radiographic measures that have been closely associated with improvements in ADL and HRQoL outcomes. However, surgical correction of ACD presents numerous challenges given the complex nature of the cervical spine and sensitivity of surrounding vital anatomical structures (neural elements and large vessels such as carotids and vertebral arteries). The optimal surgical strategy can vary widely based on patient-related factors, deformity type, rigidity, imbalance, and/or goals of surgery. In rigid, ankylosed, or focal deformities with large magnitudes of deformity, typically soft tissue releases and low-grade osteotomies are not sufficient and a 3-column osteotomy (3CO) is often warranted (Ames grades 5, 6, and 7) [12]. Ames grade 5 and 6 osteotomies consist of open- and closed wedge pedicle subtraction osteotomy (PSO) which are performed via a posterior-only approach. While Ames grade 7 osteotomy consists of a vertebral body resection (VCR) and is typically achieved from a combined anteriorposterior approach [12].
The use of 3CO in the cervical and upper thoracic spine for ACD is extremely powerful but can be associated with high morbidity in the form of medical and surgical complications. Complication rates following surgery ACD are as high as 43.6%, with mortality ranging from 1.3% to 6.7%, and neurological complication rates ranging from 13.5% to 23.0% [13-16]. Combined anteriorposterior approaches are associated with the highest rates of early complications [15,16]. Therefore, the goals of this article is to review in detail the indications, considerations, and perioperative complications of utilizing 3CO for ACD correction, with special attention to posterior based 3CO (Ames grades 5 and 6 osteotomy).
A comprehensive literature review was performed via a formal PubMed search with the words ŌĆ£cervical deformityŌĆØ and ŌĆ£osteotomy.ŌĆØ Articles and studies with these terms in the title were identified, and the abstracts were carefully reviewed to determine whether posterior based 3CO were utilized within the study cohort or case series. Only articles with adult patients that underwent cervical deformity correction via cervical or upper thoracic 3CO were of interest. Case reports and review articles were excluded. Studies of at least 5 or more patients were included. The cohort and outcomes were then summarized in a table.
The search resulted in a total of 1,124 studies. Among those, 38 were selected for formal abstract review based on a priori criteria. From that, a total of 9 studies from 1997 to 2020 were identified for final review (Table 1) [10,16-23]. All studies were retrospective reviews, with one being a retrospective review of prospectively collected data from the International Spine Study Group. Three of the earliest studies concentrated mainly on cervical open wedge PSO (Ames grade 5) for ankylosing spondylitis (AS) and the 6 more recent studies concentrate on cervical and thoracic closed wedge PSO (Ames grade 6) and upper thoracic VCR. Overall complication rates varied greatly among the identified studies ranging from 10.0% to 60.0%. The incidence of neurological complication varied quite a bit as well from 0.0% to 37.5%.
Preoperative evaluation of all ACD patients should begin with a thorough history, neurological and musculoskeletal examination. During the physical examination, it is essential to evaluate patients standing upright, in both maximal head extension as well as in the position that is most comfortable. The most comfortable position is a critical component in determining the true extent of cervical deformity (kyphosis and cervical sagittal imbalance). Next, it is essential to assess for rigidity by having the patients lay flat on their back with the goal of having the head (occiput) rest on the examination table. Rigid deformities often are unable to do so and are likely candidates for 3CO.
