|
 |
- Search
Abstract
Objective
The aim of this study was to compare geometrically cross-sectional areas of two different laminoplasty techniques in same opening size.
Some investigators have studied the expanded areas of the two different techniques using imaging study. Although it is unclear that postoperative spinal canal is correlated with the surgical outcome we just focused on mathematical and geometrical correlation of the expandable area with surgical opening size in different laminoplasty techniques.
Methods
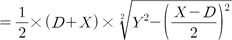
To predict the expandable area by a midline splitting technique and a unilateral open door technique, we placed an imaginary isosceles triangle in the spinal canal and drew graphs for the equation of the expandable areas in same opening size using the Pythagorean theorem and mathematical program. To substitute the constant figures of mathematical formula we estimated the normal cervical spine CT scans of 50 Korean adults.
Results
We subtracted the imaginary triangle from the spinal canal and were left with the remaining area of the spinal canal that was not changed before and after surgery. In same opening size the expandable area by the midline splitting technique was same but slightly wider than the unilateral open door technique, irrespective of the triangular shape. For a normal isosceles triangle the results were the same.
Many spine surgeons have spared no effort in the treatment of cervical compressive myelopathies. Anterior cervical procedure or cervical laminoplasty has been the treatment of choice for patients with cervical myelopathy resulting from cervical spondylosis, ossification of the posterior longitudinal ligament. Laminoplasty procedures can be traditionally classified into unilateral open door techniques (UODT) and midline splitting techniques (MST).
Some investigators have studied the expanded areas of the two different techniques. The common points of their reports include the use of an image analyzing program for the expanded area. However, we proposed some possible errors in the process. First, the image analyzing method is not quite accurate, even if the image is magnified. Second, there are variable differences in the measured area by different persons or repetitive measures, as we repeat measurement of the area. Third, where is the margin of the measuring area on the level of the neural foramen? Fourth, postoperative image may not be the same section as preoperative one.
The canal area and volume may not be correlated with the surgical result, but it should be clarified that the spinal canals were different in the areas and volumes after different surgical techniques.
We have designed the experimental measurements for the expandable area of hypothetical spinal canal. Furthermore, we have tried to compare the expandable areas for different laminoplasty techniques.
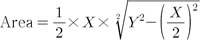
We have drawn an isosceles triangle into the cross-sectional image of the spinal canal (Fig. 1). Line X is a horizontal line through the inner points of the surgical gutters. To define the inner points of the surgical gutters, we drew an intersection point from the posterior border between the lateral mass and the lamina. Then, we estimated the nearest point on the inner surface of the lamina to this intersection point, and defined the inner points of the surgical gutters. Line Y is an oblique line between the midpoint on the inner surface of the lamina and the inner point of the surgical gutter. The expandable area after laminoplasty (UODT or MST) was assessed with triangular and extra-triangular areas (Fig. 2).
