Preoperative Neck Disability Severity Limits Extent of Postoperative Improvement Following Cervical Spine Procedures
Article information
Abstract
Objective
Our study aims to evaluate the impact of severity of preoperative Neck Disability Index (NDI) on postoperative patient-reported outcome measures (PROMs).
Methods
A retrospective review of primary, elective, single or multilevel anterior cervical discectomy and fusion or cervical disc arthroplasty procedures between 2013 and 2019 was performed. Visual analogue scale (VAS) neck and arm, NDI, 12-item Short Form physical and mental composite score (SF-12 PCS and MCS), Patient-Reported Outcome Measurement Information System physical function, and 9-item Patient Health Questionnaire (PHQ-9) were collected preoperatively and postoperatively. Patients were categorized by preoperative NDI: none-to-mild disability (< 30); moderate disability (≥ 30 to < 50); severe disability (≥ 50 to < 70); complete disability (≥ 70). The impact of preoperative NDI on PROM scores and minimum clinically important difference (MCID) achievement rates were evaluated.
Results
The cohort included 74 patients with none-to-mild disability, 95 moderate, 76 severe, and 17 with complete disability. Patients with greater preoperative disability demonstrated significantly different scores for NDI, VAS neck, SF-12 MCS, and PHQ-9 at all timepoints (p < 0.001). Patients with more severe disability demonstrated different magnitudes of improvement for NDI (all p < 0.001), VAS neck (p ≤ 0.009), VAS arm (p = 0.025), and PHQ-9 (p ≤ 0.011). The effect of preoperative severity on MCID achievement was demonstrated for NDI and for PHQ-9 (p ≤ 0.007).
Conclusion
Patients with severe neck disability demonstrated differences in pain, disability, physical and mental health. MCID achievement also differed by preoperative symptoms severity. Patients with more severe neck disability may be limited to the degree of improvement in quality of life but perceive them as significant changes.
INTRODUCTION
Degenerative cervical myelopathy is one of the leading causes of spinal cord dysfunction worldwide with areas such as North America recording a prevalence of around 605 individuals per million [1]. Arising due to the compression of the spinal cord, myelopathy is characterized by weakness, loss of manual dexterity, gait dysfunction, and extensive disability [2]. Due to such adverse effects on an individual’s physical and mental health, the number of patients electing to receive surgeries such as anterior cervical discectomy and fusion (ACDF) and cervical disc arthroplasty (CDA), rather than relying on conservative treatments for relief, is steadily rising.
Myelopathy has been cited as a major cause of disability, leading clinicians to place greater importance on following patients’ functional and mental statuses preoperatively and postoperatively. These are measured using patient-reported outcome measures (PROMs) such as the Neck Disability Index (NDI), Japanese Orthopaedic Association scores (JOA), and modified JOA (mJOA). The NDI, specifically, contains 10 domains about daily life that quantify the level of disability present in those with neck pain [3]. NDI scores have been found to significantly improve following cervical spine surgery in myelopathy patients as well as to correlate with other quality of life measures [4-8].
Although studies have considered postoperative improvements from baseline, the question of whether the extent of preoperative disability modulates postoperative recovery still exists. A past study reported that while a majority of those with severe or progressive myelopathy improve following surgery, there may be 15%–30% who do not experience recovery [9,10]. With varying outcomes, it is vital to consider postoperative improvement in the context of preoperative symptom severity. Prior analyses have established that preoperative disability may be a predictor for postoperative outcomes in myelopathy patients by using the JOA and mJOA [11,12]. Goh et al. [13] further stratified severity by JOA scores to demonstrate that severe preoperative myelopathy patients reported greater postoperative improvement and ability to attain a minimum clinically important difference (MCID) in functional and mental health outcomes following surgery. Though not categorized by severity, there has been a report of higher baseline JOA scores significantly reducing the odds of achieving MCID in myelopathy patients as well [14]. Although a few of these studies evaluate severity, they have not considered this topic or its implications on the attainment of a clinically perceivable difference in symptoms through the NDI measure. Although this measure was originally validated in the outpatient setting [15], its use in spine surgery is pervasive across the globe and previous studies have established both its reliability and appropriateness among patients with cervical myelopathy [5,16,17].
