Which Is More Predictive Value for Mechanical Complications: Fixed Thoracolumbar Alignment (T1 Pelvic Angle) Versus Dynamic Global Balance Parameter (Odontoid-Hip Axis Angle)
Article information
Abstract
Objective
In this study, we investigate about relationship between postoperative global sagittal imbalance and occurrence of mechanical complications after adult spinal deformity (ASD) surgery. In global sagittal balance parameters, odontoid-hip axis (OD-HA) angle and T1 pelvic angle (TPA) were analyzed.
Methods
Between January 2009 and December 2016, 199 consecutive patients (26 males and 173 females) with ASD underwent corrective fusion of more than 4 levels and were followed up for more than 2 years. Immediate postoperative and postoperative 2 years whole spine x-rays were checked for evaluating immediate postoperative OD-HA, TPA, and other parameters. In clinical outcomes, back and leg pain visual analogue scale, Scoliosis Research Society-22 spinal deformity questionnaire (SRS-22), Oswestry Disability Index (ODI), 36-item Short Form Health Survey (SF-36) were evaluated.
Results
Based on the occurrence of mechanical complications, a comparative analysis was performed for each parameter. In univariable analysis, mechanical complications were significantly much more occurred in OD-HA abnormal group (odds ratio [OR], 3.296; p<0.001; area under the curve [AUC]=0.645). In multivariable analysis, the result was much more related (OR, 2.924; p=0.001; AUC=0.727). In contrast, there was no significant difference between normal and the occurrence of mechanical complications in TPA. In clinical outcomes (normal vs. abnormal), the differences of SRS-22 (0.88±0.73 vs. 0.68±0.64, p=0.042), ODI (-24.72±20.16 vs. -19.01±19.95, p=0.046), SF-36 physical composite score (19.33±18.55 vs. 12.90±16.73, p=0.011) were significantly improved in OD-HA normal group.
Conclusion
The goal of ASD surgery is to improve patient life quality through correction. In our study, TPA was associated with spinopelvic parameter and OD-HA angle was associated with health-related quality of life and complications. OD-HA angle is predictable factor for mechanical complications after ASD surgery.
INTRODUCTION
Degenerative changes have the potential to greatly disrupt the normal curvature of the spine, leading to sagittal malalignment [1]. The interaction between deformity and compensatory mechanisms depicts the final presentation of patients with adult spinal deformity (ASD) [2]. ASD is a debilitating condition that often requires surgical correction. In case of severe deformity, surgical treatment has been shown to offer better clinical and radiological outcomes compared with nonoperative treatments [3-5].
However mechanical failure, such as proximal junctional kyphosis (PJK), proximal junctional failure (PJF), or rod fracture is one of the most common complication and have substantial incidence in ASD surgery. There were many studies to investigate about risk factors or predictive factors of mechanical failure after ASD surgery [6-11]. Among these radiologic parameters, increasing evidence implies that sagittal vertical axis (SVA) alone does not fully reflect sagittal malalignment, and global spinal pelvic alignment such as the T1 pelvic angle (TPA) assessment provides a more complete picture of the mechanisms for maintaining an upright posture [12]. Thus, TPA is one of the global tilt parameters that is not affected by posture with good parameter for showing thoracolumbar alignment. On the other hand, as Le Huec et al. [13] summarized the sagittal balance of the spine, odontoid-hip axis (OD-HA) angle includes a cervical alignment and have been proven to represent a constant global sagittal parameter which could show current patients posture according to gravity line [14].
TPA corresponds to the angle between a line connecting the center of T1 to the center of the femoral heads and the line to the center of the S1 endplate. It has been correlated with pelvic tilt (PT) and SVA, but does not account for pelvic incidence (PI) value. The TPA target value is under 14° and OD-HA angle is the angle between the vertical and the highest point of the dens connecting the center of the acetabulum [15,16]. The OD-HA angle target value is +2° to -5°. This angle takes into account the position of the cervical spine, the thoraco-lumbar spine and pelvis, and may benefit an overall analysis and assessment of the risk of PJK after ASD surgery (Fig. 1) [13,14,17].
