Transforaminal Endoscopic Discectomy for Large, Two Level Calcified, Thoracic Disc Herniations With 5-Year Follow-up
Article information
Abstract
To describe technical details and benefits of transforaminal endoscopic discectomy for treatment of patients with large, dorsomedial, calcified thoracic disc herniations at 2 levels and to report on their clinical outcomes in long follow-up period of 5 years using 4 different outcome tools. We present 2 patients with large, calcified disc herniations at 2 levels in mid and lower thoracic spine treated endoscopically in local anesthesia. Clinical outcomes were analyzed using verbal numeric scale (VNS), Roland-Morris low back pain and disability questionnaire (RMQ), Oswestry Disability Index (ODI), and modified MacNab criteria at 6-, 12-, 24-, 60-month follow-up. After transforaminal endoscopic discectomy, both patients had significant postoperative reduction of back pain using VNS and significant outcome improvement using ODI, RMQ score, and modified MacNab criteria. These results did not change during all 4 follow-up periods. Transforaminal percutaneous full-endoscopic discectomy and hand reamers foraminotomy in local anesthesia is feasible and effective surgical technique for patients with large, calcified thoracic disc herniations at 2 levels even in long follow-up period of 5 years using 4 different outcome measuring tools. All 3 outcome measuring tools correlated well with pain reduction using VNS.
INTRODUCTION
A variety of surgical approaches have been described to reach herniated discs in thoracic spine [1]. Morbidities associated with these more or less aggressive surgical approaches led to the development of endoscopic techniques [1-5]. The goal was to achieve sufficient decompression without manipulating the spinal cord and to minimize surgical trauma and its consequences. Only 3 articles [4,6,7] in published literature address treatment of thoracic calcified disk herniations. None of them, however, reported outcome after surgical treatment of calcified disc herniations at 2 levels in the same patient. Here we present 2 patients with large, calcified thoracic disc herniations at 2 levels totally removed using transforaminal full-endoscopic approach with awakened patient in local anesthesia. Furthermore, none of published papers used 4 different measurement tools to report clinical outcome after endoscopic surgery in thoracic spine. This paper therefore is the first to address successful application of truly minimally invasive full-endoscopic transforaminal approach in local anesthesia for 2 level, large, calcified herniated thoracic discs with successful long follow-up period of 5 years using 4 different outcome measurement tools.
CASE REPORTS
1. First Illustrative Case
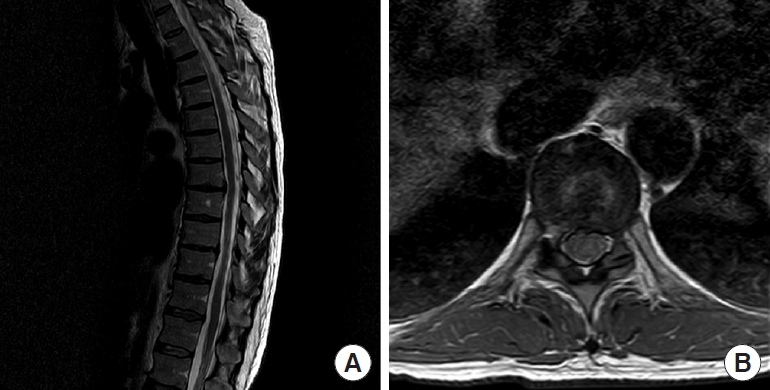
A 50-year-old male patient presented to our hospital with a history of severe thoracic back pain which lasted for more than 2 years. His neurological status was intact, but last couple of months his pain was significantly increasing. Magnetic resonance imaging (MRI) of the thoracic spine showed 2 calcified disc herniations; larger at Th6–7 level and smaller at Th7–8 disc level (Fig. 1A, B). Conservative treatment including physical therapy and pain killers was ineffective. In order to distinguish which disc herniation caused pain epidural steroid injections were performed at each level separately. Transforaminal epidural steroid injection at Th6–7 level decreased patient's pain only for 7 days. Transforaminal epidural steroid injection at lower level had no effect on patient’s pain so we concluded that only larger, cranial disc herniation at Th6–7 was clinically significant. Patient was instructed that the goal of surgery is to remove the larger disc herniation first and then, depending on postoperative pain, second disc herniation might be treated consequently in the second act.