Currently, there is controversy surrounding whether surgery is the best and most efficacious option for severe myelopathy patients, as some report the existence of residual disability postoperatively, while others find only substantial improvements [7,18,19]. Our study may shed more light on this conversation through analysis of a widely utilized PROM that captures disability severity. With this information, physicians may reference a larger variety of PROMs to screen for the distinct preoperative symptoms caused by cervical myelopathy. In doing so, spine surgeons may preemptively account for the extent of an individual’s disease manifestation and possibly predict their potential to obtain optimal outcomes following elective cervical procedures. Therefore, our aim is to evaluate the impact of the severity of preoperative NDI on postoperative PROMs.
MATERIALS AND METHODS
1. Study Design
A retrospective review of a prospectively maintained single-surgeon surgical database was performed to identify patients who underwent a cervical spine procedure between December 2013 and December 2019. Inclusion criteria were set as patients who underwent a primary, elective, single or multilevel ACDF or CDA. Exclusion criteria were set as revision procedures or procedures indicated for trauma, infection, or malignancy. Additionally, patients missing a preoperative NDI score were excluded. All procedures were performed at a single institution and both approval by the Institutional Review Board of Rush University Medical Center (ORA #14051301) and patient informed consent were obtained prior to the commencement of this study.
2. Data Collection
The surgical database used for this study contained information for each patient regarding demographics, perioperative characteristics, complications and PROMs. Demographic information was collected for age, body mass index (BMI), reported gender, ethnicity, diabetic and smoker status, and insurance collected. Patient fitness for surgery was evaluated using the American Society of Anesthesiologist physical status classification and comorbidity burden was scored as the Charlson Comorbidity Index. Perioperative characteristics were defined as the associated spinal pathology, number of operative levels, operative duration (skin incision to closure), estimated intraoperative blood loss (EBL), postoperative length of hospital stay (LOS), and day of discharge.
PROMs were collected as NDI, visual analogue scale (VAS) for neck and arm pain, Patient-Reported Outcome Measurement Information System physical function (PROMIS PF), 12-item Short Form physical composite score (SF-12 PCS) for physical health, and both 9-item Patient Health Questionnaire (PHQ-9) and SF-12 mental composite score (MCS) for mental health. All PROMs were collected preoperatively and at 6 weeks, 12 weeks, 6 months, and 1 year postoperatively. Assessment of significant improvements as perceived by the patient was collected through MCID achievement by comparing the improvement from preoperative to postoperative scores (Delta) with established thresholds from the literature: 2.6 (VAS neck) [20]; 4.1 (VAS arm) [20]; 17.3 (NDI) [20]; 8.1 (SF-12 PCS) [20]; 4.7 (SF-12 MCS) [20]; 4.5 (PROMIS PF) [21]; 3.0 (PHQ-9) [22].
3. Severity of Disability
Preoperative disability was evaluated using the NDI, which is a self-reported questionnaire adapted from the Oswestry Disability Index. The questionnaire consists of 10 equally weighted domains that are scored from 0–5. The total score is multiplied by 2 and divided by 100 to reach a final score with larger scores indicating worse disability and a score of 0 indicating absent disability. To further assess the severity of disability, the NDI score was categorized into 5 separate groups based on the score: none-to-mild disability (NDI< 30); moderate (30≤ NDI< 50); moderately severe disability (50≤ NDI< 70); complete disability (70≤ NDI).
4. Statistical Analysis
The study cohort was evaluated for differences in baseline demographics and perioperative characteristics between severity groups using either chi-square analysis for categorical variables or an unpaired t-test for continuous variables. Differences in mean absolute postoperative PROM scores and magnitude of postoperative improvement between NDI severity groups was evaluated using a 1-way analysis of variance and post hoc Tukey test. The impact of preoperative NDI severity on PROM scores was assessed using a multiple linear regression to account for radiculopathy (VAS arm and VAS neck) and any significant baseline characteristics. Similarly, the impact of preoperative NDI severity on rates of MCID achievement was evaluated using a simple logistic regression and a multiple logistic regression to account for radiculopathy. To control for False Discovery Rates, a Benjamini Hochberg correction was applied and an alpha value was set to 0.05.