Imaging of ACD should consist of at least 3 imaging modalities: x-rays, computed tomography, and magnetic resonance imagining. It is important to evaluate for presence of thoracolumbar deformity as abnormal cervical alignment maybe compensatory changes or part of concurrent deformities [24,25]. The radiographic indications for 3CO for ACD are related to extent of fusion/ankylosis, degree of deformity, focality of deformity, and/or the main driver of cervical deformity [26]. Patients with 2 or more of the 3 spinal columns fused often require a 3CO release for correction. This is especially the case for patients with focal cervical kyphosis and severe sagittal plane deformity.
The Ames Cervical Osteotomy Grade is a versatile classification and nomenclature system that describes extent of soft tissue release and bony resection, ranging from low grade (grade 1, partial facet joint resection) up to high grade (grade 7, vertebral column resection) [12]. Grades 5 to 7 consist of the 3CO. Grade 5 and 6 are variants of the PSO and approached posteriorly. Grade 7 consists of a VCR and is approached via a combined anteriorposterior approach or posterior-anterior-posterior approach if rare cases.
Grade 5 osteotomy is more commonly known as the open wedge osteotomy. This was first used for cervical deformity correction by Mason et al. [27] in 1953. This osteotomy involves resection of the posterior elements (including the lamina, spinous process, and facets) and often partial resection of the pedicles to facilitate a controlled fracture of the anterior column. Though less frequently used in modern deformity correction, there remains a number of studies describing the use of grade 5 osteotomies for cervical deformity correction; grade 5 osteotomies maybe especially effective for patients with brittle cortical bones as seen in patients with AS [23,28-32]. The largest study to date is by Simmons et al. [22] in which report their results on 131 patients (with 17 patients undergoing more extensive pedicle resections). In their cohort, they achieve a mean CBVA correction of 44.5┬░.
Similar to a grade 5 osteotomy, a grade 6 osteotomy involves resection of the posterior elements, including the lamina, spinous process, and facets. Grade 6 osteotomy includes complete resection of the pedicles and wedge shape resection of the vertebral body (traditional PSO) to facilitate a controlled closure [12]. Given the large amount of bony resection required, grade 6 osteotomies are generally performed at the C7 or upper thoracic spine (T1 to T3) to avoid the vertebral arteries which enter the transverse foramen at C6.
Typically, grade 6 osteotomies (closed wedge PSO) are now preferred over grade 5 osteotomies (open wedge PSO). Grade 6 osteotomy has been purported to be a more controlled corrective technique and associated with lower risk for complication than grade 5 osteotomies. Inducing an anteriorly directed open wedge fracture with grade 5 osteotomy requires elongation of the anterior column and ligament which results in potential vascular, esophageal, tracheal, and neurologic injury [21,23,31,33]. In addition, compared to grade 5 osteotomy, grade 6 osteotomy offers greater biomechanical stability which allows for a controlled closure and bone-on-bone interface which promotes fusion and long-term stability. Studies evaluating closed wedge PSO for the treatment of kyphotic cervical deformity have demonstrated the power of this technique with lower cervical and upper thoracic PSO offering cSVA correction of 2.2 to 4.5 cm, cervical sagittal Cobb correction of 10.1┬░ to 34.5┬░, and average correction CBVA correction of 36.7┬░ [10,16,18,19].
