Feasibility of the Far Lateral Suboccipital Approach to the Retroodontoid Region. How Much Bone Removal Is Truly Needed?
Article information
Abstract
Objective
The posterolateral extradural suboccipital approach can be used to reach the anterior epidural space and the retro-odontoid regions. The extent of necessary bone removal of the atlas vertebra (C1) has not yet been defined. We studied the changes in the size of the horizontal and vertical surgical windows using stepwise bone removal of C1. A representative case is shown.
Methods
The anatomical study was performed bilaterally on five Thiel-fixed human cadavers (mean age, 83.7 years). The surgical window (horizontal × vertical) required to access the retro-odontoid region via a posterolateral approach was measured for an intact C1 posterior arch, after a semicircular inferior partial resection of the C1 arch, after resection of the unilateral hemiarch of C1, and finally after drilling approximately 3 mm from the medial aspect of the lateral mass of C1.
Results
The intact C1 resulted in a very narrow surgical window of 6.3 mm × 9.7 mm (horizontal × vertical). The vertical window increased to a 13 mm after the semicircular inferior partial resection of the C1 arch and to 17.3 mm in the case of removal of the ipsilateral C1 posterior arch. The bone removal from the medial aspect of the C1 lateral mass resulted in a widening of the horizontal surgical window to 10.3 mm. The final size of the surgical window was 10.3 mm × 17.3 mm. The patient with severe kyphoscoliosis of the craniocervical spine was successfully operated on using odontoid and C1–2 facet osteotomies.
Conclusion
If only the anterior epidural space or the base of the odontoid needs to be reached, the semicircular inferior partial resection of the C1 arch allows for an adequate surgical window. The tip of the odontoid could only be reached if the ipsilateral posterior arch is resected.
INTRODUCTION
Different surgical exposures to the retroodontoid region exist. Anterior approaches include the transoral, high cervical retropharyngeal, or Whitesides approach. If an anterior approach is performed in the first stage, posterior instrumentation and fusion must be performed in a second surgery. Posterior approaches to the retroodontoid region include the posterolateral transcondylar approach, which results in a considerable amount of bone removal from the occipital condyle and the posterolateral extradural suboccipital approach. A midline posterior-only approach is less traumatizing for the patient in terms of soft-tissue dissection. Besides, the decompression, instrumentation, and fusion can be performed using the very same approach.
Modifications of the far lateral suboccipital approach to remove a retroodontoid pseudotumor [1], to achieve partial odontoidectomy [2], or to drain an atlantoaxial epidural abscess [3] have been reported. The authors of the studies as mentioned above report different amount of bone resection using their approaches.
The objective of the current study was to examine the changes in the size of the surgical window that would enable access to the retroodontoid region, depending on the amount of bone resection of the atlas vertebra (C1). The horizontal and vertical surgical windows leading to the retroodontoid region and the odontoid process were analyzed in intact spines and after sequential bone resection of C1 in 3 steps (Fig. 1).
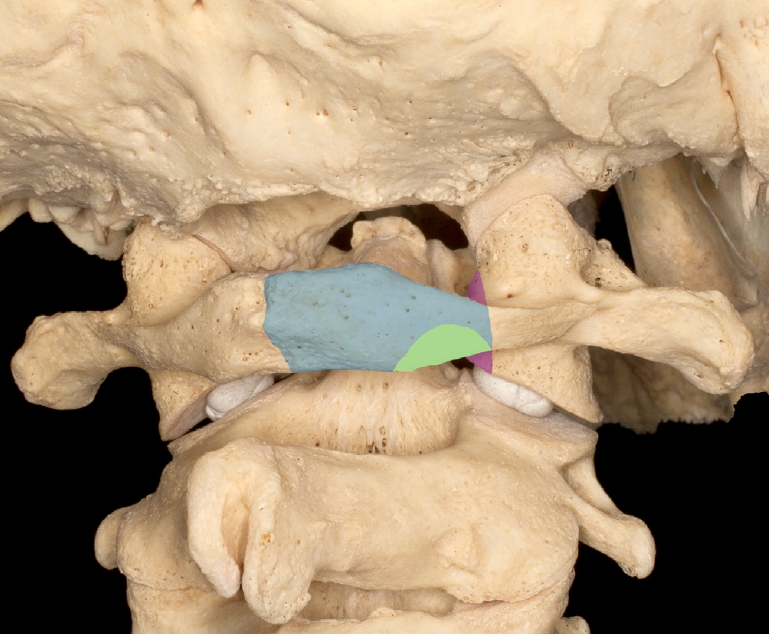
The 3 steps of C1 bone removal are shown on a macerated bone specimen. Type 1, no bone removal. Type 2, semicircular inferior partial resection of the C1 arch (colored green). Type 3, resection of the C1 posterior hemiarch (colored blue). Type 4, bone removal from the medial aspect of the C1 lateral mass (colored purple).