In order to apply the normal triangle, cervical spine computed tomography (CT; Light-speed Ultra 8, General Electric, Milwaukee, WI) was performed on 50 normal cases that had no previous spinal surgery or disease (25 males and 25 females with a mean age of 26.7 years [range, 17-40 years]) between September 2007 and January 2008. The position of the gantry angle was maintained perpendicular to the spinal canal when obtaining the cross-sectional measurement. The window angle was set at 570 and the window width was set at 3,077. We identified and evaluated the cross-sectional areas of the spinal canal at two levels, including the mid-C5 and foraminal level of the C5 nerve root. The distance and area measurements were performed directly on the CT image using a General Electric PACS viewer. Calculations and the graphics of equations were performed using Matlab 7.1 software.
The laminoplasty opening size (line D) was defined as the distance between the split points at the opened laminae (Wang et al.8)). The distance of line Y was not changed after UODT or MST. Since the sine equation using an angle was expected to be somewhat inaccurate, we used the Pythagorean theorem for the equation of an expanded area and applied to the UODT (Fig. 2A) and MST (Fig. 2B).
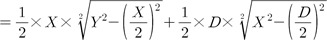
This area was not likely to apply to this study. But the imaginary isosceles triangle could give us an easy solution (Fig. 3). The excluded area was not changed after any technique compared to the previous one. During the procedure, the groove must be made, but the groove is not only very small, but also bears no relation with the spinal cord and nerve root. Even though line Y decreases after the opening procedure, a little loss of line Y can be included in the laminoplasty opening size and considered before surgery.
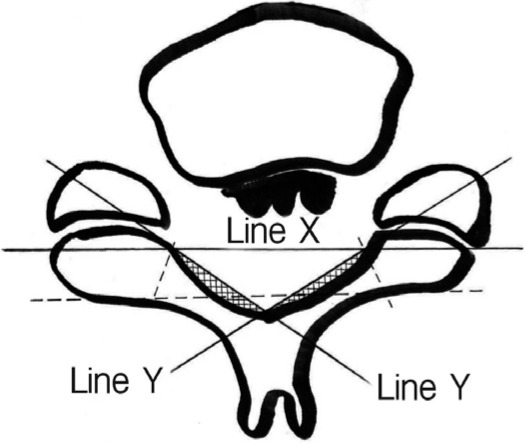
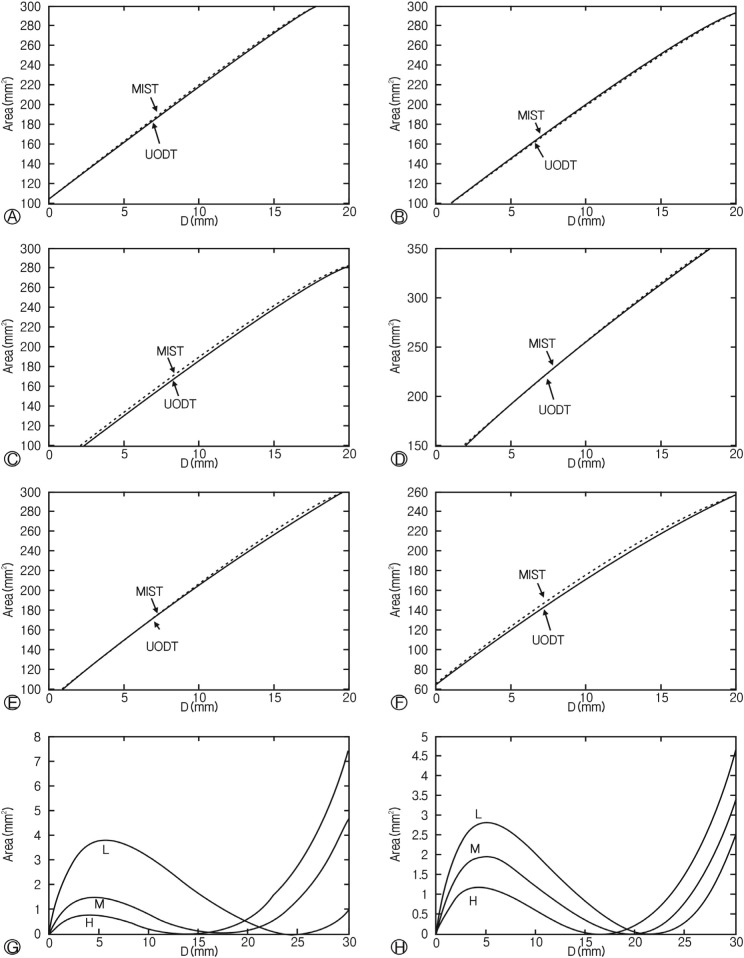
The mean distance of line X and line Y was 22.92mm (range, 21.2-26.3) and 13.78mm(range, 12.9-15.6) at the mid-C5 level, respectively, and 23.56mm(range, 20.6-26.3) and 14.02mm(range, 12.4-16.2), at the C4-5 neural foraminal level, respectively. Using variables (shortest, mean, and longest) for the height of the normal isosceles triangle, we expect differences between the expanded area after the two techniques (Fig. 4). The graphs of MST were lined just over those of UODT. In same opening size the expandable area by the midline splitting technique was same but slightly wider than the unilateral open door technique, irrespective of the triangular shape.
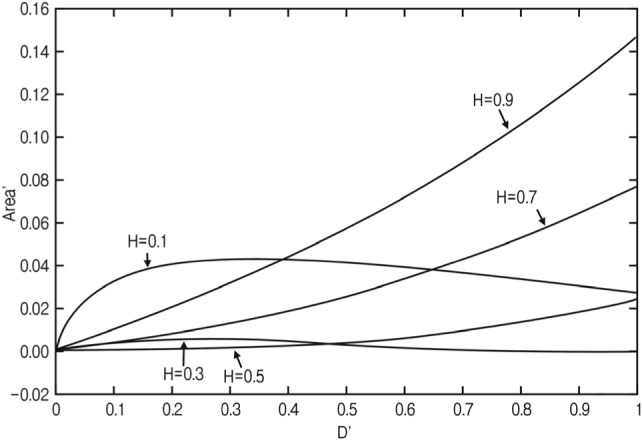
Although the distance, D, was applied to the mean area of the imaginary isosceles triangle using the Matlab program, the expanded areas after the MST were larger than after the UODT. We achieved the same results for triangles that had the largest and smallest ratios of height to X (Fig. 5). The graphs (Area'=area of MST-area of UODT) show that areas of two techniques had no significant difference when height to X is about 0.5, but all graphs were lined over zero.
The main goal of cervical laminoplasty is a widening of the spinal canal with preservation of the posterior elements for maintaining the stability of the cervical spine. Among the various methods of compressive cervical myelopathy, the UODT and the MST are the most popular methods. Some investigators have studied the differences in radiologic and clinical results between the two methods.