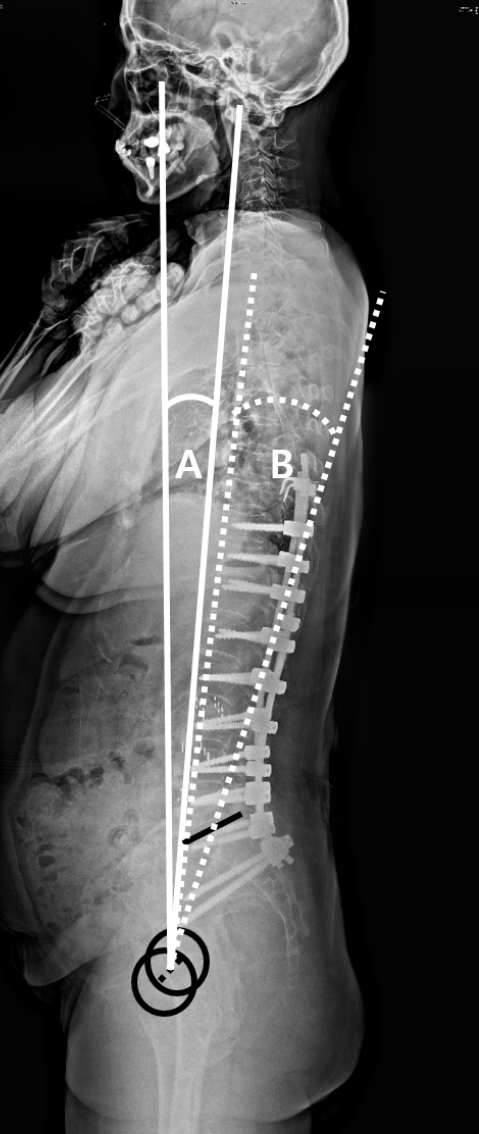
Measurement of global balance parameters. (A) Odontoid-hip axis (OD-HA) angle. OD-HA angle (white lines) is the angle between the vertical and the hightest point of the dens connecting the center of the femoral heads (black dotted line, center of the black circles). The OD-HA angle target value is +2° to -5°. (B) T1 pelvic angle (TPA). TPA (white dotted lines) corresponds to the angle between a line connecting the center of T1 to the center of the femoral heads (black dotted line, center of the black circles) and the line to the center of the S1 endplate (black line). The TPA target value is under 14°.
Although both of these parameters have been proved to reflect global balance, there is little comparative study between these 2 parameters with regard to impact on mechanical complications or patients’ reported outcome.
Therefore, this study aimed to investigate which one would be a good representation of a patient’s global balance, to predict clinical outcome and the occurrence of mechanical complications after surgery for patients with ASD.
MATERIALS AND METHODS
1. Patient Population
We retrospectively reviewed patients with ASD who underwent posterior spinal fusion and instrumentation in 2 centers. Inclusion criteria were as follows: (1) patients who underwent surgical corrective surgery for ASD; (2) those with at least one of the following radiologic criteria: coronal Cobb angle more than 20°, SVA more than 5 cm, PT more than 25°, and/or thoracic kyphosis (TK) more than 60°; (3) those who underwent posterior spinal fusion and instrumentation as ASD surgery for more than 4 levels; and (4) those with a follow-up period of more than 24 months. Exclusion criteria were (1) patients with ASD secondary to syndromic, autoimmune, infectious, tumor, or other pathologic conditions: (2) those who underwent ASD surgery for fewer than 4 levels; and (3) those with a follow-up period less than 24 months.
Between February 2011 and January 2018, 454 patients with ASD underwent spinal surgery in our institute. Among them, we excluded 253 patients whose follow-up period was less than 2 years, and those who were not indicated for corrective surgery for ASD or whose surgery level was 3 levels or less. Finally, 199 consecutive patients with sagittal imbalance who underwent ASD surgery were included.
The demographics of patients, such as age, sex, bone mineral density (BMD), body mass index (BMI) were also conducted. Dual-energy x-ray absorptiometry scan to measure BMD at the spine and hip.
This study was approved by each hospital’s Institutional Review Board, and all participants provided written informed consent.