In the representative case, this approach was used to correct severe craniocervical kyphoscoliosis with a completely fused anterior column at the C1–2 level.
MATERIALS AND METHODS
1. Anatomical Study
For the anatomical, descriptive part of the study, a macerated bone specimen of the craniocervical junction was used. For the anatomical and experimental study, 5 Thiel-fixed human cadaveric specimens were used. The mean age of these specimens was 83.7 years, with a range of 74 to 94 years. The measurements were performed on both sides of the cadavers. The vertebral arteries were filled with colored silicon prior to dissection.
The dissections were performed with the cadavers in the prone position. The head was fixed with a modified Halo-fixation system with the cervical spine in the neutral position. The posterior aspect of the craniocervical junction was reached with a posterior midline incision and a posterolateral suboccipital approach with adequate soft tissue release to allow for medial angulation of the working channel. The occiput, posterior arch of the atlas (C1), lamina of the axis vertebra (C2) was dissected in a subperiosteal fashion. The V3v and V3h segments of the vertebral artery was prepared [4].
The C2 nerve root was identified and ligated lateral to its ganglion at the level of the C2 isthmus. It was used for gentle medial retraction of the dural sac to gain access to the epidural region in all specimens (Fig. 2A).
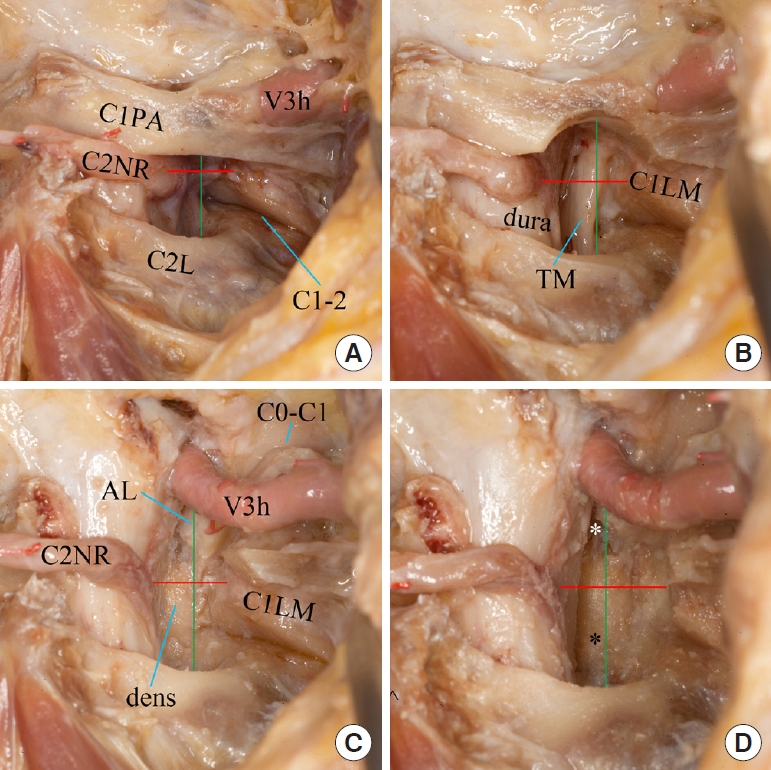
(A-D) Steps of C1 bone removal, right side. The red line marks the horizontal window, and the green line marks the vertical window. C1PA, C1 posterior arch; C2L, C2 lamina; C1LM, C1 lateral mass; AL, alar ligament; C2NR, C2 nerve root; TM, tectorial membrane; V3h, a horizontal segment of the vertebral artery. Visible joints: C0–C1, atlantooccipital joint; C1–C2, atlantoaxial joint. White asterisk marks the tip of the dens, the black asterisk its base.
With the intact C1, the window to the epidural region was limited medially by the dural sac, laterally by the lateral atlantoaxial joint, cranially by the C1 posterior arch, and inferiorly by the lamina of C2 (Fig. 2A). After measuring the horizontal and vertical limits of this surgical window, it was widened using sequential bone removal of C1, and the available surgical window was measured again.
First, a semicircular inferior partial resection of the C1 arch was created at the inferior aspect of the posterolateral part of the ipsilateral C1 posterior arch (Figs. 1, 2B) using a 5-mm diamond burr. The dimensions of the laminotomy were 10 mm horizontally, while its height was 3–4 mm according to the local anatomy. Second, the ipsilateral C1 posterior hemiarch was removed with a high-speed burr and a 2-mm Kerrison rongeur (Figs. 1, 2C). At this stage, the cranial margin of the surgical window was limited by the V3h segment of the vertebral artery, while the dimensions of the horizontal window did not change. Third, 3 mm of bone was removed from the medial aspect of the C1 lateral mass with a high-speed burr (Figs. 1, 2D). This resulted in a widening of the horizontal surgical window but did not change the limits of the vertical window. These 3 steps were performed first on the right side and then on the left side of the cadaver.