RESULTS
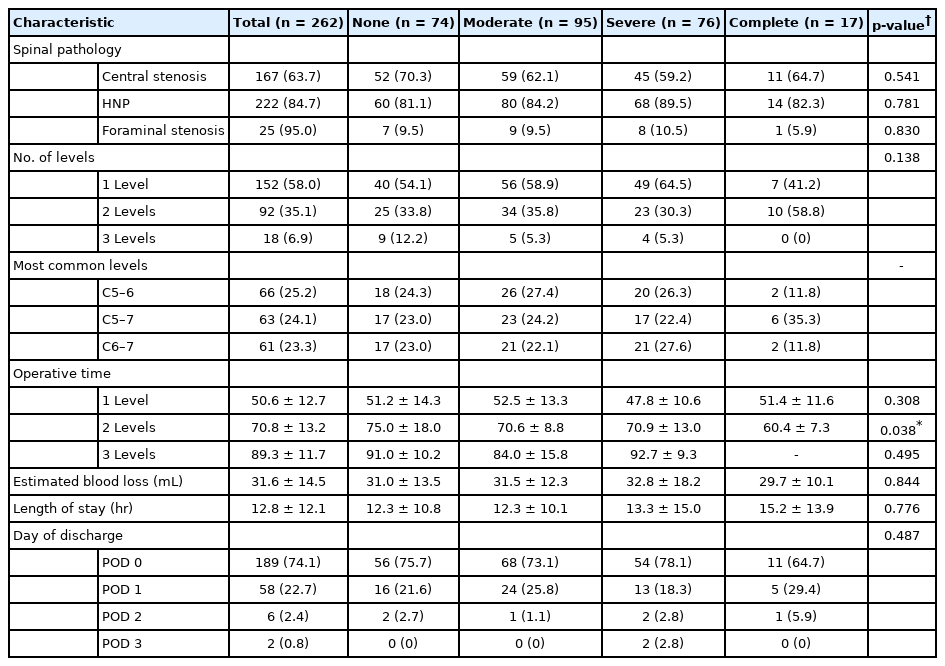
Following the application of inclusion and exclusion criteria, a total of 262 patients were included in the study cohort, of whom 74 had none-to-mild disability, 95 moderate, 76 severe, and 17 with complete disability. Mean age was 49.3 years with 62.6% being male and having an average BMI of 29.4 kg/m2. Except for smoker status and insurance collected (both p ≤ 0.29), there were no significant differences in baseline characteristics between all groups (Table 1).
Perioperative characteristics are detailed in Table 2. Majority of patients had a preoperative spinal pathology of herniated nucleus pulposus, which was similar across all groups (p = 0.781), with most operations conducted at the single level (58.5%, p = 0.205). Similar EBL, LOS, and day of discharge were demonstrated for all groups, but the operative duration was significantly shorter in the severe group as compared to the none-to-mild group (53.8 ± 21.3 minutes vs. 63.1 ± 21.6 minutes, p = 0.028).
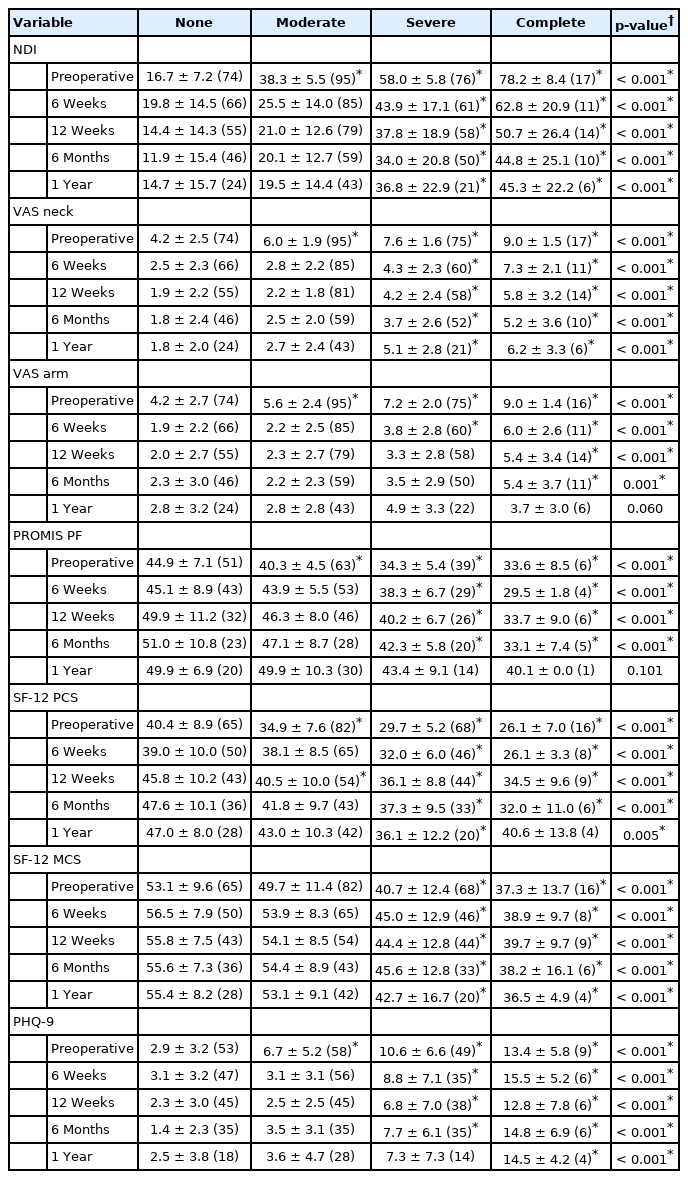
Comparisons of PROMs between neck disability severity groups is detailed in Table 3. At the preoperative timepoint, mean NDI demonstrated significantly higher values for moderate, severe, and complete disability groups as compared to the none-to-mild group (p < 0.001). A significantly higher disability remained for both the severe and complete disability groups as compared to the none-to-mild group for all postoperative timepoints (p < 0.001, all). The