Outcomes of Posterior Lumbar Hemivertebra Resection and Short Fusion in Patients With Severe Sacral Tilt
Article information
Abstract
Objective
To introduce surgical strategies to restore coronal balance during limited fusion for early lumbar hemivertebra resection in patients with severe sacral tilt.
Methods
Sacral tilt was defined as a sacral tilt angle ≥ 5, and severe sacral tilt was defined as a sacral tilt angle > 10. From July 2004 to December 2017, 73 consecutive patients treated with posterior hemivertebra resection and short fusion in our institution were evaluated. Severe sacral tilt was noted in 26 patients (14 boys and 12 girls), and all were enrolled in this study. Undercorrection of the primary lumbar curve as compensation for the sacral tilt and short fusion was performed in these patients. The medical charts and imaging data of the patients were retrospectively reviewed to evaluate the outcomes.
Results
All patients were followed for at least 2 years. The mean age at the time of surgery was 3.7 (2–9) years old, with a total of 31 lumbar hemivertebra excised. On average, 2.8 (2–5) segments were fused for each patient. Sacral tilt minimally improved from 14.5° preoperatively to 13.6° postoperatively (p=0.15) and remained stable at the follow-up. The overall lumbar curve was 41.9° preoperatively, 11.7° immediately postoperatively, and 14.6° at the final follow-up. The segmental scoliosis curve was 39.1° preoperatively, 9.7° immediately postoperatively, and 11.2° at the final follow-up. Segmental kyphosis was corrected from 27.2° to 6.5° after the surgery and was 7.1° at the latest follow-up.
Conclusion
Sacral tilt is seen in patients with congenital scoliosis in lumbar hemivertebra. Undercorrection of the lumbar curve and segmental scoliosis to compensate for sacral tilt and short fusion after hemivertebra resection may be helpful to restore coronal balance and preserve mobility in segments in patients with pronounced severe sacral tilt.
INTRODUCTION
The main goals of spinal deformity surgery are to prevent progression, restore the alignment of the spine in both the coronal and sagittal planes and preserve mobility and function in segments to the greatest extent possible. The sacrum plays an important role in the balance of the spine and pelvis, as it is located at the base of the spine and serves as a foundation for mechanical loading. The importance of treating lumbosacral deformities in patients with degenerative scoliosis has been well studied [1]. The etiologies of lumbosacral deformities in young patients with spinal deformities may be different from those in patients with degenerative scoliosis. It has been reported that lumbosacral deformities due to sacral tilt exist in patients with adolescent idiopathic scoliosis (AIS) and may influence surgical outcomes, especially in the restoration of coronal balance [2-4]. Until now, there have been no reports on sacral tilt in patents with congenital scoliosis (CS).
The natural history of CS has been well studied [5-7]. Hemivertebra is the most common type of CS, and some curves due to hemivertebra are progressive due to the growth potential of the spine, most notably in the lower thoracic, thoracolumbar or lumbar spine [7,8]. In addition to the primary curve, compensatory secondary structural curves may develop in response to asymmetric development. Delayed treatment will lead to higher risks related to surgery and necessitate the fusion of more vertebral levels [9]. As a result, early surgical intervention is mandatory for most patients with CS due to hemivertebra to achieve better correction while preserving as many motion segments as possible. Hemivertebral resection, first performed via a combined anterior-posterior approach, has become the most popular surgery for CS [10.11]. Many studies have described the outcomes of posterior hemivertebral resection [12-17]. However, no studies have described sacral tilt in CS and the role of sacral tilt in restoring coronal balance in patients with lumbar hemivertebra resection and short fusion. Therefore, this study was conducted to evaluate sacral tilt in patients who have undergone lumbar hemivertebra resection, introduce surgical strategies for the treatment of sacral tilt during surgery, and determine the influence of these strategies on coronal balance.
MATERIALS AND METHODS
Inclusion criteria: After the institutional review board approved this study, 73 consecutive patients with CS undergoing posterior hemivertebra resection and short fusion (fewer than 5 segments) in our institution from July 2004 to December 2017 were included. Sacral tilt was defined as a sacral tilt angle ≥ 5°. Considering the Scoliosis Research Society’s definition of scoliosis, a Cobb angle > 10°, the authors defined severe sacral tilt as a sacral tilt angle > 10°. When the sacral tilt ≤ 10°, the compensatory changes were considered mild and no special strategies were taken and these patients were excluded in this study. The authors utilized strategies to undercorrect the segmental curve in the patients with severe tilt, and these patients were enrolled in this study. For these patients, the medical charts and radiographs were studied. All patients were followed up in the outpatient department at 3 months, 6 months, and then yearly after surgery. All patients were followed for at least 2 years.