The thickness of the odontoid process was measured at its base as well as its height from its tip to its base. After opening the dura, the maximal thickness of the spinal cord in the coronal plane at the level of C1–2 was also measured.
All measurements were performed with an electronic caliper (Absolute System, Heidenheim, Germany). The anatomic dissections were carried out using loupe magnification (Zeiss, 3.4-fold magnification). Detailed photo documentation was carried out using a Canon 5-dimensional digital camera.
2. Surgical Case and Clinical Application of the far Lateral Approach
The surgical approach and technique of anterior column and odontoid osteotomy using a midline incision and far lateral approach was explored in a 34-year-old patient with ankylosing spondylitis. The patient presented with disabling loss of function and visual axis due to a severe global deformity related to fixed cervicothoracic and craniocervical kyphoscoliosis as well as lumbar kyphosis with severe global coronal and sagittal imbalance. The representative case was operated by the senior author (HK).
RESULTS
1. Relevant Bony and Neural Anatomy of C1–2
The atlantoaxial region showed great bony variations. The distance between the C1 posterior arch and the C2 lamina was variable and depended on the position of the head, increasing on flexion of the upper cervical spine.
When the axis vertebra was viewed laterally, it was apparent that the superior border of the lamina of the axis, the superior limit of the pars interarticularis, and the base of the odontoid were located on a rising slope, the base of the odontoid being most cranial. For this reason, entering the spinal canal just above the lamina of the axis in a horizontal line lead us to the upper part of the C2 vertebral body, while the base of the odontoid was located more cranially and was covered by the posterior arch of the atlas.
The thickness of the odontoid at its base measured 10.8 ± 1.4 mm, while the odontoid height measured 14.4 ± 1.0 mm. The maximal thickness of the spinal cord at the C1–2 level was 10.7 ± 0.3 mm.
2. Sequential C1 Bone Resection
To classify the different steps of the C1 bone resection, the sequential process is differentiated into types 1 to 4.
1) Type 1 – no bone removal
The surgical window was limited in the frontal plane medially by the dura and laterally by the C1–2 joint. In the craniocephalad direction, the surgical window was limited by the C2 lamina caudally and the posterior arch of the atlas cranially.
The intact configuration without bone resection resulted in a limited surgical window, which allowed for limited access to the anterior epidural space up to the base of the odontoid. The window measured 6.3 ± 2.1 mm×9.7±1.5 mm (horizontal×vertical).
2) Type 2 – semicircular inferior partial resection of the C1 arch
The semicircular inferior partial resection of the C1 arch was centered above the surgical window and was 10 mm wide and 3–4 mm high.
The horizontal surgical window did not change; it was still limited medially by the dura and laterally by the C1–2 joint. The vertical limits were formed caudally by the C2 lamina and cranially by the C1 posterior arch at the site of the C1 laminotomy defect.
The laminotomy allowed access to the anterior epidural space up to the base of the odontoid. The window measured 6.3 ± 2.1 mm × 13.0 ± 1.2 mm (horizontal × vertical).
3) Type 3 – ipsilateral removal of the C1 posterior arch
The removal of the ipsilateral C1 posterior arch between its posterior tubercle and its base laterally considerably widened the vertical part of the surgical window while leaving the horizontal part of the surgical window unchanged. The vertical limits of the surgical window were formed caudally by the C2 lamina and cranially by the V3h segment of the vertebral artery.
This extension of the vertical surgical window allowed access to the odontoid up to its tip. The window measured 6.3 ± 2.1 mm × 17.3 ± 1.1 mm (horizontal × vertical).
4) Type 4 – partial removal of the C1 lateral mass
Bone removal from the medial aspect of the C1 lateral mass resulted in a widening of the horizontal surgical window while leaving the vertical limits unchanged. The increased space was proportional to the amount of C1 bone removed. We drilled approximately 3 mm off the medial aspect of the C1 lateral mass. The horizontal limits of the surgical window were then formed by the dura medially and the C1–2 joint with a thinned C1 lateral mass laterally.
This allowed access to the anterior epidural space and the odontoid from its base to its tip and its ipsilateral side. The medial aspect of the lateral mass, as well as the distance between the odontoid and the lateral mass could then be reached.
The final size of the surgical window measured 10.3 ± 0.5 mm × 17.3 ± 1.1 mm (horizontal× vertical window).