The most extensive release is the grade 7 osteotomy, which involves total resection of one or more entire vertebral bodies, as well as removal of the adjacent disks and the complete uncovertebral joint, facets, and posterior lamina [12]. Given such extensive bony resection, anterior column support is almost always required and may aid in deformity correction with expandable cage options. The grade 7 osteotomy is typically achieved through a combined anteriorposterior approach. The sequential approach depends greatly on the specific deformity being treated. Patients with moderate to severe focal kyphotic deformities in the subaxial cervical spine are the ideal candidates for grade 7 osteotomies, especially if the posterior column is at least semi-flexible or can be overpowered. While grade 7 osteotomies involve the greatest bony resection and spinal release, its use is limited in patient with global cervical kyphosis, deformity primarily from a cervicothoracic driver, and/or severe cervical kyphosis in which the anterior column cannot be readily approached from an anterior approach. If a grade 7 osteotomy is the goal in severely kyphotic patients, a posterior-anteriorposterior approach may be warranted; however, this has been associated with high morbidity and complication rates [13,15,34]. In rare case, an anterior approach may not be possible and posterior based only approaches such as grade 5 and 6 osteotomies are the only options.
There has yet to be an established threshold of postoperative cervical lordosis that has been correlated to outcomes for ACD. In cervical spondylotic myelopathy, there is suggestion that 20 degrees of lordosis maybe associated with benefits in neck pain following surgery [35]. In ACD, cSVA seems to be the most consistent and well supported radiographic parameters in regards to effecting patient long-term outcomes, with the goal of cSVA less than 4 cm [7]. With this in mind, it is essential to identify the main driver of cervical deformity when planning a 3CO: (1) subaxial cervical kyphosis (C3 to C7) and/or (2) forward translation of the cervical spine secondary to pathology in the lower cervical (C6ŌĆō7) or upper thoracic spine (T1ŌĆō3) [36,37]. Both drivers can result in abnormal cervical sagittal imbalance, but patients with lower cervical or upper thoracic drivers can have normal or hyper cervical lordosis. T1-slope is a helpful radiographic parameter that determines whether the driver is located distal to the cervical spine. A T1 slope of greater than 30┬░ is typically indicative of a sagittal deformity involving the upper thoracic spine or even more distal spine [38]. T1-slope can be used with C2-slope to assess the relationship between cervical and thoracolumbar alignment [39]. If C2-slope is low and T1-slope is high, this suggests the driver of deformity is distal to the cervical spine. If C2 slope is high and T1 slope is low, then this indicates a primarily cervical spine driven deformity. A difference of greater than 17┬░ between the T1 slope and CL also suggests a cervical deformity, even with a concurrent thoracolumbar deformity present. A combined cervical and distal deformity can often present with C2-slope and T1-slope both being high.
Following identification of the main driver for ACD, planning a 3CO at the appropriate level is critical in order to achieve the correction desired. Subaxial ACD with focal kyphotic deformities often has to be addressed with the 3CO at the apex. However, in patients with more global subaxial kyphosis, a 3CO at C6 or C7 is often preferred given the lower risk for devastating neurological injury and vertebral artery injury compared to more proximal cervical levels (C5 and above) [40-42]. ACD patients with mainly cervical sagittal imbalance from a deformity driver located at or distal to the cervicothoracic junction should undergo 3CO in the upper thoracic spine. Traditionally, a 3CO at the cervicothoracic junction was preferred, but there is a push towards transitioning 3CO to more distal levels, specially PSO at T2 or T3 to minimize nerve root injury and related weakness [16,17]. The incidence of neurological complications has been shown to decreases with more distal levels: C7 (37.5%), T1 (37.5%), T2 (20.0%), T3 (15.4%), T4 (0.0%) [16]. In addition, 3CO at T2 has been shown to offer the greatest C2 to T3 angular change (39.1┬░) compared to 3CO at C7 (16.9┬░), T1 (13.5┬░), and T3 (15.7┬░) [37].