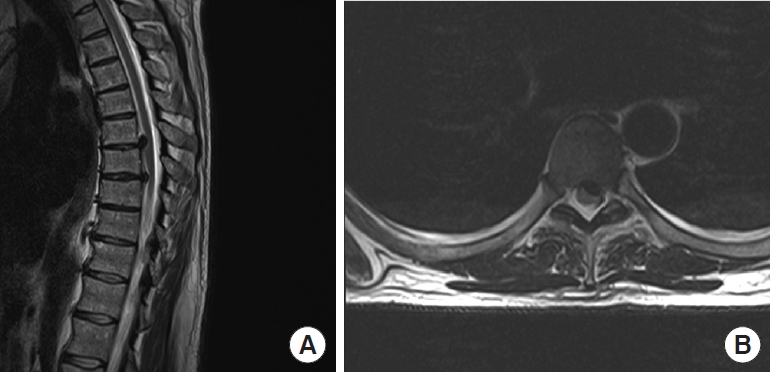
(A) Preoperative sagittal T2-weighed magnetic resonance imaging (T2W MRI) of thoracic spine of the first illustrative patient depicting 2 large calcified disc herniations: larger and cranially migrated at Th6–7 level and smaller at Th7–8 level. (B) Preoperative axial T2W MRI depicting calcified disc herniation at Th6–7 level.
2. Second Illustrative Case
A 59-year-old male patient presented to our hospital with prolonged gait disturbances, severe progressive paraparesis, paresthesias in lower limbs, and thoracic back pain radiating bilaterally between the ribs. He was not able to walk alone and was ambulatory only in a wheelchair. Initial computed tomography (CT) scan (Fig. 2A, B) showed 2 large calcified disc herniations causing significant spinal canal stenosis with consequent compression of the spinal cord. At Th7–8 level disc herniation was dorsomedial and at Th9–10 level disc herniation was dorsolateral on the left side. Thoracic MRI (Fig. 2C, D) confirmed the diagnosis.

(A) Preoperative sagittal computed tomography (CT) image of thoracic spine of the second illustrative patient depicting 2 large medial calcified disc herniations at Th7–8 and Th9–10 level. (B) Preoperative axial CT image of large medial calcified disc herniation at Th7–8 level causing absolute spinal canal stenosis and severe spinal cord compression. (C) Preoperative sagittal T2-weighed magnetic resonance imaging (T2W MRI) of thoracic spine, depicting same 2 large medial calcified disc herniations. (D) Preoperative axial T2W MRI of large medial calcified disc herniation at Th7–8 level causing absolute spinal canal stenosis and severe spinal cord compression.
Both patients were treated in local anesthesia using full-endoscopic transforaminal approach with blunt hand reamers for foraminotomy. In the first illustrative case only larger, clinically significant disc herniation at Th6–7 was treated surgically. For this patient, surgery lasted one and a half hour. In second illustrative case, both disc levels were treated at same time because patient manifested with sighs of myelopathy. This surgery lasted 2 and a half hours. The clinical outcome was evaluated using VNS, RMQ, ODI, and modified MacNab criteria in 4 follow-up periods. Both patients had significant postoperative reduction of back pain using VNS and significant outcome improvement using ODI, RMQ score, and modified MacNab criteria. All outcome tools correlated well with pain reduction using VNS in all follow-up periods. No evidence of increasing instability was found in postoperative imaging which makes this technique safe even for surgery at 2 levels. Satisfactory surgical decompression was achieved in both cases without any significant surgical morbidity. No surgery-related thoracic spine pain was observed immediately postoperatively or in the follow-up period.
Approval of hospital Ethics Committee was obtained for both patients and both patients signed an informed consent before surgery. Both patients were discharged home within 24 hours after the surgery without preoperative thoracic back pain. In the second illustrative patient symptoms of myelopathy vanished during first follow-up period.