3. Surgical Case Example
The 34-year-old ankylosing spondylitis patient sought treatment for a severe global deformity with loss of visual axis, difficulty with oral intake, and with walking unless in a ski-jumpers position, which balanced his tendency to fall forwards with his arms lifted posteriorly.
Following extended imaging diagnostics, an anaesthesiologic feasibility study of transnasal intubation was performed in the intensive care unit with the patient sedated. Given the complex deformity affecting the patient from head to the pelvis, the family agreed for a multistaged correction strategy to improve the debilitating deformity, which had ensued over more than 10 years (Fig. 3A).
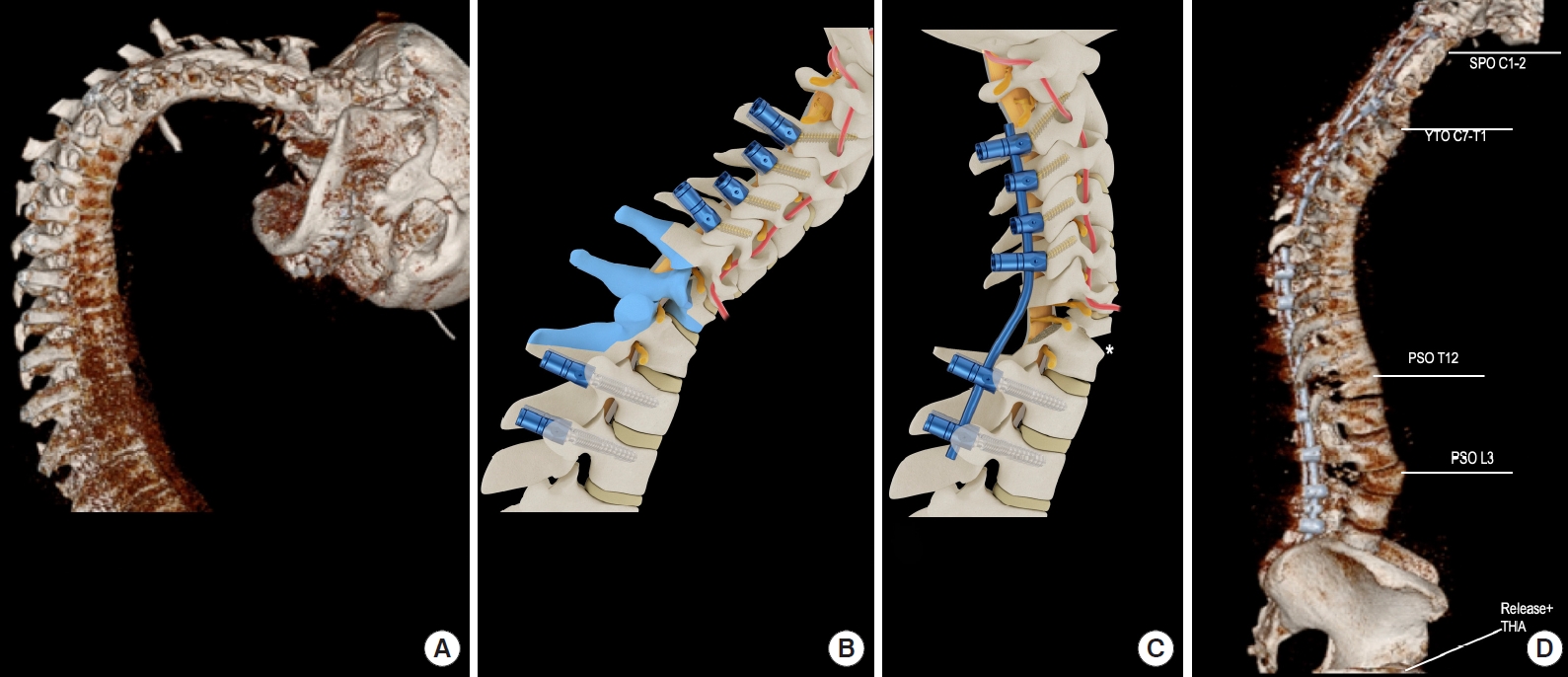
Clinical case example of applying a far lateral approach. A 34-year-old ankylosing spondylitis patient presented with a severe disabling deformity. (A) The patient displayed global sagittal and coronal deformity with chin-on-chest deformity. (B+C) The first treatment was with an open-closing-wedge osteotomy of C7–T1. Subsequently, dual lumbar and thoracic pedicle subtraction osteotomy (PSO) was performed at T12 and L3. This was followed by craniocervical osteotomy using an Smith-Petersen osteotomy like mechanism for correction. Panel D shows postoperative imaging after all osteotomies had been performed. Finally, the patient underwent hip joint release and total hip arthroplasty for arthritic hip flexion-contracture of the right hip joint.