This study was approved by the Institutional Review Board of Peking Union Medical College Hospital (approval number: S-K1729).
1. Radiographic Evaluation
Full-length standing posteroanterior and lateral x-ray films were taken preoperatively, at 1–2 weeks postoperatively, and at each follow-up. All patients underwent preoperative computed tomography (CT) scans and 3-dimensional reconstruction of the spine to assess the morphology of the hemivertebra and sacrum.
Coronal and sagittal parameters were measured according to the method provided by Bollini et al. [10]. The segmental curve was measured between one level above and below the hemivertebra, whereas the entire lumbar curve was the maximal Cobb angle obtained in the lumbar spine. The cranial compensatory curve was measured as the maximal Cobb angle of the proximal unfused spine. The trunk shift (TS) was the horizontal distance between the center of C7 and the central sacral vertical line (CSVL). In addition, upper instrumented vertebral translation (UIVT) and lower instrumented vertebral translation (LIVT) were measured as the distances between the center of the instrumented vertebra and the CSVL, respectively.
The degree of sacral tilt was typically defined as the angle between the horizontal line and the upper end plate of the sacrum on the posteroanterior x-ray films. However, changes in sacral tilt, which is parallel to the bi-iliac crest tangent line, can occur secondary to abnormalities of the spine and lower extremities and can be corrected with the correction of the primary abnormalities. The authors excluded secondary sacral tilt by defining the tilt angle as the angle between the bi-iliac crest tangent line and the upper endplate of the sacrum. Sacral tilt was defined as an angle ≥ 5°, and severe sacral tilt was defined as an angle > 10°. Upper instrumented vertebra (UIV) tilt was measured as the angle between the upper endplate of the UIV and the bi-iliac crest tangent line (Fig. 1).
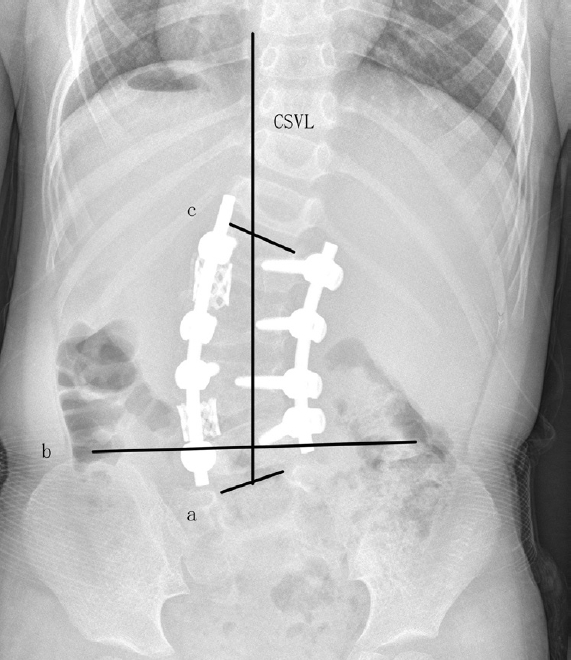
The angle between lines a and b was the sacral tilt angle. The angle between lines b and c was the upper instrumented vertebral tilt angle. CSVL, central sacral vertical line.
On the sagittal plane, true segmental kyphosis was defined as the difference between the measured segmental kyphosis angle (between the 2 vertebrae adjacent to the hemivertebra) and normal segmental kyphosis angle, as noted by Bernhardt and Bridwell [18]. Global sagittal balance was the distance from the C7PL (C7 plumb line) to the perpendicular line drawn from the superior posterior endplate of the S1 vertebral body. Thoracic kyphosis was measured from T5 to T12, and lumbar lordosis was measured from L1 to S1. The thoracolumbar junction was assessed from T10 to L2. All measurements were performed with Surgimap 2.2 (Nemaris, Inc., Methuen, MA, USA).
All radiographic assessments were performed by 2 attending spine surgeons, and repeated measurements were performed by the same surgeons. The means of all measurements were used in the final analysis to reduce measurement error.