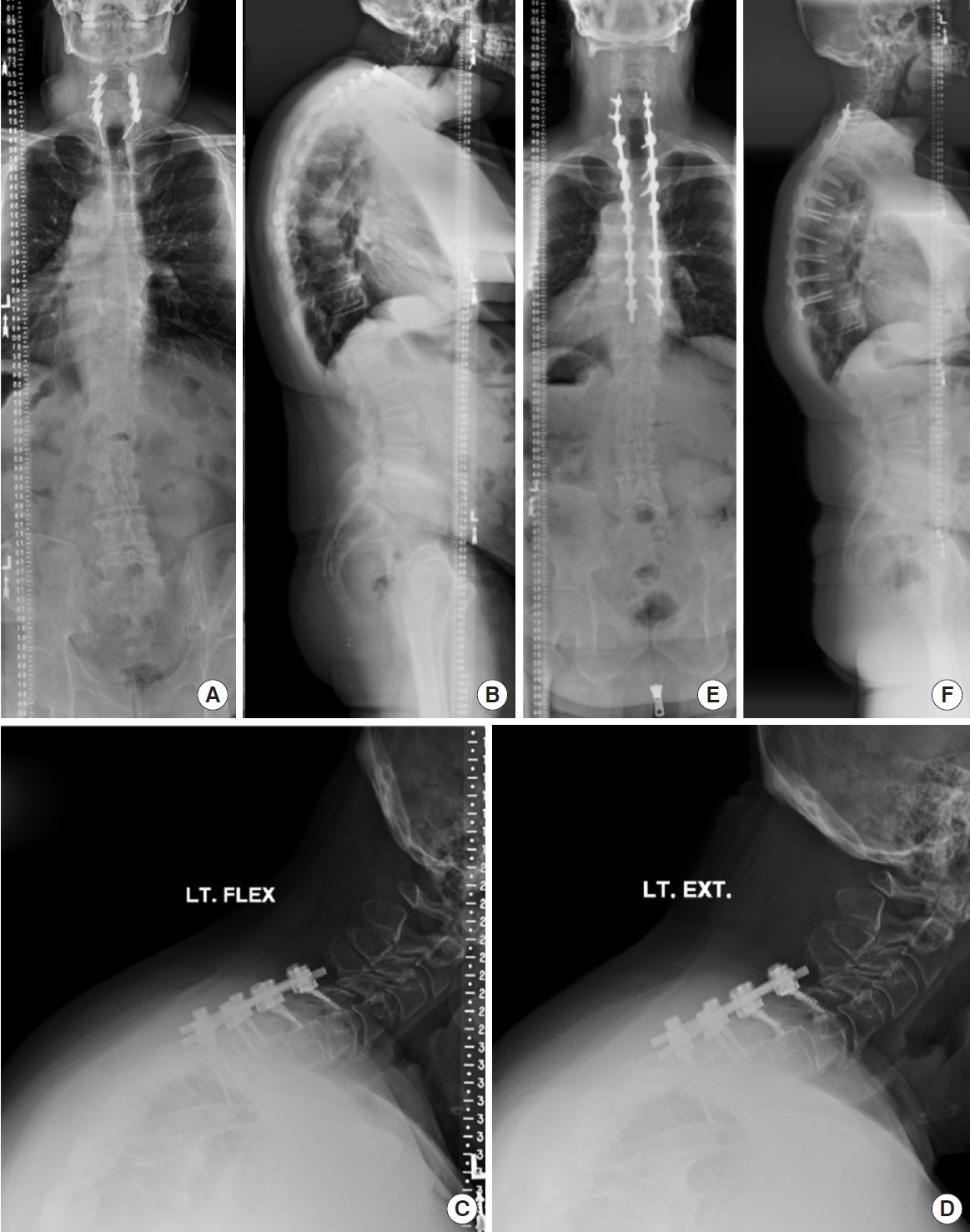
Fig. 1 illustrates a patient who presented with a history of C5 to T1 posterior spinal fusion/instrumentation (PSF/I) and severe cervical sagittal imbalance with a cSVA of 10.4 cm and an abnormally high T1-slope of 45┬░. He had normal cervical lordosis of 9┬░. The patientŌĆÖs primary driver of cervical deformity was in his upper thoracic spine. Flexion-extension films demonstrate a rigid deformity. He underwent revision, C5 to T9 PSF/I, T2 PSO (Ames grade 6 osteotomy). Postoperatively his cervical parameters were normalized with cSVA 4.1 cm, cervical lordosis 11┬░, and T1-slope of 25┬░.
Adequate spinal fixation is critical in order to safely close a 3CO, especially in cases that require large translational correction. Unlike the robust fixation that can be readily achieved in the adult thoracolumbar spine, reliable and confident cervical spine fixation can be difficult. The most common mechanism of failure at the upper instrumented vertebrae (UIV) is screw pull out especially with the use of lateral mass screw fixation in the midsubaxial spine. Therefore, there should be consideration to choose C2 as the UIV and/or utilize pedicle screw fixation. There is strong biomechanical evidence that C2 pedicle screws (vs. C2 pars screws) and subaxial (C3 to C7) cervical pedicle screws (vs. lateral mass screws) have significantly greater pull out strength [43,44]. C2 pedicle screws have an average pullout strength 92% stronger than a C2 pars screw [44], and subaxial cervical pedicle screws have at least twice the strength of lateral mass screws [43]. For correction of subaxial cervical kyphosis lower instrumented vertebrae (LIV) above the thoracic apex is generally sufficient. In cases of 3CO near the cervicothoracic junction or upper thoracic spine, the optimal LIV remains to be studied. Currently, some would consider LIV past the thoracic apex near T10 [26].
It has been shown that patients who undergo a 3CO for ACD correction have significant improvements in HRQoL outcomes, as measured by neck disability index scores, neck visual analogue pain scores, and 36-Item Short Form Survey physical component scores [10,18]. However, the treatment of rigid, severe ACD can be technically challenging because of the proximity of the cervical spine to several vital and relatively delicate structures. This results in potential risk for complications with serious morbidity (include injury to the vertebral artery, esophagus, trachea, sympathetic nerve roots, cervical nerve roots, and/or the spinal cord itself). A prospective study by Smith et al. [15] of 78 patients who underwent surgery for ACD, reported an overall complication rate of 43.6%. Similarly, in a retrospective study of 95 patients who underwent ACD deformity correction by Lau et al. [16] reported a complication rate of 37.9%. The most common perioperative complications being nerve root weakness, surgical site infection, dysphagia, and comorbid medical-related complications. Independent risk factors for complication include sex (male), and deformity severity (cSVA greater than 8 cm and kyphosis greater than 20┬░), and surgical approach (posterior-only vs. combine anteriorposterior) [15,16].