In the first surgery, the patient underwent successful closingopening wedge osteotomy at C7–T1, the so-called Y-osteotomy (YTO; Fig. B3, C3), according to Koller et al. [5]. A sitting position was necessary given the chin-to-pelvic global posture of the patient, which prohibited prone positioning by buttressing the patient’s weight at the sternum and the pubis. Intraoperative use of an image intensifier was not possible given the severe craniocervico-thoracic deformity and the patient’s need to be in a sitting position. To facilitate osteotomy closure and track the correction, a temporary malleable rod and an overhead customized Crutchfield system were applied to the head. Osteotomy closure was advanced until intraoperative neuromonitoring indicated irritation of the left C8 nerve root. After osteotomy closure, a 4-rod cervicothoracic construct was established, and cervicothoracic fusion was achieved by bone-on-bone closure mediated by an asymmetric YTO-correction mechanism (Fig. 3C*). Blood loss was 650 mL.
After an uneventful postoperative course and timely recovery within 2 weeks, the patient underwent dual pedicle subtraction osteotomy (PSO) of T12 and L3 and thoracolumbosacral fusion using a 4-rod construct (Fig. 3D). Blood loss was 1,600 mL.
The residual head tilt (Figs. 4A-C, 5B) was addressed using a posterolateral far lateral approach via a midsagittal incision. A C1–2 osteotomy of the anterior fused column, including the facets and odontoid (Fig. 4) was conducted using a type 3 bilateral surgical window as described above. The atlantoaxial membrane was opened medially and mobilized laterally to control the C1–2 venous plexus. The C2 nerve root was dissected, ligated just proximal to its ganglion. The ganglion was coagulated with bipolar forceps and transected. An epiperiostal approach to the anterior ossified C1–2 fusion mass was obtained. The anterior bloc was osteotomized using an ultrasound burr and ultrasound blade with the protection of the vertebral arteries laterally and cranially. The dural sac was protected and retracted medially using a Watson-Jones dissector.
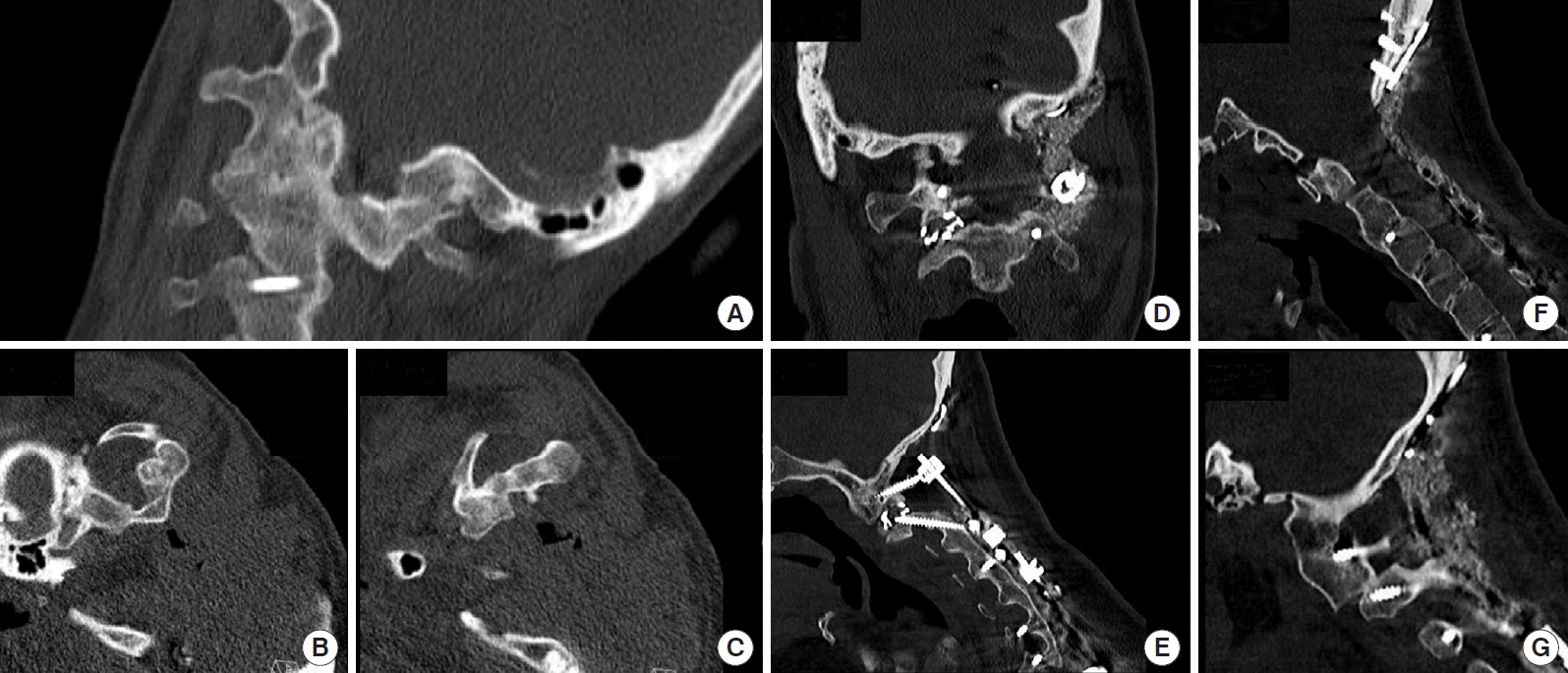
(A-C) The AS-patient also presented with fixed rotational kyphoscoliosis of the craniocervical junction. The anterior column between C0 and C2 was completely fused. (F) The patient underwent anterior column osteotomy via a posterior midline incision using the far lateral approach. To address craniocervical malalignment with severe head rotation to the left and head obliquity to the right, a titanium cervical cage was inserted between the C1–2 joints (D+E), and bone-on-bone contact was intended on the left side (G). (D) A large fusion mass using local bone and allograft material was applied at the craniocervical transition zone.