moderate, severe, and complete disability groups demonstrated significantly worse values for VAS neck, VAS arm, PROMIS PF, SF-12 PCS, and PHQ-9 as compared to the none-to-mild group at the preoperative timepoint, whereas, only the severe and complete disability groups demonstrated significantly worse scores for SF-12 MCS (p < 0.001, all). Postoperatively, VAS neck and SF-12 MCS demonstrated significantly worse scores among the severe and complete disability groups compared to the none-to-mild group at 6 weeks through 1 year and 6 weeks through 6 months for PROMIS PF (p < 0.001, all). VAS arm scores were significantly worse for the severe disability group at the 6-week timepoint only and for the complete group from 6 weeks through 6 months (p < 0.001, all). SF-12 PCS scores were significantly worse than the none-to-mild group for patients categorized with complete disability from 6 weeks through 6 months, severe disability at all postoperative timepoints, and for moderate disability at 12 weeks only (p < 0.001, all). Lastly, mean PHQ-9 values were significantly worse for the severe-to-complete disability group at all postoperative timepoints and from 6 weeks through 6 months for the severe group (p < 0.001, all).
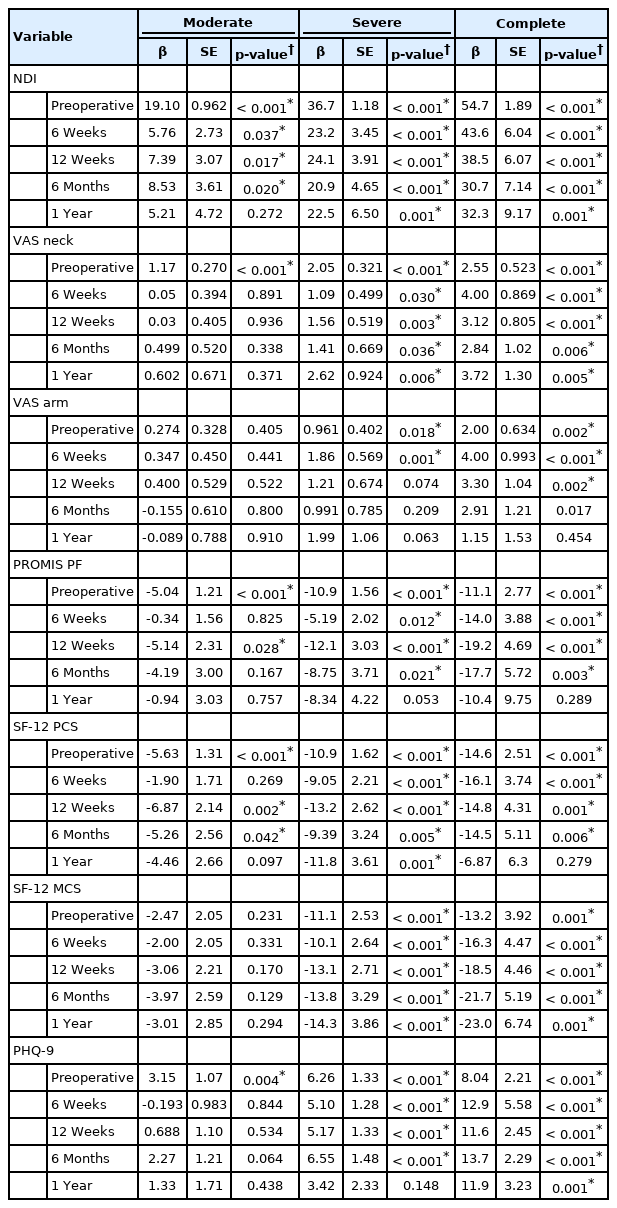
A summary of all multiple linear regression analyses is found in Table 4. Regression analysis demonstrated that relative to the none-to-mild group, preoperative NDI severity groups were significant effectors of preoperative NDI, VAS