It has been shown that combined anteriorposterior approaches (such as Ames grade 7 osteotomies/VCR) are associated with the highest rate of complications at 79.3%, while posterior-only approaches were lower at 68.4% [15]. Many patients with moderate to severe ACD will experience postoperative dysphagia regardless of approach (secondary to esophageal lengthening), especially in those who already have preoperative esophageal dysfunction [45]. However, the incidence of symptomatic dysphagia is significantly lower with posterior-only approaches compared to combined anteriorposterior approaches (2.6% vs. 24.1%, respectively) [15]. In addition, the anterior approach can result in unidentified esophageal injuries. Therefore, there is a push towards utilizing posterior-only based approaches to 3CO via Ames grade 6 osteotomy (closed wedge PSO) when at all possible.
There remains a paucity of literature strictly dedicated to the study of complications following 3CO for ACD. Among the available ACD 3CO literature, reported perioperative complications rates range from 10.0% to 56.5% with larger case series showing higher rates of complication [10, 16-23]. When performing 3CO (compared to lower grade osteotomies), greater blood loss and higher risk for neurological morbidity should be taken into serious consideration. The reported neurological deficit rate following 3CO for ACD range between 0.0% to 37.5% [10,16-23]. A more recent study by Lau et al. [16] compared neurological deficit rates between posterior based low grade and high grade (3CO) for ACD correction among 95 patients. 3CO patients experience a new neurological deficit rate 20.4% of the time compared to 13.0% in low-grade ostoetomies. With regards to neurological deficits following PSO, nerve root injury in the form of direct compression or corrective stretch injury (neuropraxia) is much more common than spinal cord injury. In particular, the C8 nerve root is most at risk when PSO is performed at the lower cervical and T1 levels. The nerve root is at risk during bony resection, closure of the osteotomy (direct compression of surrounding structures such as T1 rib head), and following correction (stretch/neuropraxia). Patients need to be formally and thoroughly counseled regarding risk for hand weakness and numbness. The long-term outcomes to C8 palsy have yet to be thoroughly studied and therefore its natural history is less understood than C5 palsy following cervical spine surgery. 3CO at T2 or T3 may mitigate this risk [18]. In addition, patients who undergo lower cervical 3CO have significantly higher complication rates (60.0% vs. 27.3%), longer intensive care unit (6.0 days vs. 1.6 days), and hospital stays (15.0 days vs. 7.5 days). This is secondary to more patients requiring a tracheostomy and/or gastrostomy tube after lower cervical 3CO [18].
In a review of the literature conducted by Etame et al. [13], they showed that medical complication rates for ACD surgery patients vary dramatically from 3.1% to 44.4%. In general, ACD patients tend to be frailer than the average ASD patient. ACD patients often struggle with myelopathy and severe calorie deficits and malnutrition. In addition to comorbid chronic conditions, this theoretically results in lower physiologic reserve. Fortunately, ACD patients who undergo 3CO (compared to low grade osteotomy) do not experience high rates of medical complications [16].
ACD, particularly cervical kyphosis and sagittal imbalance, can result in significant pain, disability, and myelopathy due to spinal cord injury even in the absence of cervical stenosis. Correction of cervical spinal parameters, especially cSVA and CBVA are associated with significant improvements in gait, horizontal gaze, and patient HRQoL outcomes. For ACD patients with rigid, focal and/or severe deformities, 3CO should be considered in order achieve adequate correction. Ames grade 5 to 7 osteotomies are 3CO, with grade 5 and 6 being posterior-only approaches and grade 7 requiring