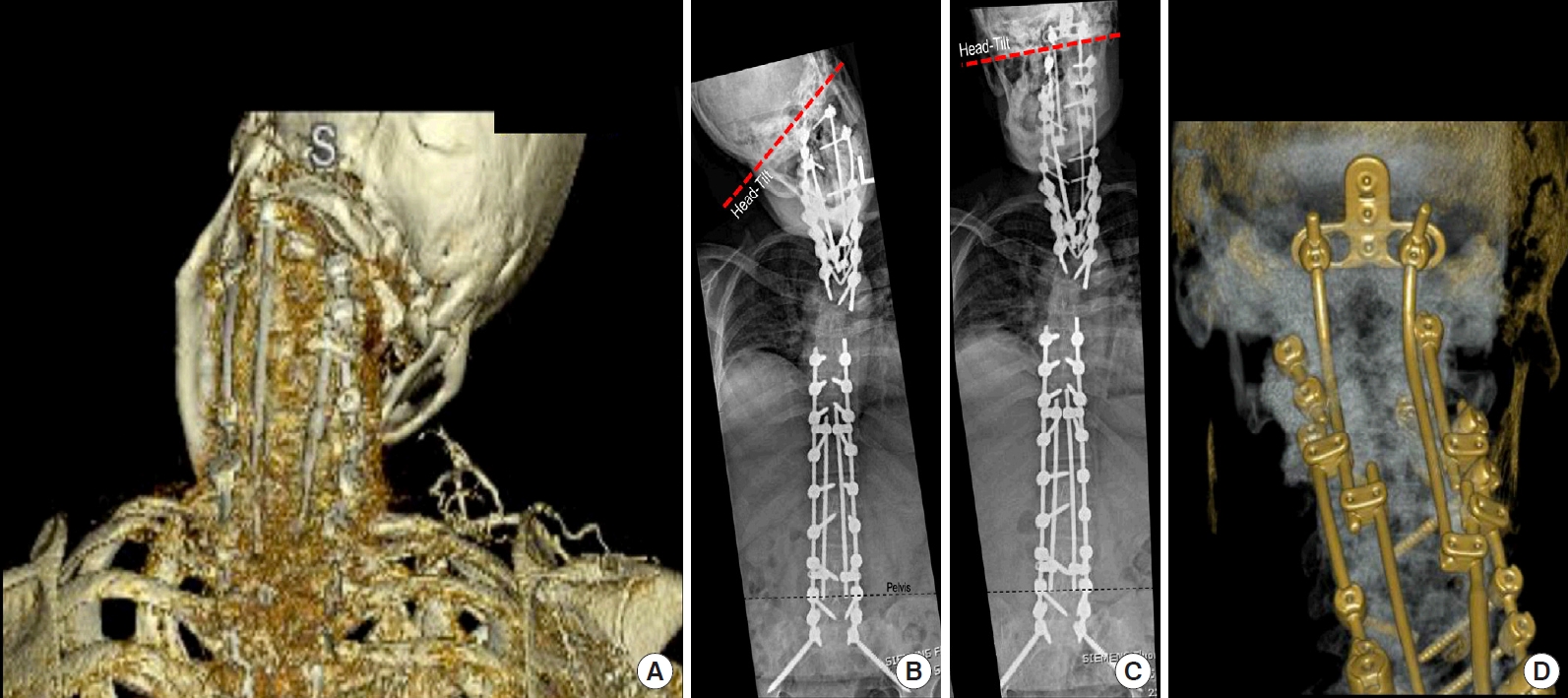
Panels A and B show preoperative 3-dimensional scan and full-spine standing radiographs after cervicothoracic asymmetric Y-Type osteotomy and before the C1–2 osteotomy. Note the head rotation and head tilt. Panels C and D show postoperative radiographs and reconstructed computed tomography scans after craniocervical correction using the far lateral approach. A 4-rod construct bridges the connection in the cervical spine towards the thoracic spine and from the thoracic to the lumbar spine, crossing two three-column osteotomies. A 2-rod connection was established between the occiput and cervical construct by a construct-to-construct assembly of 4.0-mm titanium rods.