neck, PROMIS PF, SF-12 PCS, and PHQ-9 (p < 0.001, all). Similarly, severe and complete groups were also significant effectors of preoperative VAS arm and SF-12 MCS (p < 0.001, both). Postoperatively, the moderate severity group was significantly associated with NDI from 6 weeks through 6 months (p ≤ 0.037, all), 12 weeks only for PROMIS PF (p = 0.028), and 12 weeks through 6 months for SF-12 PCS (p ≤ 0.042, both). The severe disability group was a significant effector of NDI, VAS neck, SF-12 PCS, and SF-12 MCS at all postoperative timepoints (p ≤ 0.036, all) as well as VAS arm at 6 weeks (p = 0.001), PROMIS PF at 6 weeks through 6 months (p ≤ 0.021, all), and PHQ-9 from 6 weeks through 6 months (p < 0.001, all). Complete disability was a significant effector of all postoperative PROM scores (p ≤ 0.017, all) except for at 1 year for VAS arm, PROMIS PF, and SF-12 PCS (p ≥ 0.279, all).
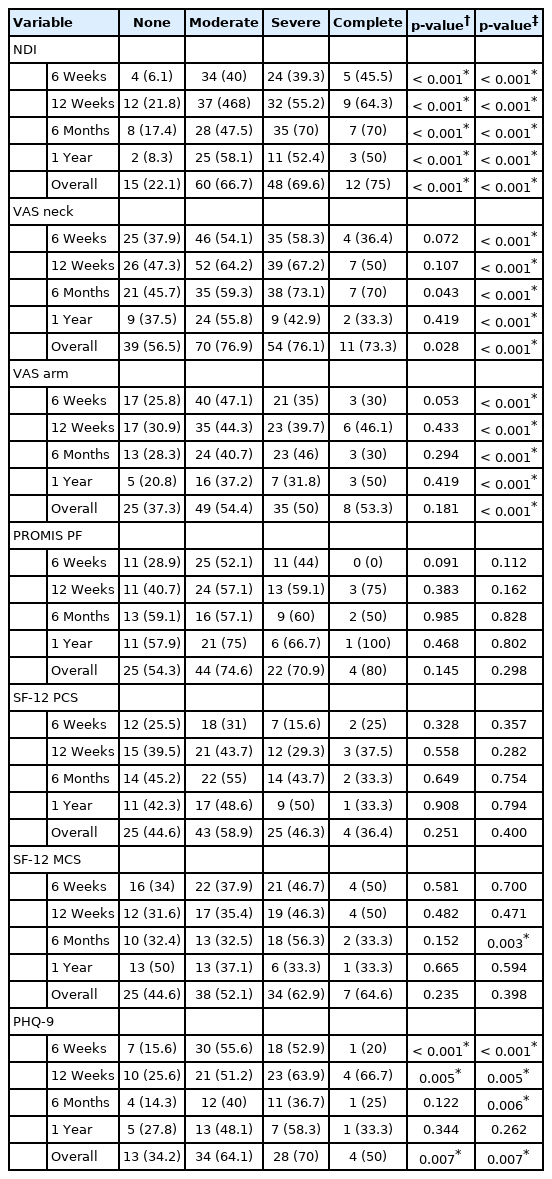
Evaluation of differences in the magnitude of improvement from the preoperative to all postoperative timepoints is summarized in Table 5. Mean improvement (delta) was significantly different between groups from 6 weeks through 1 year for NDI (p < 0.001, all). Additionally, a significant difference in mean delta VAS neck between groups was demonstrated at the 6-week through 6-month timepoints (p ≤ 0.009, all). Delta VAS arm and delta PHQ-9 demonstrated significantly different mean values at 6 months only (p = 0.025), and both 6 weeks and 12 weeks (p ≤ 0.011), respectively.