2. Radiological Assessments
In order to minimize the error, our study used the radiographic measurement manual introduced by the Scoliosis Research Society for whole spine radiograph imaging. A 36-inch whole spinal anteroposterior and lateral planar radiographs were collected at a distance of 72 inches from the film. The patient was standing in a comfortable position with the knees fixed, feet shoulder-width apart, looking straight ahead, elbows bent, and the knuckles of the supraclavicular fossa bilaterally [18,19].
All radiologic evaluation of OD-HA angle and TPA were conducted at 4 weeks postoperatively. The normal value of OD-HA angle is +2° to -5°, and normal value of TPA was under 14° [13].
And whole spine anteroposterior/lateral was performed at postoperatively 2 years to evaluate mechanical complications; such as PI, sacral slope, L1-S1 lordosis (LL), PT, SVA, and PI–LL. In order to reduce the error between individual measurements, a software program called Surgimap (https://www.surgimap.com/) was used. Also, level of fusion vertebra, uppermost instrumented vertebra (UIV) and lowest instrumented vertebra (LIV), and state of spinopelvic fixation (SPF) were conducted.
3. Mechanical Complications and Clinical Outcomes
Mechanical complications were defined as PJK or PJF, distal junctional kyphosis (DJK) or distal junctional failure, rod fracture, and implant-related complications [20,21]. Implant-related complications were defined as rod breakage or prominence, painful implant, screw breakage, loosening, or malposition, implant (interbody graft, hook, or set-screw) dislodgement [20,22].
In clinical assessments, patients reported pre- and postoperative 24-month back and leg pain using a visual analogue scale (VAS) scored from 0–10. The Oswestry Disability Index (ODI), Scoliosis Research Society-22 spinal deformity questionnaire (SRS-22), and 36-item Short Form Health Survey (SF-36) were used to measure health-related quality of life (HRQoL) measures.
4. Statistical Analysis
Statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Demographic and radiological data were compared using independent t-test and categorical variables using chi-square test or Fisher exact test. The logistic regression model is established with mechanical complications, PJK, PJF, and implant-related failure as outcome. The results are expressed as mean±standard deviation or number (percentage). A p-value less than 0.05 was considered statistically significant.