Before osteotomy conduction, screw hole preparation was performed using a 2.4-mm drill. However, insertion of shank shaft screws into C1 was accomplished only after dissection towards the anterior epidural space, and left side osteotomy of C1–2 was achieved.
In a left-to-right side fashion, the stability of the C0–C2 junction was continuously maintained using temporary 3.5-mm titanium rods.
After completing of the osteotomy, the osteotomy gap on the right side was distracted using an arthrodesis spreader, and a 16 × 12-mm solid titanium intervertebral cervical cage was impacted between the curetted facets of C1–2. The cage was filled with local autograft bone. On the contralateral (left) side, the articular surfaces of C1 and C2 were smoothed with a chisel, curetted using the ultrasound burr, and then approximated using compression techniques mediated by screw-rod manoeuvres. The correction was also tracked by fixing the head in a Mayfield-head holder with all hinges partially released during the correction process to enable manual correction both with axial rotation and coronal tilt reduction by 1 of the 2 surgeons. After gross head correction, the Mayfield-head holder was locked again, and fine adjustments were performed using screw-rod maneuvers in a construct-to-construct fashion (craniocervical to subaxial cervical construct connection, Fig. 5D) to complete the correction process. With the cage in the right C1–2 joint acting as a hinge, an asymmetric correction mechanism was possible to correct the severe head tilt and axial rotation and reduce the kyphosis of C0–C2. The correction mechanism was similar to that of asymmetrical open-wedge osteotomies and Smith-Petersen osteotomy, respectively. A large amount of local autograft was mixed with allograft bone material to achieve a high-volume fusion mass at C0–C2 (Fig. 4D). Blood loss was 300 mL. The postoperative course was accompanied by prolonged dysphagia and dizziness reported by the patient for 1 week and subsided with medical treatment. After otolaryngeal and surgical causes were ruled out, the symptoms were assumed to be related to the acute and drastic correction of both head tilt in the coronal plane and axial head malrotation. Both might have challenged his cortical balance system in the first postoperative days (Fig. 5C).
Finally, the patient underwent hip joint release and total hip arthroplasty for femoroacetabular osteoarthritis and hip joint contracture on the right side. He experienced an uneventful postoperative course. One year after the surgical series, the patient is independently mobilized and lives with his very grateful family.
DISCUSSION
To the best of our knowledge, this is the first study to analyze the different magnitudes of C1 bony resections and their related surgical window dimensions to reach the retroodontoid region with a far lateral surgical approach via a midline posterior incision. The novel data were very helpful for planning and successfully performing an open-wedge osteotomy of both the odontoid and the fused facets in patients with severe fixed kyphoscoliosis.
The largest series reporting on the transoccipitocervical posterolateral approach with decompression of the neural structures in case of anterior lesions at C0–C2 included 23 patients [6]. In these cases, the bony decompression included expansion of the foramen magnum and resection of the posterior arch of the atlas, the posterior part of the C1 lateral mass, the posterior part of the odontoid and the posterosuperior part of the C2 vertebral body. This resulted in anteroposterior decompression of the medulla and spinal cord followed by craniocervical fusion.
In the following years, modifications of this approach were reported to remove a retroodontoid pseudotumor after complete resection of the C1 posterior arch with a transdural approach preserving the arachnoid [1]. Later, odontoidectomy with the use of a posterior tubular retractor system and bone resection of the C1–2 lateral masses and the C2 pars interarticularis in 4 cadavers as well as clinical application in 2 clinical cases was reported by Archavlis et al. [2]. A similar approach was used to treat a high cervical abscess by Riley et al. [3]. In that specific case, the medial aspect of the C1–2 joint and the C1 inferior laminar edge was resected using a bone shaver by 2–3 mm, and 3 mm of the C1 lateral mass was removed through a 14-mm tubular retractor system to reach the C1–2 epidural space and the odontoid. To gain access to the anterior epidural space at C1–2, the upper cervical spine was flexed with the patient in the prone position. The head was tilted and rotated to the contralateral side to increase the C1–2 interlaminar space.