SURGICAL TECHNIQUE
Surgical procedure was performed in local anesthesia with conscious sedation allowing continuous feedback from the patients. Patients underwent surgery in prone position with head turned to one side and hands resting above the head. Half an hour before the surgery patients intravenously received prophylactic antibiotic. For premedication patients received diazepam and bolus of 0.1 mg of Fentanyl. During surgery Fentanyl and Midazolam were applied in fractionated manner.
Using preoperative axial magnetic resonance images, a desired trajectory was planned and a place of skin incision was determined. Appropriate skin entry point was determined by drawing a line from posterior annulus at the medial pedicular line to lateral margin of facet joint (Fig. 3). One-centimeter long skin incision is usually placed between 5,5 cm and 6,5 cm from the midline at the side of the disc herniation or at the more painful side if the disc herniation was in the midline. The correct disc level was identified by counting the ribs first in caudal to cranial direction and then double checked by counting the ribs from cranial to caudal direction. This was done using metal rod as a marker on the skin. After skin incision, using lateral fluoroscopic view, a 20-G spinal needle was inserted into the skin and was targeted towards the desired intervertebral disc using transforaminal route. The tip of the needle was always directed towards the bone (superior articular process of lower vertebra and a rib head) as a safe zone. The approximate entry angle at the skin level depends on the patient constitution and is usually between 40° to 50° from the horizontal plane. Steeper angle should be avoided in order to avoid entering a pleural cavity. If pleural cavity is accidentally entered, surgery should be terminated and patient observed over couple of days. Since 20-G spinal needle is not very thick usually the pneumothorax is resolved spontaneously without suction tube or any surgical intervention.
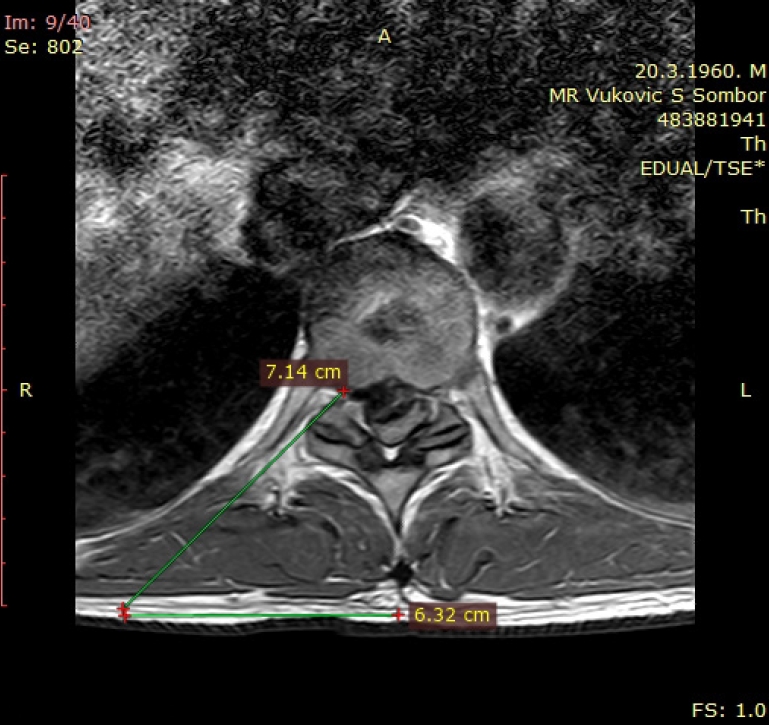
Determining skin entry point using preoperative axial T2-weighed magnetic resonance imaging. The line is drawn from posterior annulus at the medial pedicular line to lateral margin of facet joint. The distance from the mid line is 6.3 cm.