RESULTS
A total of 199 patients (26 males and 173 females) were retrospectively reviewed. The average age was 67.36 years (range, 49–80 years), and they were followed for an average of 30.54 months (range, 24–118 months).
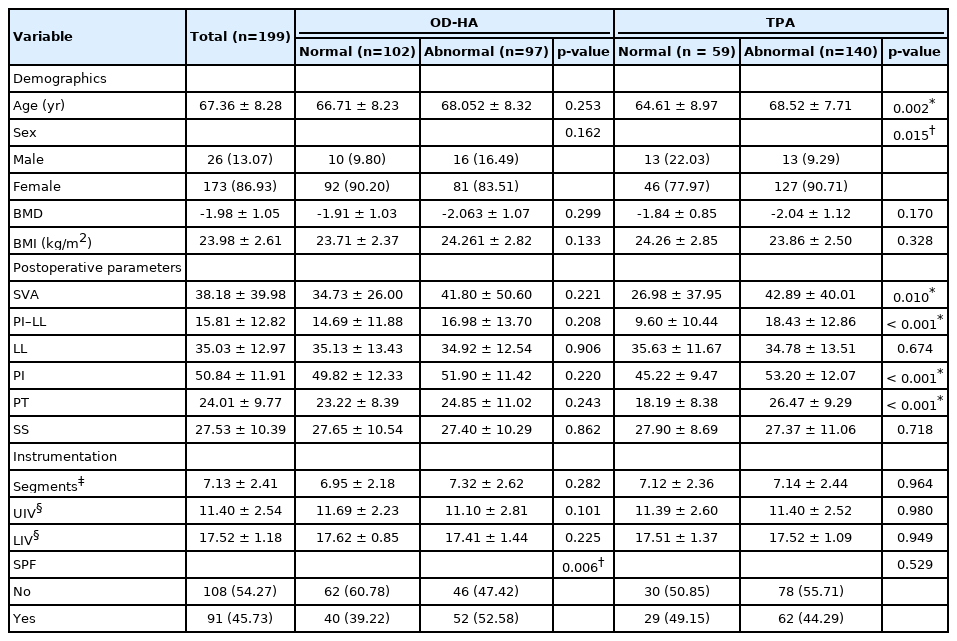
Patients were classified according to normal TPA and OD-HA angle values. In the OD-HA angle group, 102 patients were in the normal range and 97 patients were in the abnormal range, In the TPA group had 59 patients with a normal range and 140 patients with an abnormal range. Although the OD-HA angle group showed no difference between normal and abnormal groups in demographic comparisons, the TPA group had a high average age and female ratio in the abnormal group. In radiological assessments, postoperative sagittal balance parameters were compared with fusion segment, UIV, LIV, and SPF via whole spine radiographs anteroposterior/lateral view for the 2 years after surgery. In postoperative parameters, in OD-HA angle groups, the normal group was on average close to normal compared to the abnormal group, but there was no statistical significance. On the other and, the TPA group showed differences in SVA, PI–LL, PI, and PT values, which were statistically significant. For instrumentation, on average, there were 7 fusion segments, T11–12 for UIV, L5–S1 for LIV. In these results, both OD-HA angle and TPA were not different in normal and abnormal groups. In SPF, 91 patients were administered and 108 were not. In this result, OD-HA angle was significantly more frequent in the normal group, and there was no difference between the 2 groups in TPA (Table 1).
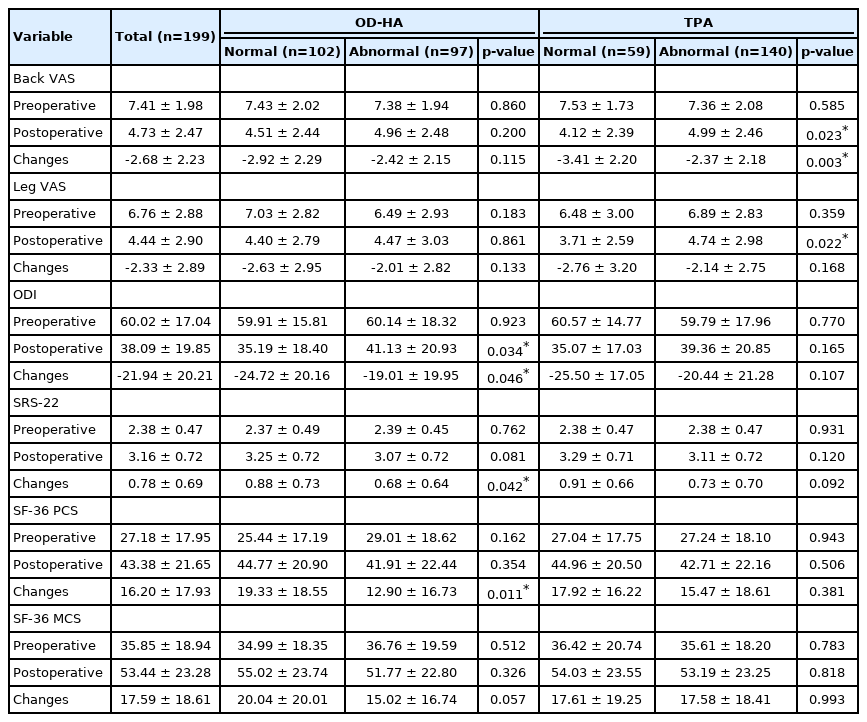
In clinical assessments, back and leg VAS related to pain and ODI, SRS-22, SF-36 related to functional impairment were analyzed. First of all, there was no significant difference in pain between normal and abnormal groups in the OD-HA angle group. However, there were significant differences in the change values of ODI, SRS-22, and SF-36 physical composite score related to the functional impairment. On the other hand, in the TPA group, there was no significant difference in functional impairment between normal and abnormal groups, but in the case of pain, the results were particularly favorable in the back pain, which was statistically significant (Table 2).