a combined anteriorposterior approach. Considerations to 3CO should include identification of the main driver of cervical deformity (subaxial kyphosis or cervicothoracic junction imbalance (high T1-slope). In turn, this will aid in planning the 3CO level in which the goals are to perform the osteotomy at the most distal level possible, preferably T2. Perioperative complications following 3CO for ACD are relatively high with combined anteriorposterior approaches associated with the highest risk for complication and nerve root weakness remains a serious concern. Nonetheless, 3CO for ACD allows for the greatest extent of correction in severely deformed patients. Thus, with careful surgical planning and preoperative optimization, 3CO is a vital tool to improve the function and quality of life of cervical deformity patients.
Fig.┬Ā1.
T2 pedicle subtraction osteotomy (PSO) for correction of rigid adult cervical deformity. Panels A and B show prior C5 to T1 posterior spinal fusion/instrumentation (PSF/I) and severe cervical sagittal imbalance with cervical sagittal vertical axis (cSVA) of 10.4 cm, T1-slope of 45┬░, and cervical lordosis 9┬░. (C, D) Flexion-extension films demonstrate no movement. He underwent removal of implants, revision C5 to T9 PSF/I, and T2 PSO (Ames grade 6 osteotomy) for deformity correction. Postoperatively his cervical parameters were normalized with cSVA 4.1 cm, cervical lordosis 11┬░, and T1-slope of 25┬░.
Table┬Ā1.
Tabulated summary of studied examining cervical and thoracic three column osteotomy for cervical deformity
| Study | No. of patients | 3CO type | Extent of correction | Overall complications | Neurological complications | Comments |
|---|---|---|---|---|---|---|
| Lau et al. [16] (2020) | 49 | PSO, VCR | cSVA: 2.1 cm | 42.9% | 20.4% | cSVA > 8 cm and cervical kyphosis > 20┬░ associated with higher surgical complication |
| CL: 9.1┬░ | ||||||
| T1-slope: 13.1┬░ | ||||||
| Smith et al. [17] (2017) | 23 | PSO, VCR | cSVA: 2.2 cm | 56.6% | 17.4% | Most common complications were neurologic deficit, infection, DJK, and cardiorespiratory failure |
| CL: 10.1┬░ | ||||||
| T1-slope: 6.5┬░ | ||||||
| Theologis et al. [18] (2015) | 48 | PSO, VCR | Cervical | Cervical: 60.0% | Cervical: 6.7% | Cervical 3CO more complications and longer hospital and ICU stays |
| ŌĆācSVA: 3.8 cm | Thoracic: 27.3% | Thoracic: 6.1% | ||||
| ŌĆāCL: 2.2┬░ | ||||||
| ŌĆāT1-slope: 3.6┬░ | ||||||
| Thoracic | ||||||
| ŌĆācSVA: 1.8 cm | ||||||
| ŌĆāCL: 11.2┬░ | ||||||
| ŌĆāT1-slope: 15.4┬░ | ||||||
| Kim et al. [19] (2015) | 10 | PSO | CL: 36.6┬░ | 10.0% | 0% | |
| Angular correction: 44.8┬░ | ||||||
| Translational correction: 3.8 cm | ||||||
| Deviren et al. [10] (2011) | 11 | PSO | cSVA: 4.5 cm | 36.4% | 0% | Improvement of NDI and SF-36 questionnaires at all follow-up time points |
| PSO correction angle: 19.0┬░ | ||||||
| Samudrala et al. [20] (2010) | 8 | PSO | CTJ angle: 38.7┬░ | n/a | 37.5% | |
| CBVA: 36.3┬░ | ||||||
| Tokala et al. [21] (2007) | 8 | Open wedge PSO | CTJ angle: 57┬░ | n/a | 37.5% | No permanent injuries at 2 years |
| CBVA: 35┬░ | ||||||
| Simmons et al. [22] (2006) | 131 | Open wedge (with 17 undergoing pedicle resections) | CBVA: 44.5┬░ | 23.0% | 16.0% | Ankylosing spondylitis, mortality 3.1% |
| McMaster et al. [23] (1997) | 15 | Open wedge with minimal pedicle resection | 54┬░ of kyphosis correction | 60.0% | 20.0% | Ankylosing spondylitis |
3CO, 3-column osteotomy; PSO, pedicle subtraction osteotomy; VCR, vertebral body resection; cSVA, cervical sagittal vertical axis; CL, cervical lordosis; DJK, distal junctional kyphosis; ICU, intensive care unit; NDI, Neck Disability Index; SF-36, 36-Item Short Form Survey; CTJ, cervicothoracic junction; CBVA, chin brow vertical angle.
REFERENCES
1. Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013 38:S149-60.