Once the bone is reached with the tip of the spinal needle the needle is slightly pulled backwards, redirected and then slide into neural foramen. After reaching the center of the disc, discography was performed using 1.5 mL of indigo carmine dye and Omnipaque 350 contrast (GE Healthcare, Chicago, IL, USA). Indigo carmine stains the degenerated acidic nucleus pulposus in blue and helps to identify herniated disc. Free fragments and calcified intervertebral disc tissue usually do not stain. Spinal needle is used only to perform the discography. The trajectory to the spinal canal established with the spinal needle is not the same and usually is not adequate as the trajectory needed for placement of the endoscope and working channel. In order to establish correct trajectory for the endoscope, surgeon needs to go through the top of the rib head and through the superior articular process of lower vertebra. Since the spinal needle is only 20 G it cannot be advanced through the bone. This can be done using cannulated TomShidi needle. This instrument is introduced percutaneously through the same skin incision and is targeted towards the desired foramen at the anterolateral border of superior articular process of the lower vertebra and over or through the rib head. Once in contact with the bone TomShidi needle is hammered through the bone in order to establish desired trajectory for working channel and endoscope. The inner part of TomShidi needle can be sharp or blunt. Sharp inlet is used first to help advance the instrument through the bone and once the tip of the instrument is in the spinal canal surgeon can switch to the blunt tip to avoid puncture of the dura or spinal cord injury. TomShidi needle cannot be percutaneously placed at the superior articular process of desired vertebra in a single step, rather couple of smaller maneuvers controlled by x-ray are necessary. When the tip of TomShidi needle reaches the dorsal border of the intervertebral disc, C-arm is rotated in anteroposterior view (Fig. 4A, B). In this view, the tip of the instrument should not under any circumstances stray far into spinal canal over the medial pedicle line. A 0.8-mm blunt tip guidewire was then introduced though TomShidi needle into the posterior part of the disc. Tapered, cannulated muscle dilatator was advanced over the guidewire until its tip reached lateral border of neural foramen. Foraminotomy was performed using hand, blunt tip, reamers sequentially starting from 4 to 8 mm (Fig. 4C). While advancing hand reamers one should take care that guidewire stays in place. During foraminotomy, only a small anterolateral portion of facet joint and cranial part or a rib head are removed. This maneuver does not affect spinal stability. After foraminotomy, a 25° angled, 4-mm endoscope was introduced through a working canula. Endoscope was positioned in the lateral epidural space so its tip was in the lower portion of neural foramen and was not passing over medial pedicle line (Fig. 4D). The inferior pedicle, calcified disc, epidural space, and exiting spinal nerve root were exposed. The first step in removing big dorsomedial calcified disc herniation is indirect decompression at the level of intervertebral disc space. This can be achieved with graspers for soft disc tissue but also with straight and angled electric burrs for bone removal. When a “bed” beneath the calcified portion of the disc is prepared one should detach herniated portion of the disc from the posterior longitudinal ligament at the level of endplate. In the final step surgeon carefully establishes the plane between free floating calcified portion of the disc and usually attached dura. Dissection plane is usually established from lateral to medial part of the disc and movements during dissection are carried out in cranio-caudal direction. Dissection is done using careful and slow movements with adjustable, curved, blunt tip probe and using so called “joystick” technique. Care must always be taken to avoid aggressive manipulation of the spinal cord to avoid further neurological deterioration and this is even more important in patients with myelopathy. All patients with myelopathy should preoperatively be informed about the possible but unlikely scenario of further neurological deterioration after surgery. After complete removal of all extruded calcified fragments from the spinal canal epidural space and spinal cord were adequately decompressed and we noticed pulsations of the dura. In some cases, when calcified portion of the disc cannot be safely detached from the dura, above mentioned “floating technique” is sufficient to resolve the compression to the spinal cord. In these cases, surgeon should not insist on complete disc removal in order to avoid further neurological deterioration. After thorough hemostasis, a guide wire was introduced once again in the intervertebral disc space. Spinal needle was then navigated to the disc over the guidewire and was used for postoperative epidural application of local anesthetic and corticosteroid mixture. Water pump was not used during surgery in order to avoid elevated pressure to the spinal cord. Instead, we used a free fall of the water with the water tank elevated between 50 cm to 1 m above the patient. The height of the water tank was manually adjusted for every patient and is mainly dependable on intraoperative bleeding. Postoperative MRI scans of first illustrative patients are shown in Fig. 5A and B, while postoperative MRI scans of the second patient are shown in Fig. 6A and B. In the first case cranial, clinically significant, disc herniation was removed completely. In the second case, both disc herniations were removed successfully. Preoperative and postoperative values of pain intensity using VNS, RMQ, ODI scores, and MacNab outcome criteria scores for both patients are shown in Table 1.