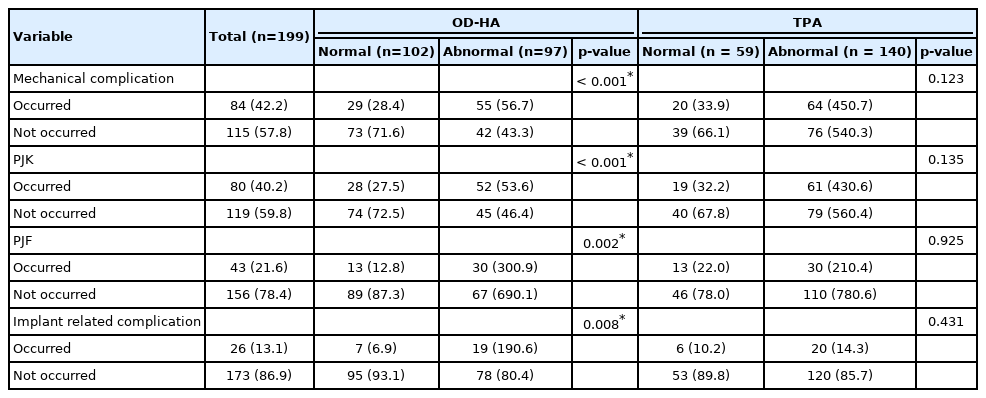
A simple comparison of the patients’ mechanical complication, PJK, PJF, and implant-related complication was conducted. In the entire patient population, the incidence of complications (n, %) was mechanical complication (84 of 199, 42.2%), PJK (80 of 199, 40.2%), PJF (43 of 199, 21.6%), implant-related complication (26 of 199, 13.1%). In simple comparison, there was no difference between normal and abnormal groups in TPA, but in C2HA, there was a difference between normal and abnormal groups. [Normal (n, %) vs. abnormal (n, %), p-value, mechanical complication (29 of 102, 28.4%) vs. (55 of 97, 56.7%), p<0.001; PJK (28 of 102, 27.5%) vs. (52 of 97, 53.6%), p<0.001; PJF (13 of 102, 12.8%) vs. 30 of 97, 30.9%, p=0.002; implant-related complication (7 of 102, 6.9%) vs. 19 of 97, 19.6%, p=0.008] (Table 3).
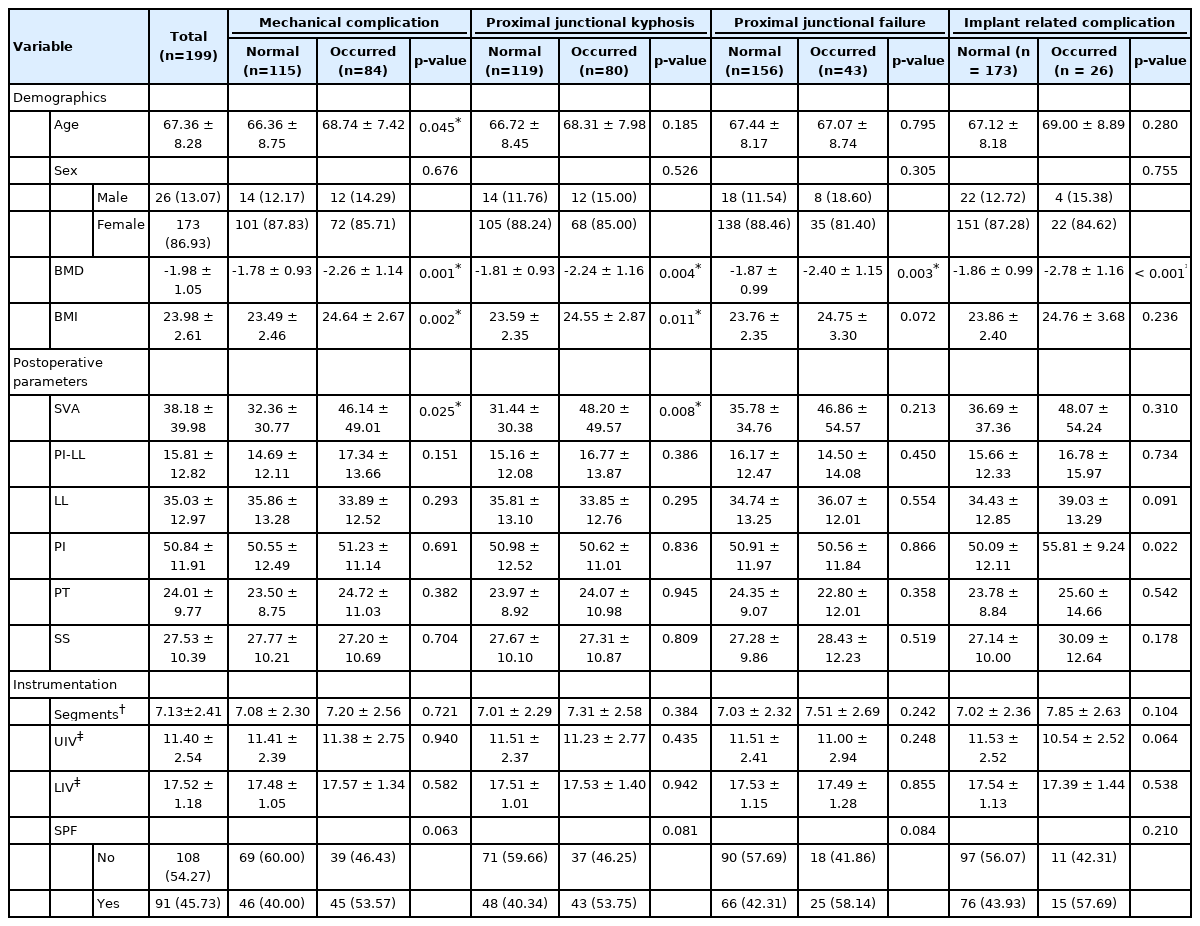
In order to investigate the correlation more closely, a logistic regression was constructed using mechanical complication, PJK, PJF, and implant-related complication as outcomes. In univariate analysis, OD-HA angle, age, BMD, BMI, postoperative SVA was related with postoperative mechanical complication. In multivariable analysis, OD-HA angle was related with postoperative mechanical complication (OR, 2.924; p=0.001; AUC=0.727) (Table 4, Fig. 2).
DISCUSSION
Recent studies on outcomes following ASD surgeries have shown high rates of complications (8.4%–42%) and revision rates (9%–17.6%) [2,12,23-25]. In our study, the overall mechanical complication occurred in about 42%, and revision rate was about 21%. This is slightly higher than other studies, but does not show much difference [3,11,22].
