Redundant Nerve Roots of Cauda Equina Mimicking Intradural Disc Herniation: A Case Report
Article information
Abstract
Redundant Nerve Roots (RNRs) is an uncommon clinical condition characterized by a tortuous, serpentine, large and elongated nerve root of the cauda equina. To our knowledge, most cases of RNRs are associated with lumbar stenosis, and RNRs associated with lumbar disc herniation has not been reported until now.
Here we present a rare case of unusual RNRs associated with lumbar disc herniation mimicking intradural disc herniation.
INTRODUCTION
RNRs of the cauda equina were first described by Verbiest14) in 1954, and subsequently named by Cressman and Paul1) in 1968. RNRs is characterized by a tortuous, serpentine, large and elongated nerve root of the cauda equina10). It has been reported that RNRs develop as a response to lumbar spinal stenosis3,7,10). To our knowledge, most RNRs are associated with lumbar spinal stenosis, and the RNRs associated with lumbar disc herniation has not been reported until now.
Therefore, we present a rare case of unusual RNRs associated with lumbar disc herniation mimicking intradural disc herniation on magnetic resonance imaging study.
CASE REPORT
A 50-year-old man who worked at a rice-cake shop has suffered from increasing low back pain and radiating pain on his left leg for five years. He had a nerve root block on L5 level five years ago, and the pain subsided temporarily. He was having conservative treatment but mild chronic pain still lasted and gradually aggravated and abruptly extended to the right leg a few days before his admission. Radiating pain was on posterior and lateral aspect of the leg and toe.
He had no significant medical history or trauma history of spine. But he has been lifting heavy things repeatedly at work. A neurological examination revealed no paresthesia or motor weakness. A straight leg raise test was positive on the left side and the bilateral knee and ankle jerk was normal. Micturition and defecation were not disturbed.
Sagittal and axial T2-weighted magnetic resonance image reveals broad base central disc protrusion at L4-5 level, and about 0.7×0.5×2.5 cm sized ovoid nonenhancing lesion in dorsal aspect of L5-S1, which seemed to be intradural disc herniation rather than intradural mass (Fig. 1). Although the image clearly demonstrated neither the classical ring enhancement of the intradural fragments on gadolinium contrast MRI or discontinuity of the PLL disrupted at the disc level, this finding was thought as an intradural disc herniation rather than an intradural extramedullary (IDEM) tumor such as meningioma. CT myelography showed central disc herniation at L4-5 and intradural lesion looked like intradural disc or intradural mass within the thecal sac below L4/5 (Fig. 2).
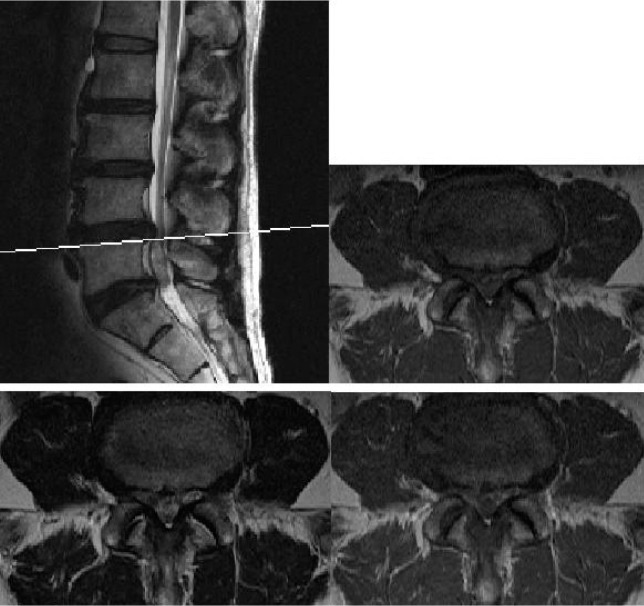
Sagittal and axial T2-weighted magnetic resonance image reveals broad base central disc protrusion at the L4-5 level, and about 0.7×0.5×2.5 cm sized ovoid nonenhancing lesion in dorsal aspect of L5-S1, which seems probably intradural disc herniation rather than intradural mass.

Preoperative CT myelography shows central disc herniation at L4-5 and intradural lesion looked like intradural disc or intradural mass within the thecal sac below L4/5.
A decompressive laminectomy was carried out at L4-5 levels and a herniated disc at L4-5 was removed. And we found the fragments of ruptured disc and adhesion with the dura. To determine whether there was a coexisting intradural disc rupture, we carried out an intradural exploration. After durotomy, a long, edematous and tortuous nerve root had forced out through a dural incision (Fig. 3). We explored the thecal sac, but there was no other intradural abnormality such as intradural disc herniation or intradural mass.

Intraoperative dorsal view of the elongated, edematous nerve root of the cauda equina. A non-pulsatile dural sac suddenly extruded through the dural incision as if it was squeezed from a tube of toothpaste.