2. Surgical Technique
To preserve the function of the lumbosacral region, the sacral tilt was left untreated in all patients. However, the lumbar curve in the patients with severe sacral tilt was undercorrected during surgery to compensate for the pronounced severe sacral tilt.
All patients were treated with posterior hemivertebra resection and short fusion. After general anesthesia, the patient was placed in a prone position and draped in a routine sterile fashion. A standard midline incision was made, and the levels to be treated were exposed. Once the levels were prepared to be excised and instrumented, instrumentation and hemivertebra resection were performed. The vertebral body of the hemivertebra and its upper and lower discs were completely removed, and the contralateral disc and bar were also resected. A titanium mesh cage was implanted into the gap for undercorrection, and compression was applied to close the gap and correct the deformity (Fig. 2). Additional compression or distraction was applied to improve the degree of correction. The residual segmental curve was preserved instead of fully correction of the segmental curve. Intraoperative fluoroscopy was used to check the position of the UIV and the residual segmental curve. The magnitude of the residual segmental curve was intended to be similar to the degree of sacral tilt. In other words, the correction angle was intended to be similar to the degree of segmental curve minus sacral tilt. Then, the screws were locked, and posterolateral fusion was performed. The incision was closed with a subfascial drain.
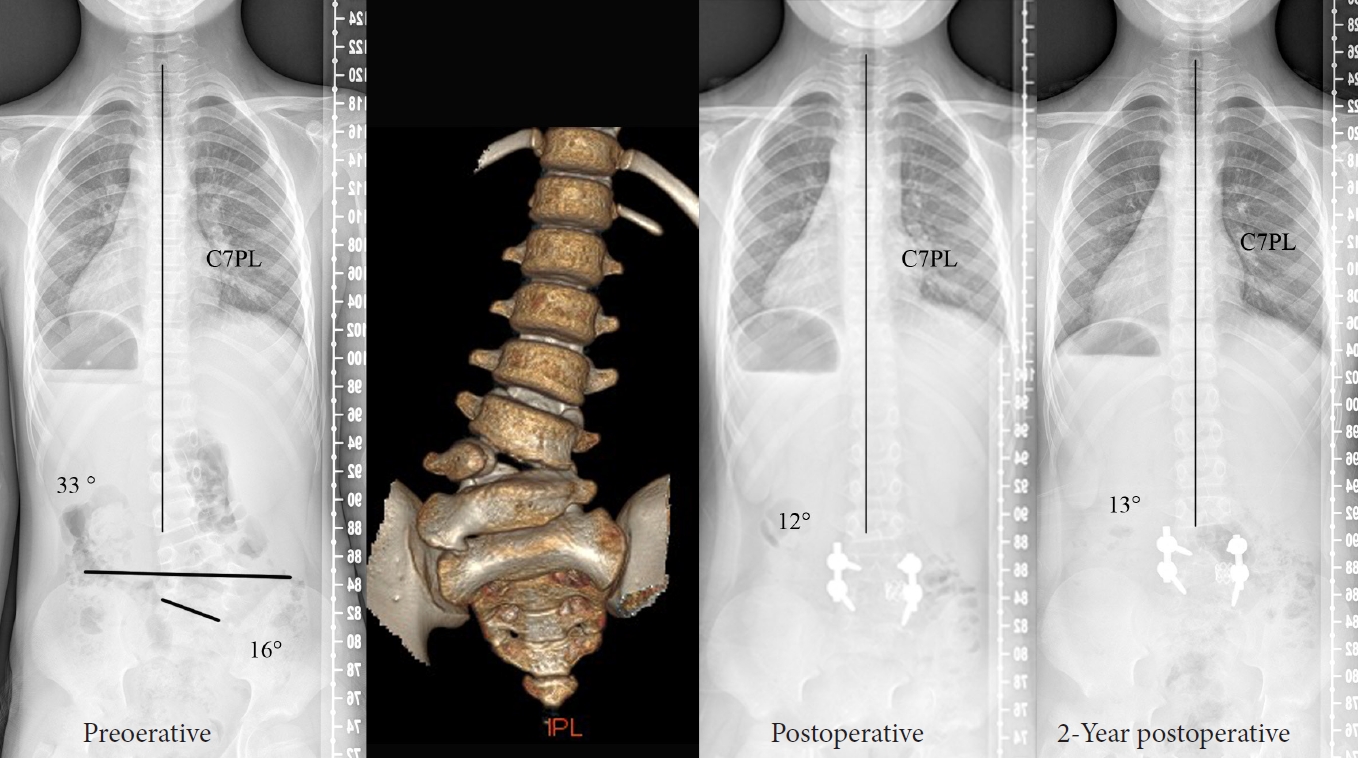
A 7-year-old boy had hemivertebra between L4 and L5, with a sacral tilt of 16°. The major lumbar curve was 33°. A severe sacrum tilt was noted on the computed tomography scan. Posterior hemivertebral resection with monosegmental fusion was performed. A titanium cage was implanted in the osteotomy gap for undercorrection to compensate for the sacral tilt, leaving a residual curve of 12°. The correction after the surgery was satisfactory. The residual curve progressed to 13°, and good coronal alignment was well maintained during the 2-year follow-up period. C7PL, C7 plumb line.