The occurrence of mechanical complications after ASD surgery has already been dealt with in several studies. In previous studies, thoracoplasty, posterior spinal fusion, combined anteroposterior spinal fusion preoperative existence of more than 5° proximal junctional angle one level above UIV, fusion to the sacrum and surgical correction of TK more than 50% was suggested as risk factors for PJK [7,11,26-29]. And older age (over 55 years), large abnormal preoperative sagittal parameters, osteoporosis, high BMI, thoracoplasty, and fusion to the lower lumbar vertebra and sacrum was suggested as risk factors for PJF [12,30-33].
Yagi et al. [11] demonstrated that PJK can be minimized by postoperative normalization of global spine alignment and balance. Thus, we analyzed the difference according to whether normality of the postoperative global balance parameters TPA and OD-HA angle.
It is done through cervical curvature and lumbar lordosis in order to maintain a horizontal gaze and to free the upper limbs. It is important to analyze the problem statically and dynamically to understand the conditions required for this balance. Recently, several studies demonstrated that OD-HA angle was characterized the overall spinal balance, remains constant whatever the age and despite variations of lordosis (which decreases with loss of disc height) and the presence of compensation mechanism. And it hardly varies and is a good way to study the overall sagittal balance. It integrates the cervical spine and head and stays constant even in elderly if they are asymptomatic [13-15].
In Dubousset’s conus of economy (ref), the concept of balance includes from head to lower limbs. Therefore, the center of the head, that is, the center of C2, which is a line descending from the center of the external auditory meatus, can be regarded as the center of gravity. For that reason, OD-HA could be a good indicator of global balance in terms of the concept of Dubousset’s conus of economy that global balance is the ability of a person to stand upright with respect to gravity and that it is efficient to use the least energy. However, there are not many studies yet analyzed whether this indicator can predict mechanical complications in ASD.