In our anatomic feasibility study, the position of the head was neutral, which allowed for standardization of the measurements. Additionally, in our opinion, the rotation of the atlantoaxial joint, which leads to changes in the relation of the vertebral artery and the related bony structures, makes intraoperative protection of vascular and neural structures more demanding. Changes in the position of C1 relative to C2 are not effective in patients with rigid craniocervical deformities, as shown in our case.
Likewise, to our knowledge, the present study was the first to report osteotomy of the odontoid and anterior column of C1–2 mediated by a posterolateral suboccipital approach using a midline incision. A transoral approach and anterior release of the C1–2 structures was not possible in our case given the severe flexion deformity with the rigid chin-on-chest position of the head. Additionally, this procedure was not considered, as control of the dural sac and avoidance of infection was judged to be better with the postero-lateral approach to the retroodontoid region and to perform the osteotomy.
According to our results, 3 forms of bone removal can be chosen according to the goal of the surgery. The semicircular inferior partial resection of the C1 arch should be tailored according to the anatomical variations of the C1 posterior arch. It allows for the opening of the anterior epidural space and reaching the base of the odontoid. Maintaining a bony rim cranially below the vertebral artery facilitates protection of the vertebral artery during working anterior to the dural sac and in the retroodontoid region. If complete resection of the odontoid is planned, the unilateral C1 posterior arch should be resected to allow for a greater vertical surgical window and to reach the tip of the odontoid. In such a clinical situation, the vertical window is limited cranially by the horizontal part of the vertebral artery (V3v-segment). The horizontal window could be increased by resecting the medial aspect of the C1 lateral mass. This could also be helpful if the goal of the surgery is to resect the odontoid, as the mean maximal width of the odontoid is 11 mm in the coronal and sagittal planes [7]. According to our present results, the height of the odontoid was 14.4 ± 1.0 mm. While the horizontal window with intact bony surroundings is only 6 mm, it can be increased to 10 mm after resectioning of the medial part of the C1 lateral mass. Otherwise, achieving an area for odontoid resection can be a demanding or impossible procedure using the posterior midline incision and far lateral approach.
Reaching the odontoid and freeing it of soft tissues will result in injury to the main stabilizers of the upper cervical spine, the tectorial membrane, the craniocervical Y-ligament [8], the transverse ligament, and the alar ligaments. This could lead to craniocervical and atlantoaxial instability, necessitating C0–C2 or C1–2 fusion. Notably, posterior fusion could be performed using the same posterior approach.
In the long-term course, the need for combined spinal deformity treatment of both thoracolumbar and cervicothoracic kyphosis can lead to up to 30% of ankylosing spondylitis patients requiring spinal deformity surgery [5]. However, descriptions of multistage surgical correction in patients with severe deformities, including those of the craniocervical junction, the cervicothoracic region, and the thoracolumbar spine, are scant. Chien [9] reported on a patient who had both C7 PSO for chin-on-chest deformity and staged C1–2 facet joint release in addition to correction of malrotation and C1–2 flexion deformity with stenosis. Anterior column C1–2 osteotomy was not indicated. Kim et al. [10] reported a case of severe global deformity with chin-on-pubis deformity. A multistaged correction was performed with PSO of C6, posterior vertebral column resection of T11–12, PSO of L3, and bilateral total hip arthroplasty. Craniocervical correction was not necessary. The author of the current case preferred YTO to PSO at C7-T1, given the ability for a larger correction and application of an asymmetric correction mechanism with YTO to address the flexion deformity, the frontal plane head tilt, and scoliosis as well as the rotational deformity. Asymmetric PSO, a closing-wedge osteotomy, is limited due to the geometry of the correction and the limited vertebral height of C7 or T1. [5]. A vertebral column resection at C7 or T1 increases the magnitude of destabilization, which is more difficult to control with the patient in the sitting position and, thus, was not selected in that specific case.
CONCLUSION
Sequential bone resection of C1 enlarges the surgical window, increasing from 6 mm × 10 mm (intact C1) to 10 mm × 17 mm (maximum resection). Using a semicircular inferior partial resection of the C1 arch, the anterior epidural space and the base of the odontoid could be reached. The tip of the odontoid could only be reached if the unilateral C1 posterior arch was resected. In case of iatrogenic injury to the stabilizing ligaments of the craniocervical junction and upper cervical spine, fusion should be performed. It can be achieved using the same approach used for the retroodontoid region.
Successful application of the far lateral suboccipital approach and utilization of a type 3 window in a patient with severe craniocervical kyphosis showed that the anatomical nuances of the far lateral approach have clinical significance and might aid in comparisons of different techniques and results in the future.
Notes
The authors have nothing to disclose.