Preoperative neck disability severity had a significant impact on rates of MCID achievement at all postoperative timepoints for NDI (p < 0.001, all) and at 6 weeks, 12 weeks, and overall for PHQ-9 (p ≤ 0.007, all). When accounting for VAS neck and VAS arm, multiple logistic regression demonstrated a significant association with the achievement of MCID at all postoperative timepoints for NDI, VAS neck, and VAS arm (p < 0.001, all). The same was observed for SF-12 MCS at 6-months (p = 0.003) and PHQ-9 from 6 weeks to 6 months and overall (p ≤ 0.007). A summary of MCID achievement by severity group is summarized in Table 6.
DISCUSSION
Patients suffering from cervical spondylotic myelopathy or myeloradiculopathy often seek invasive treatments to alleviate their symptoms. While patients with severe symptoms typically find relief of pain and disability following surgery, past studies have indicated that surgical treatment for patients suffering from milder symptoms is similarly efficacious and safe [8,19]. However, it remains to be established whether the preoperative severity of symptoms may impact the extent of postoperative recovery of pain, disability, and both physical and mental health. The current study was able to establish that individuals suffering from more severe preoperative disability demonstrate similar changes in postoperative pain, physical and mental health, but not disability. Additionally, these individuals may also be restricted in the degree to which they improve, reporting worse postoperative PROMs compared to those with milder disability.
Evaluating the impact of the severity of preoperative disability on postoperative outcomes, whether surgical or patient-reported, has been seldom reported among spine literature. Patients in our study’s cohort reported worse preoperative and postoperative pain, disability, physical function, and mental health when compared to individuals with none-to-mild disability. Few other studies have evaluated outcomes by severity groups, but among published studies, patients were categorized according to their preoperative mJOA. At the preoperative timepoint, both Goh et al. [13] and Fehlings et al. [19] were able to demonstrate that patients with severe neck disability (mJOA< 9) had significantly worse NDI, Nurick Score, mJOA, and SF-36 PCS and MCS. Although we used NDI in place of mJOA for preoperative severity categorization, our study demonstrated a similar finding where patients in the moderate, severe, and complete disability groups had a significantly worse disability (NDI), physical function (PROMIS PF and SF-12 PCS), and mental health (SF-12 MCS and PHQ-9). Additionally, our study demonstrated that both arm and neck pain were significantly worse, a finding which was not reported by either study. In many regards, these results were expected as a number of studies have established the significant correlations between NDI and a variety of PROMs [23,24].
Postoperatively, patients with more severe preoperative disability demonstrated significantly worse postoperative outcomes as compared to the milder severity groups. While past studies align well with our preoperative results, the current literature is somewhat split on the impact neck disability has on outcomes. A prospective study of patients with severe degenerative myelopathy reported residual symptoms and disability following decompression surgery [7], which was similarly observed among our severe and complete disability groups. Other investigators have similarly established that a more severe preoperative neck disability translated into worse Nurick Scale, NDI, mJOA, and SF-36 PCS at the 2-year follow-up [13]. Interestingly, Goh et al. [13] observed no difference in these same outcomes at 6 months and their patient cohort reported no difference in pain among all groups irrespective of postoperative timepoint, which is in contrast to our results. While our study and others were able to establish differences among severity groups, a large-scale multicenter study of cervical spondylotic myelopathy patients contrarily reported that severity of neck disability, as measured by mJOA, had no impact on mean values for NDI, SF-36 PCS and MCS, with the exception of mJOA, out to 1 year. These differences may be due, in part, to the heterogeneity associated with the large-scale multicenter design (8 different centers) the study implemented. Whereas, comparatively, our study and the study of Goh et al. [13] were able to demonstrate minimal differences in study cohort demographics. On a more basic science level, our results may also be reflective of the biological changes to the central nervous system as a result of more severe neck disability. Holly et al. [25] was able to observe that cervical spondylotic patients with a higher NDI demonstrated significant functional connectivity changes to the pre- and postcentral gyri, the superior frontal gyrus, and supplementary motor area, all of which have implications in chronic pain and motor dysfunction [26], which are common symptoms among myelopathy and myeloradiculopathy patients. It may then be inferred that patients with worse disability at the preoperative level may inherently be limited to the extent they will recover postoperatively and surgeons may need to counsel patients on expected improvements.