Protopsaltis et al. [16] introduced about TPA, and several studies reported it is related with clinical outcomes of patients’ mechanical complication after ASD surgery [12,16,20,21,34]. TPA is similar to the spinopelvic angle, allows the patient to check thoracolumbar alignment well, and is not affected by changes in the patient’s posture, so it can be evaluated objectively. It can be assumed that there may be a downside to being difficult to know exactly in terms of the ability to stand in the Dubousset’s conus of economy. In our study, the normality of TPA was related to the normal value of the spinopelvic parameter after surgery, and was related to the pain parameters. The sagittal spinopelvic parameters were related with chronic back pain and/or HRQoL [34-36]. It can be seen that this contributed to the improvement of back pain by sufficiently making lordosis through correction of the sagittal imbalance. TPA has a certain value even in the stooping posture of the patient because the alignment of cervical spine and the horizontal gaze of the patient are missing. There was no research on whether these differences were related to the prediction of mechanical complications. In postoperative stooping posture related with global imbalance of the patient after ASD surgery, it may be due to pain, and there may be various reasons. Such as, PJK, DJK, pain, insufficient decompression. If the patient’s global balance cannot be maintained due to various reasons, assuming that the OD-HA angle might come out poorly and TPA remains constant, we studied whether this difference is different in the prediction of the patient’s postoperative prognosis, that is, the mechanical complication. Results in our paper, OD-HA angle showed better results.
In several studies have reported that spinopelvic fixation affects the occurrence of PJK. In several studies reported SPF with iliac screws had high rates of lumbosacral fusion and low incidence of mechanical complications and revision surgery for PJK [37] and reduced sacroiliac joint pain after multisegment spinal fusion after SPF with S2 alar iliac screws [38]. Otherwise, some studies reported although the rigid SPF has decreased the risk for distal screw loosening, cyclic loading during daily activities might lead to fatigue of the posterior instrumentation, which can result in mechanical long-term complications such as nonunion and eventually increase the risk of iliac screw loosening, development of PJK, PJF, and pseudarthrosis or pedicle screw loosening at L5–S1 level [10,39,40]. In our study, statistical significance was not observed, but there was a force to SPF was related with development of mechanical complication especially PJK/PJF.
Also, many articles reported that older age, osteoporosis, and obesity are important risk factors of mechanical complication, PJK, and PJF. Lau et al. [32] demonstrated that age was an important risk factor of PJK and PJF. And high BMI was related with worse sagittal alignment after ASD surgery and worse postoperative scores in HRQoL, and development of PJK [10,20,41]. And osteoporosis was related with PJK and PJF [10,11,20]. Especially, Yagi et al. [11] reported low BMD (T score < -1.5) was a significant risk factor for the incidence of PJF. In our study, older age was related with occurrence of mechanical complication, BMD was related with all types of complications, and BMI was related with occurrence of mechanical complication and PJK. Sexual difference was not related with occurrence of complications. In radiological assessments, postoperative SVA was related with occurrence of mechanical complication and PJK. The other postoperative sagittal parameters were not related with complications. And UIV and LIV were similar between the 2 groups as T11–12 and L5–S1. In SPF, there is no significant difference between the 2 groups, but it shows approaching an acceptable significance level. The results of our study were also similar to previous other studies (Table 5).
The present study had several limitations. Because this was not a randomized and prospective study, but rather retrospective in design, a control population that received standard conservative care was not included. In addition, we did not control for selected surgical method or the period of preoperative conservative management. Meanwhile, the clinical score was not an absolute result because it was entirely patent specific. The images of the patients were measured by whole spine x-ray. Due to this, there may be some correction by the patient’s position. Finally, the results of this study may be limited because it was conducted only in a single country and a single institution. Further studies are needed with multicenter, multinational, and multiracial data for more reliable results in the future.
CONCLUSION
The goal of ASD surgery is to improve patient life quality through correction. In our study, TPA was associated with spinopelvic parameter and clinical parameters related with pain, OD-HA angle was associated with clinical parameters with functional impairment and complications. OD-HA angle is predictable factor for mechanical complications after ASD surgery.
Notes
The authors have nothing to disclose.