After rearrangement of RNRs of the cauda equina to be released from the tangled position, the dura was carefully closed without tension.
The radiating pain was improved immediately in the postoperative period. The patient made an uneventful recovery and returned to normal activities. One year after surgery, he had no further pain.
DISCUSSION
The RNRs of the cauda equina has been discussed sporadically in both the neurological and radiological literature. Characteristically, the patients are men in their 4th to 6th decade, and the L3 to S1 nerve roots are most commonly involved4).
RNRs are relatively common finding in association with spinal stenosis5). RNRs were found in 42.3% of the patients with severe dural constriction and were seen on 8.2% of cadavers of aged people in autopsy10). Low back pain, lumbar radiculopathy, and intermittent claudication are common presenting features3). Associated bladder and sexual dysfunction can also occur3,6). The disorder is usually found in older patients and the onset of symptoms exhibits a long period10).
The cause of RNRs is unknown and is a matter of controversy. It was once presumed to be a rare congenital anomaly. Patients with achondroplasia may have RNRs8). Some authors suggested that congenitally long nerve roots in a narrow canal create a block1,8). There are a few cases associated with the presence of an arachnoid cyst9,11). There are many reports on the relationship between RNRs and constriction of the spinal canal and the most substantial mechanism seems to be an acquired elongation of nerve roots due to mechanical trapping at the site of spinal stenosis2,3,4,10,13,14). The inhibition of normal sliding and mobility causes repeated stretching of the nerves, leading to elongation above the level of constriction. When positional changes (e.g., flexion) cause a cephalic pull on the nerve roots, they are caught at the constriction and are unable to slide through. This repeated stretch causes elongation of the roots above the block. When the nerve roots are relieved, the elongated segments relax and pile up in redundant loops above the block2). Different from many cases of RNRs presenting above the stenosis, redundant nerve roots were below L4/5 level that had a broad base central disc protrusion in our case. The pathogenic mechanism seems to be different from the RNRs associated with spinal stenosis. We suppose that disc protrusion had an effect on the thecal sac and caused the RNRs. But, it is still a question why the RNRs developed below the block, and not above, and there is lack of sufficient analysis about the RNRs developed below the block in the previous study.
The importance of recognizing RNRs is to avoid misdiagnosis. In previous reports of RNRs, the evaluations were mainly based on myelographic findings. Though the appearance of serpiginous filling defects can be helpful in differentiating from other causes, it can also cause confusion occasionally, so it must be differentiated from vascular lesions such as arteriovenous malformation or dilated tortuous veins due to other causes2,3). Arteriovenous malformations can also produce serpiginous filling defects, but usually are not associated with extradural blocks. They, usually thoracic in location, show no variability with positional change and often have large feeding vessels2,9). Venous engorgement resulting from impaired venous drainage secondary to a block produces filling defects below the block. Also, the positional changes seen with redundant roots should not occur2,6,12).
RNRs could also be diagnosed on sagittal T2-weighted MR images. In general, the positive rate of RNRs examined by the MR imaging was as high as 97.6% when the nerve roots appeared as loop-shaped lesion on myelograms, whereas the positive rate was only 23.5% when the nerve roots appeared as serpentine-shaped lesions. According to the previous study, Magnetic resonance imaging appeared to demonstrate more advanced RNRs, and therefore MR imaging features of the RNRs are thought to represent important clinical findings7).
Unfortunately, MR imaging of the present case didn't show definite features of usual RNRs in spinal stenosis and it was not enough to exclude intradural herniation or intradural mass. Untypically, the RNRs looked like intradural mass such as IDEM tumor, but the lesion was not enhanced unlike intradural mass. The RNRs had similar signal intensity to the cauda equina on both T1 and T2-weighted images but on enhanced images, it is observed as a non-enhancing lesion protruding on intradural space of L4-5. In addition, there was disc protrusion on L4/5 accompanied by non-enhanced intradural lesion just below L4/5.
Also, CT myelography showed central disc herniation at L4/5 and intradural lesion looking like intradural disc or intradural mass within the thecal sac below L4/5. It is possible to mistake the intradural lesion as the downward migrating intradural ruptured disc, so we performed the intradural exploration to confirm. To avoid misdiagnosis and unnecessary procedure, careful analysis and wide experiences are needed.
Early and sufficient decompressive laminectomy with duroplasty is recommended to relieve the nerve root compression before neurological deficits appear3,6). Relief of RNRs at an early stage is strongly recommended. Patients with severe dural constriction caused by lumbar spinal stenosis should be treated surgically before the nerve roots undergo irreversible damage10) and intradural exploration should be considered where there still exists a question of tumor or AVM.
CONCLUSION
We experienced untypical RNRs and the RNRs with lumbar disc herniation could have been misdiagnosed as the intradural disc herniation before operation. To avoid misdiagnosis, it needs to be notice that lumbar disc herniation could be causative of RNRs. So we report a rare case of RNRs associated with lumbar disc herniation mimicking intradural disc herniation.