Although patients may have demonstrated worse postoperative outcomes among the more severe neck disability groups, the magnitude of improvement was largely not affected. Given the close association NDI has with physical function outcomes [24,27-29], it was hypothesized that all three, the absolute score, degree of improvement, and MCID, should be limited by the extent of neck disability; however, delta values were only significantly different between groups for NDI and PHQ-9. In terms of delta values, our results align well with those of Fehlings et al. [19], where the degree of improvement in disability, physical and mental health (SF-36 PCS and MCS) were unaffected by preoperative severity. While our results regarding the achievement of MCID mirror those of Goh et al. [13], where a large proportion of patients achieved the threshold value for NDI and PCS, other investigators have also alluded that a higher JOA acted as a significant predictor of MCID achievement [14]. While our results largely are similar to these previous studies, it was interesting to observe that the only differences in mean delta and MCID achievement rates occurred for both NDI and PHQ-9. Differing results between mental health outcomes may stem from the specificity of the 2 psychometrics, with PHQ-9 better suited to capture depressive symptoms as it is based on the Diagnostic and Statistical Manual of Mental Disorders. These results may reflect the significant association of NDI with depressive symptoms reported by several previous studies [23,30-32]. Collectively, these results support the notion that the ability to achieve a significantly improved PROM score may not be influenced by preoperative severity of neck disability. There may be limitations to the extent of these improvements, but patients may not necessarily perceive this as an unfavorable outcome.
Given that patients with more severe disability largely demonstrated a similar level of postoperative improvement in pain, disability, physical function, and mental health, there is one possible explanation that may not be inherently clear. While myelopathy has its own set of symptoms, there is a number that does overlap with symptoms associated with radiculopathy. Previous studies have also demonstrated significant improvements in overall health-related quality of life and could be the underlying factor that may explain the similar improvements among patients who have a more severe disability [33]. However, the current study has accounted for signs of radiculopathy by way of VAS arm and VAS neck and largely found similar significant associations with NDI severity with PROM scores and MCID achievement. These results place a larger emphasis on the notion that a patient’s disability may not impede the ability to achieve a significant improvement in pain, disability, physical function, mental health, and overall quality of life. This will provide both patient and provider with the confidence to move forward with surgery for treatment of disabling cervical spine pathologies.
This study is not without limitations, which may affect the interpretation of results. The current study categorized patients according to preoperative NDI to represent the extent of neck disability severity as a result of myelopathy or myeloradiculopathy. However, radiographic analysis was not conducted for the purposes of this study, but may benefit future studies looking at the translational effect of spinal cord compression on postoperative outcomes. Another limitation is related to the use of health-related questionnaires completed by patients, which are prone to the responder and recall bias and could affect the values reported in this study. Additionally, the impact of duration of symptoms prior to surgical therapy may also influence how a patient responds to health questionnaires and ultimately may affect preoperative and postoperative outcomes. Future studies should calculate the duration of symptoms to determine the effects, if any, on preoperative NDI. Lastly, the generalizability of this study is limited as patients received treatment from a single surgeon at the same institution.
CONCLUSION
Patients suffering from varying degrees of neck disability severity due to cervical spondylotic myelopathy or myeloradiculopathy demonstrated significantly different preoperative pain, disability, physical function, and mental health. Postoperatively, differences in pain, disability, physical function, and mental health continued between severity groups. While postoperative PROM values demonstrated significant differences, the magnitude of improvement from preoperative values was not significantly different between severity groups except for neck disability and depressive symptoms. The same differences were observed for achievement of an MCID of NDI and PHQ-9. These results suggest patients with worse preoperative neck disability may be unable to achieve a similar level of improvement following cervical spine surgery.
Notes
The authors have nothing to disclose.