2. Steinmetz MP, Stewart TJ, Kager CD, et al. Cervical deformity correction. Neurosurgery 2007 60:S90-7.



3. OŌĆÖShaughnessy BA, Liu JC, Hsieh PC, et al. Surgical treatment of fixed cervical kyphosis with myelopathy. Spine (Phila Pa 1976) 2008 33:771-8.


4. Kaptain GJ, Simmons NE, Replogle RE, et al. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg 2000 93:199-204.


6. Griegel-Morris P, Larson K, Mueller-Klaus K, et al. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther 1992 72:425-31.



7. Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012 71:662. -9. discussion 9.



8. Smith JS, Line B, Bess S, et al. The health impact of adult cervical deformity in patients presenting for surgical treatment: comparison to united states population norms and chronic disease states based on the EuroQuol-5 Dimensions Questionnaire. Neurosurgery 2017 80:716-25.



9. Suk KS, Kim KT, Lee SH, et al. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976) 2003 28:2001-5.


10. Deviren V, Scheer JK, Ames CP. Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine 2011 15:174-81.


11. Kim KT, Lee SH, Son ES, et al. Surgical treatment of ŌĆ£chin-on-pubisŌĆØ deformity in a patient with ankylosing spondylitis: a case report of consecutive cervical, thoracic, and lumbar corrective osteotomies. Spine (Phila Pa 1976) 2012 37:E1017-21.


12. Ames CP, Smith JS, Scheer JK, et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine 2013 19:269-78.


13. Etame AB, Wang AC, Than KD, et al. Outcomes after surgery for cervical spine deformity: review of the literature. Neurosurg Focus 2010 28:E14.

14. Etame AB, Than KD, Wang AC, et al. Surgical management of symptomatic cervical or cervicothoracic kyphosis due to ankylosing spondylitis. Spine (Phila Pa 1976) 2008 33:E559-64.


15. Smith JS, Ramchandran S, Lafage V, et al. Prospective multicenter assessment of early complication rates associated with adult cervical deformity surgery in 78 patients. Neurosurgery 2016 79:378-88.



16. Lau D, Deviren V, Joshi RS, et al. Comparison of perioperative complications following posterior column osteotomy versus posterior-based 3-column osteotomy for correction of rigid cervicothoracic deformity: a single-surgeon series of 95 consecutive cases. J Neurosurg Spine 2020 May 8 1. -10. https://doi.org/10.3171/2020.3.SPINE191330. [Epub].


17. Smith JS, Shaffrey CI, Lafage R, et al. Three-column osteotomy for correction of cervical and cervicothoracic deformities: alignment changes and early complications in a multicenter prospective series of 23 patients. Eur Spine J 2017 26:2128-37.



18. Theologis AA, Tabaraee E, Funao H, et al. Three-column osteotomies of the lower cervical and upper thoracic spine: comparison of early outcomes, radiographic parameters, and peri-operative complications in 48 patients. Eur Spine J 2015 24 Suppl 1:S23-30.



19. Kim HJ, Piyaskulkaew C, Riew KD. Comparison of Smith-Petersen osteotomy versus pedicle subtraction osteotomy versus anterior-posterior osteotomy types for the correction of cervical spine deformities. Spine (Phila Pa 1976) 2015 40:143-6.


20. Samudrala S, Vaynman S, Thiayananthan T, et al. Cervicothoracic junction kyphosis: surgical reconstruction with pedicle subtraction osteotomy and Smith-Petersen osteotomy. Presented at the 2009 Joint Spine Section Meeting. Clinical article. J Neurosurg Spine 2010 13:695-706.