Multimodality neurophysiologic monitoring of the spinal cord, including motor evoked potential and somatosensory evoked potential monitoring, was performed in all surgeries. Postoperatively, patients ambulated with a 2-piece plastic brace for 6 months.
3. Statistical Analysis
The results are presented as the means and standard deviations for the continuous variables and frequencies for the categorical variables. The p-values were calculated using t-tests or nonparametric tests, and p<0.05 indicated a significant difference.
RESULTS
Sacral tilt was found in 49 patients (67.1%). Severe sacral tilts were noted in 26 patients, with an incidence of 35.6%. Twenty-six consecutive patients (14 boys and 12 girls) were enrolled. The mean age at the time of surgery was 3.7 (2–9) years old, with an average follow-up duration of 36.5 (24–88) months. A total of 31 (above L3–9, at or below L3–22) lumbar hemivertebrae were excised, averaging 1.2 (1–2) hemivertebrae per patient. The average number of fused segments was 2.8 (2–5) for each patient. The demographics of all patients are summarized in Table 1.
There were no significant differences in sacral tilt from before to after surgery (p=0.15). In the coronal plane, undercorrection of segmental scoliosis and the major lumbar curve was performed. The major lumbar curve was 41.9° preoperatively, 11.7° postoperatively, and 14.6° at the latest follow-up. The segmental scoliosis curve was 39.1° preoperatively, 9.7° postoperatively, and 11.2° at the latest follow-up. There was no significant correction loss of the segmental scoliosis curve (p=0.09) or major lumbar curve (p=0.15). The cranial and caudal compensatory scoliosis curves significantly improved after surgery and maintained correction during the follow-up period. The UIV tilt improved from 27.3° to 6.7° after the surgery, and a 2.8° loss of correction was found at the latest follow-up. The TS was 15.7 mm preoperatively, 15.6 mm immediately after surgery and improved significantly (p<0.05) at the latest follow-up. Significant improvements in upper instrumented vertebral angle, lower instrumented vertebral angle, UIVT, and LIVT were found immediately after the surgery and maintained during the follow-up period. In the sagittal plane, segmental kyphosis significantly improved from 27.2° to 6.5° after the surgery, and no significant correction loss occurred during the follow-up period. No significant changes were found in thoracic kyphosis, thoracolumbar junction alignment, lumbar lordosis, or the sagittal vertical axis. The correction results are shown in Table 2.
Poor wound healing occurred in 1 patient, who was treated with irrigation and debridement. Malpositioning of a pedicle screw occurred in 1 patient, but revision surgery was not indicated since there were no related symptoms. Transient root irritation occurred in 2 patients. Both of them had radicular pain after surgery. A CT scan was performed to rule out root and dura compression. Both of the patients recovered completely during the follow-up period. No major neurologic complications occurred.
DISCUSSION
Sacral tilt can result from primary problems such as sacral rotation, compensation for a scoliotic spine, and leg length discrepancy or primary congenital sacrum deformities [2-4]. Secondary sacral tilt is nearly parallel to the pelvis obliquity and can be improved with correction of the primary deformities. CS is more likely to be associated with other skeletal deformities, and congenital sacral malformation may have been the most common cause of sacral tilt in our study.