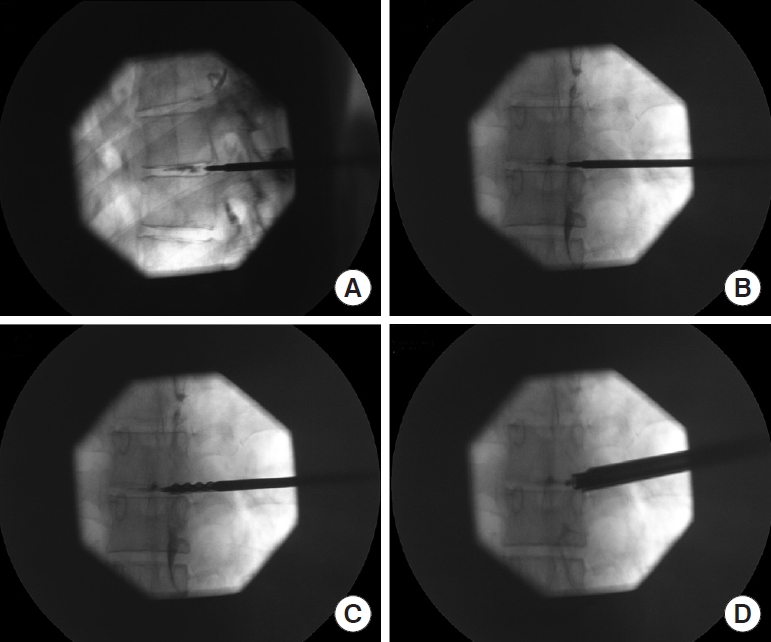
(A) Lateral intraoperative fluoroscopic view depicting position of TomShidi needle with the tip in the posterior part of annulus fibrosus of the desired intervertebral disc. The disc is stained with Omnipaque 350 contrast (GE Healthcare, Chicago, IL, USA). (B) Anteroposterior (AP) fluoroscopic view of the TomShidi needle at the same position showing the tip of the instrument in medial pedicular line. (C) Intraoperative fluoroscopic AP view showing final position of the first-hand reamer. The blunt tip of the instrument is just over the medial pedicular line while the sharp part of the instrument is at medial pedicular line. (D) Intraoperative fluoroscopic AP view showing position of the working channel, endoscope, and the probe in the neural foramen.
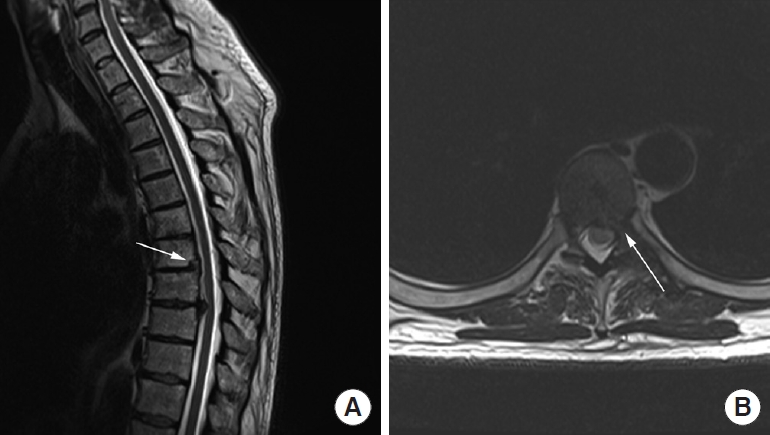
(A) Postoperative sagittal T2-weighed magnetic resonance imaging (T2W MRI) of thoracic spine of the first illustrative patient showing total removal of larger, cranial disc herniations at Th6–7 levels. White arrow depicts bone defect of the posterior vertebral body i.e., “bed” drilled beneath the disc for a removal of calcified portion of the extruded disc. (B) Postoperative axial T2W MRI of the same patient showing normal width of the spinal canal without disc herniation. White arrow depicts surgical trajectory i.e., transforaminal access to the spinal canal between the rib and a facet joint.