O'brien et al. reported that computer-assisted morphometric analysis of UODT was performed on preoperative and postoperative CT scans; the preoperative sagittal canal diameter was 8.2┬▒0.96mm and the canal area was 180.6┬▒33.7mm2.7) These dimensions increased after surgery to 16.6┬▒1.5mm and 321.9┬▒29.7mm2, respectively7). Itoh et al. reported the extent of the enlargement of the canal was 4.1mm on the average in the anteroposterior diameter4), and in no case was a significant reduction in the diameter of the canal noted during the follow-up period. Hirabayashi et al. reported that optimal widening of the AP diameter of the spinal canal is considered to be >4mm3).
Hamburger et al. reported that all patients with a postoperative area >160mm2 reached a Japanese Orthopedic Association score higher than 12, whereas 6 patients with a smaller postoperative area only had scores between 4 and 10.22). They used pixel-dependent area calculation software for the area measurement. Kohno et al. assessed the anteroposterior diameter and the area of the residual spinal canal using a microcomputer imaging device and the stenotic cervical canal could be enlarged to the normal range (over 12mm residual AP diameter and 200mm2 residual canal area)5).
Baek et al. compared the expansion ratios of the axial canal area between the UODT group (27 patients) and the MST group (10 patients) using a picture archiving and communication system. The increase in the postoperative axial canal area was 63.23┬▒23.24% in the UODT group and 42.30┬▒14.96% in the MST group, demonstrating a statistically significant difference between the two groups 1).
Wang et al. reported that the differences between the postoperative canal increase in the sagittal diameter and canal area for the UODT versus the MST were statistically significant when the door was opened by >12mm. They measured the canal area by computer-assisted surgery simulation systems, but they found no clinical differences between the two groups8).
Naito et al. reported that there were no significant difference in clinical results and sagittal diameter among three operations (Z-plasty, UODT, and MST), and excellent or good results were obtained in >70% of the patients6).
In the current study, the expanded area of the MST was slightly larger than that of the UODT but nearly same. The result of the current study is different from previous reports. We presume that previous results had some limitations, like small case series, hand-drawing errors, differences between preoperative and postoperative images and little reproducibility, and automatic analysis limitations. The automatic analysis method may be more accurate than the manually drawing method, but the method must be hard to apply at the foraminal level and its processes can change the area.
The isosceles triangular application also had an error in surgical defects, especially the splitting site. We believe the hypothetical key for the expanded area must be mathematics, on the other hand we worry about its simplicity and lack of clinical correlation.
We designed hypothetical model and equation for the expanded area. When applied to the imaginary triangle method, the expandable area after the two technique will be nearly same irrespective of the lamina opening size. If a surgeon determines the opening size preoperatively or intraoperatively, there will be little difference between expandable areas of the MST and the UODT.
References
1. Baek HC, Kang SH, Jeon SR, Roh SW, Rhim SC. Comparison of early surgical outcome between unilateral open-door laminoplasty and midline splitting laminoplasty. J Korean Neurosurg Soc 2007 41:382-386.
2. Hamburger C, Buttner A, Uhl E. The cross-sectional area of the cervical spinal canal in patients with cervical spondylotic myelopathy. Correlation of preoperative and postoperative area with clinical symptoms. Spine (Phila Pa 1976) 1997 22:1990. -1994. discussion 1995. PMID: 9306528.


3. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983 8:693-699. PMID: 6420895.


4. Itoh T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine (Phila Pa 1976) 1985 10:729-736. PMID: 3909451.


5. Kohno K, Kumon Y, Oka Y, Matsui S, Ohue S, Sakaki S. Evaluation of prognostic factors following expansive laminoplasty for cervical spinal stenotic myelopathy. Surg Neurol 1997 48:237-245. PMID: 9290710.


6. Naito M, Ogata K, Kurose S, Oyama M. Canal-expansive laminoplasty in 83 patients with cervical myelopathy. A comparative study of three different procedures. Int Orthop 1994 18:347-351. PMID: 7698864.


7. O'Brien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine (Phila Pa 1976) 1996 21:474. -483. discussion 484. PMID: 8658252.


8. Wang XY, Dai LY, Xu HZ, Chi YL. Prediction of spinal canal expansion following cervical laminoplasty: A computer-simulated comparison between single and double-door techniques. Spine (Phila Pa 1976) 2006 31:2863-2870. PMID: 17108843.


Fig.┬Ā2
(A) Line X, Y and D of isosceles trapezoid after MST. (B) After UODT, preoperative imaginary triangle was rotated posteriorly.
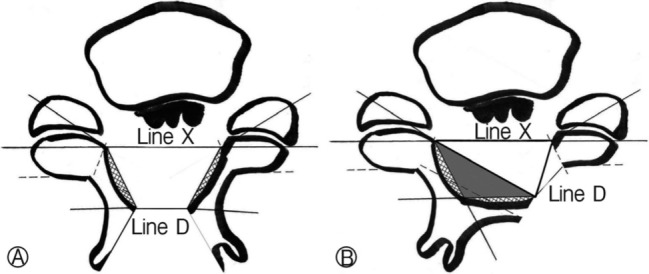
Fig.┬Ā3
Panel (A) and (C) show the excluded area (black area) from imaginary triangle. After laminoplasty (panel (B): midline splitting technique, panel (D): unilateral open door technique) black area was moved, but not changed.
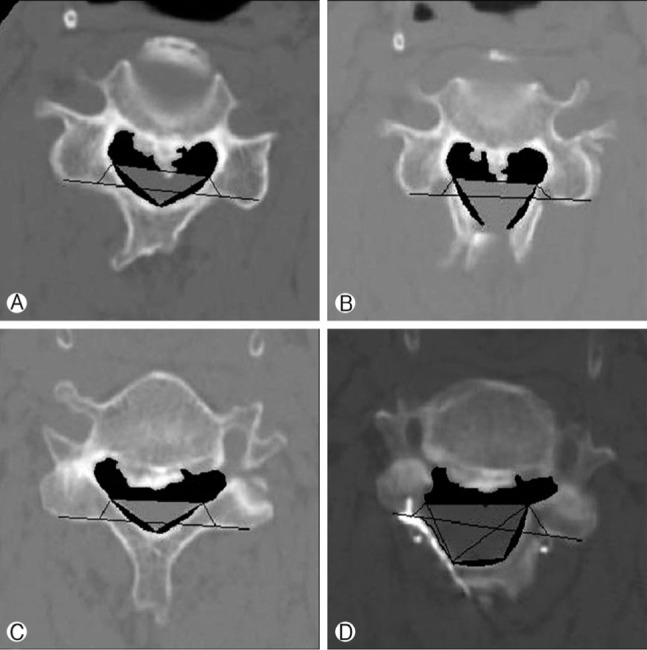
Fig.┬Ā4
Graphs for expandable areas of real triangles. (A) highest triangle on C5 level, (B) triangle with mean height on C5 level, (C) lowest triangle on C5 level, (D) highest triangle on C5 foraminal level, (E) triangle with mean height on C5 foraminal level, (F) lowest triangle on C5 foraminal level, (G) difference between MST and UODT on C5 level, (H) difference between MST and UODT on C5 foraminal level.

- TOOLS
-
METRICS

-
- 3 Crossref
- Scopus
- 5,345 View
- 53 Download
- Related articles in NS
-
Journal Impact Factor 3.2