21. Tokala DP, Lam KS, Freeman BJ, et al. C7 decancellisation closing wedge osteotomy for the correction of fixed cervicothoracic kyphosis. Eur Spine J 2007 16:1471-8.




22. Simmons ED, DiStefano RJ, Zheng Y, et al. Thirty-six years experience of cervical extension osteotomy in ankylosing spondylitis: techniques and outcomes. Spine (Phila Pa 1976) 2006 31:3006-12.


23. McMaster MJ. Osteotomy of the cervical spine in ankylosing spondylitis. J Bone Joint Surg Br 1997 79:197-203.


24. Oh T, Scheer JK, Eastlack R, et al. Cervical compensatory alignment changes following correction of adult thoracic deformity: a multicenter experience in 57 patients with a 2-year follow-up. J Neurosurg Spine 2015 22:658-65.


25. Ha Y, Schwab F, Lafage V, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J 2014 23:552-9.



26. Smith JS, Klineberg E, Shaffrey CI, et al. Assessment of surgical treatment strategies for moderate to severe cervical spinal deformity reveals marked variation in approaches, osteotomies, and fusion levels. World Neurosurg 2016 91:228-37.


27. Mason C, Cozen L, Adelstein L. Surgical correction of flexion deformity of the cervical spine. Calif Med 1953 79:244-6.
28. Simmons EH. The surgical correction of flexion deformity of the cervical spine in ankylosing spondylitis. Clin Orthop Relat Res 1972 86:132-43.


29. Mehdian SM, Freeman BJ, Licina P. Cervical osteotomy for ankylosing spondylitis: an innovative variation on an existing technique. Eur Spine J 1999 8:505-9.




30. Mehdian S, Arun R. A safe controlled instrumented reduction technique for cervical osteotomy in ankylosing spondylitis. Spine (Phila Pa 1976) 2011 36:715-20.


31. Belanger TA, Milam RAt, Roh JS, et al. Cervicothoracic extension osteotomy for chin-on-chest deformity in ankylosing spondylitis. J Bone Joint Surg Am 2005 87:1732-8.


32. Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop Relat Res 1977 (128):65-77.

33. Herbert JJ. Vertebral osteotomy for kyphosis, especially in Marie-Strumpell arthritis; a report on fifty cases. J Bone Joint Surg Am 1959 (41-A):291. -302. passim.


34. Koerner JD, Kepler CK, Albert TJ. Revision surgery for failed cervical spine reconstruction: review article. HSS J 2015 11:2-8.



35. Lau D, Winkler EA, Than KD, et al. Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy: influence of cervical alignment on outcomes. J Neurosurg Spine 2017 27:508-17.


36. Passias PG, Jalai CM, Lafage V, et al. Primary drivers of adult cervical deformity: prevalence, variations in presentation, and effect of surgical treatment strategies on early postoperative alignment. Neurosurgery 2018 83:651-9.



37. Passias PG, Horn SR, Raman T, et al. The impact of osteotomy grade and location on regional and global alignment following cervical deformity surgery. J Craniovertebr Junction Spine 2019 10:160-6.



38. Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 2010 10:994-8.


39. Protopsaltis TS, Ramchandran S, Tishelman JC, et al. The importance of C2 slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine (Phila Pa 1976) 2020 45:184-92.


40. Wollowick AL, Kelly MP, Riew KD. Pedicle subtraction osteotomy in the cervical spine. Spine 2012 37:E342-8.


41. Kim HJ, Nemani VM, Daniel Riew K. Cervical osteotomies for neurological deformities. Eur Spine J 2015 24 Suppl 1:S16-22.



42. Yuk FJ, Rasouli JJ, Arginteanu MS, et al. The case for T2 pedicle subtraction osteotomy in the surgical treatment of rigid cervicothoracic deformity. J Neurosurg Spine 2019 32:248-57.


43. Barnes AH, Eguizabal JA, Acosta FL Jr, et al. Biomechanical pullout strength and stability of the cervical artificial pedicle screw. Spine (Phila Pa 1976) 2009 34:E16-20.






