(A) Postoperative sagittal T2-weighed magnetic resonance imaging (T2W MRI) of thoracic spine of the second illustrative patient showing complete removal of both disc herniations at Th7–8 and Th9–10 levels. (B) Postoperative axial T2W MRI of the same patient showing normal width of the spinal canal without disc herniation at Th7–8 level.
DISCUSSION
Surgical treatment for thoracic disc herniation has evolved from open surgery to minimally invasive endoscopic techniques with the aim of reducing access-induced complications and improvement of surgical outcomes. In the paper of Gille et al. [6], authors described resection of the rib head and of the underlying vertebral pedicle together with the lateral part of the vertebral body to access the calcified disc herniation. In our opinion, this approach is too aggressive and the resection of pedicle is unnecessary if surgical trajectory is well planned preoperatively. This observation also corresponds to conclusion of other published paper [7]. Sparing the pedicle is even more important when operating on 2 adjacent disc levels. In the paper of Ruetten et al. [7], patients underwent endoscopic surgery in general anesthesia. In our opinion general anesthesia poses a higher risk for the spinal cord injury since surgeon is lacking real-time feedback from the awake patient. This fact is even more important for unexperienced surgeons who may not place trajectory well and may incidentally advance instruments too deeply/medially in the spinal canal.
The concept of the posterolateral transforaminal endoscopic approach was first developed as inside-out technique. In this paper, we present further development of this technique called outside-in technique first described by Hoogland [8]. There are several technique challenges for the transforaminal endoscopic procedure in the thoracic spine. First, safe and effective access to the disc is limited to a narrow bone channel between the facet joint and a rib head. Second, there is little working space. Third, creation of intradiscal working space is needed before intracanal calcified disc fragment extraction. The focus of this approach is to preserve the intact disc tissue and to remove only herniated soft or calcified portion of the disc from the spinal canal. During the procedure, we invaded only posterior one fifth of the disc and avoided invading deeper intradiscal space. Fourth, a herniated fragment is accessible only when the operating instrument is placed in the optimal trajectory. It is authors’ opinion that placement of right trajectory is the crucial step during the entire surgery. With optimal trajectory, even large, medial and calcified herniated discs in thoracic spine can be safely removed using this transforaminal approach. This technique leaves little possibility of injuring neural structures if TomShidi needle and working channel are not passed far over medial pedicle line and if surgery is performed with awakened patient in local anesthesia. The patient, in a continuous awakened state, is instructed to alert the surgeon if there should be any inadvertent physical trauma to the nervous structures.
The limitation to this method is the fact that the learning curve of this technique is rather long and it takes much time to achieve maximum level of efficacy. This is due to specific bone anatomy in thoracic spine and the vicinity of pleura and the lungs but also due to small number of patients with symptomatic thoracic disc herniations who require surgery. It is authors’ opinion that one should first be familiar with endoscopy at lumbar spine before thoracic spine can be successfully assessed. The development of full-endoscopic techniques, however, should not be evaluated as a replacement for existing standard operations but as a complementary procedure within the overall concept of spine surgery. Authors are aware that symptomatic thoracic disc herniations are extremely rare but significant clinical improvement of our patients in long follow-up period using 4 different outcome measurement tools indicate the need for controlled studies and larger samples to establish the efficacy of this technique.
CONCLUSION
Percutaneous full-endoscopic transforaminal discectomy, using blunt hand reamers for foraminotomy, is feasible and safe technique in treatment of calcified herniated discs in mid and lower thoracic spine. This surgical technique is recommended only to experienced surgeons with sufficient experience in endoscopy. Even large medial calcified disc herniations can be safely removed using this outside-in endoscopic technique which allow immediate verification of dura and nerve decompression.
Notes
The authors have nothing to disclose.