The role of the sacral tilt in surgeries for spinal deformities in children has not been well studied. We found some studies evaluating the role of sacral tilt in correction surgeries for AIS. Lee et al. [4] first described sacral tilt in AIS, and the frequencies of sacral tilt were 19.5%, 29.6%, and 40.6% when using the criteria of 5°, 4°, 3°, respectively. Cho et al. [2] found that the proportion of patients with ≥ 5° of sacral tilt among those with < 3° of pelvic obliquity was 8.9% in their cohort of AIS patients. They found that sacral tilt may be a compensatory mechanism for large lumbar curves that are accompanied by pelvic obliquity abnormalities. Of note, a congenitally tilted upper sacrum may contribute to scoliosis in some AIS patients. The authors reported that leg length discrepancy is not directly correlated with sacral tilt. Joo et al. [3] reported that the frequency of sacral tilt ≥ 3° was 28.6% (36 of 126 patients) in their study of AIS patients. However, the authors defined the degree of sacral tilt as the angle between the horizontal line and the upper endplate of the sacrum with the sacral tilt in most cases, likely due to compensatory secondary pelvis obliquity, which may be corrected after spinal surgeries.
To date, no studies have described sacral tilt in patients with CS. In the present study, the authors defined the degree of sacral tilt as the angle between the bi-iliac crest tangent line and the upper endplate of the sacrum to rule out the impact of lower limb discrepancies, patient habitus, and pelvic obliquity due to spinal deformities such as those reported in patients with neuromuscular scoliosis caused by cerebral palsy [19,20]. Due to difficulty in distinguishing angles of 5°, 4°, and 3°, measurement bias may have been a source of error in the study. This error has been investigated and was suggested to be approximately 5° [21,22] but could be as small as to 3° in CS [23]. Most investigators have considered changes ≥ 5° to be clinically important [24], and a difference of more than 5° can minimize the measurement variation. As a result, sacral tilt was defined as a sacral tilt angle ≥ 5°. The frequency of sacral tilt in the present study was 67.1%, which was much higher than that reported in patients with AIS [2].
Sacral tilt may affect the coronal balance in correction surgeries for spinal deformities in children. When the sacral tilt is not addressed, coronal imbalance may occur after correction surgery for spine deformities (Fig. 3). Lee et al. [4] noted that sacral tilt should be considered when the distal fusion level is selected to avoid coronal decompensation when planning corrective surgery in patients with AIS. Joo et al. [3] found that sacral tilt typically occurred to the left in the Lenke 4-L type cases and to the right in the Lenke 4-R type cases and was associated with a higher probability of the adding-on phenomenon. In this study, the lumbosacral curve was not severe and was left untreated to preserve the important function of the lumbosacral region. However, the existing lumbosacral curve should be considered in the reconstruction of coronal balance. In children undergoing hemivertebral resection and short fusion, coronal imbalance with progressive deterioration of the coronal TS is rare because there are many mobile segments for compensation. However, correction loss or an “adding-on”-like phenomenon may lead to a longer lumbar curve extending to adjacent mobile segments. This occurs after surgery as a result of compensation for the lumbosacral curve with sacral tilt if the primary lumbar scoliosis curve is completely corrected. Thus, attention should be placed to the lumbosacral curve with severe sacral tilt in preoperative planning. In this study, special strategies were not taken during the surgery in patients with sacral tilt ≤ 10° because the compensatory changes for sacral tilt were usually mild in these patients. Considering the Scoliosis Research Society (SRS)’s definition of scoliosis, a Cobb angle > 10°, the authors defined severe sacral tilt as a sacral tilt angle > 10°. For patients with lumbosacral curves with severe sacral tilt, maximal correction of the main lumbar curve may lead to an increase in UIV tilt (Fig. 4). With UIV deviation, the lumbar curve may deteriorate and extend to the proximal mobile spine. Cranial compensatory curves or wedge-shaped discs may lead to issues that will negatively impact the spine. Thus, undercorrection with asymmetrical cage placement in the osteotomy gap is recommended to compensate for the residual lumbosacral curve in patients with severe sacral tilt. A titanium mesh cage was inserted to the convex side to decrease the postoperative UIV tilt and achieve a median UIV (Fig. 5). The degree of residual segmental scoliosis should be similar to that of the sacral tilt.

A 15-year-old female had L3/4 hemivertebra with severe sacral tilt. Surgery was indicated for low back pain at a local institution. The hemivertebra was resected, and the whole lumbar curve was corrected with long-segment fusion from T12 to L5. However, coronal decompensation worsened significantly after the surgery and did not improve during the 9-year follow-up period.

(A) Maximal correction of the primary lumbar curve in patients with a severe sacral tilt will lead to tilt and deviation of the fusion mass from the central line. (B) Undercorrection can compensate for the sacral tilt and provide a more level and medial upper instrumented vertebral at the base of the mobile proximal spine.
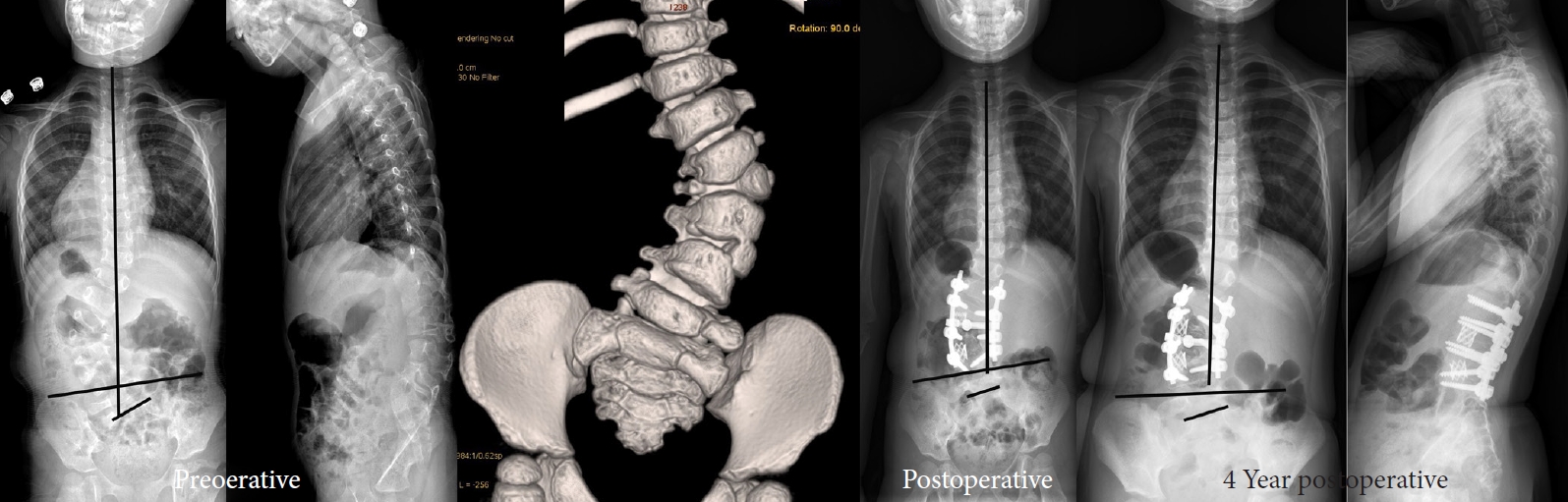
A 2-year-old female suffered from severe lumbar kyphoscoliosis due to 2 ipsilateral fully segmented hemivertebrae with sacral tilt. Hemivertebral resection of both hemivertebrae with short fusion was performed. Two titanium cages were inserted into the 2 osteotomy gaps for undercorrection to compensate for the sacral tilt. The correction looked good on the postoperative x-ray. During the 3-year follow-up, alignment in both the coronal and sagittal planes was well maintained.
Although we first described the role and treatment of lumbosacral curves with sacral tilt in patients who underwent lumbar hemivertebra resection for CS in this study, there are some potential limitations. First, this was a retrospective study, and avoiding maximal correction was an empirical conclusion; and the authors did not conduct a case-control study due to obvious ethical concerns. Second, some patients were still too young to complete the SRS-22 questionnaire at the latest follow-up, thus we could not acquire the SRS-22 questionnaire at latest follow-up.
CONCLUSION
Sacral tilt may exist in patients with CS with lumbar hemivertebra. In patients with a significant severe sacral tilt, if the lumbosacral curve is left untreated, surgical treatment with undercorrection of the major lumbar curve and segmental scoliosis curve to compensate for the lumbosacral curve with sacral tilt should be performed to achieve better coronal alignment in cases requiring short fusion.
Notes
The authors have nothing to disclose.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81171673, 81972037 and 81902178), Beijing Natural Science Foundation (No. L192015). The manuscript submitted does not contain information about medical device(s)/drug(s).


