 |
 |
- Search
| Neurospine > Volume 18(4); 2021 > Article |
|
|
See commentary "Double Dome Laminoplasty: Works Well but There Are Exceptions" in Volume 18 on page 889.
Abstract
Objective
To introduce a new surgical technique - double dome laminoplasty for decompression of the entire C2 lamina and preservation of an extensor muscle insertion.
Methods
Eleven consecutive cervical myelopathy patients due to ossification of the posterior longitudinal ligament involving the Axis (C2) area were contained at this study. Direct decompression was evaluated as an increasing rate in space available cord (%) and posterior cord shift (mm) at C2 level. The Japanese Orthopaedic Association (JOA) score, visual analogue scale, and C2–7 Cobb angle in a neutral lateral x-ray were analyzed.
Results
The mean increase in space available for spinal cord at the C2 level, average posterior cord shift, and JOA recovery rate were 69.7%, 5.3±0.15 mm, and 58.0%, respectively. Cervical lordotic angle was maintained in all patients. One patient reported neck pain (visual analogue scale 6) postoperatively. No specific complications such as C2 laminar fracture or insufficient decompression were observed.
Ossification of the posterior longitudinal ligament (OPLL) is a representative disease that compresses the spinal cord and causes cervical myelopathy. If the patient develops neurological symptoms, surgical treatment should be considered first [1,2]. Most OPLL appear downwards, including C2, but it sometimes appears upward from C2 because posterior longitudinal ligament originates from the tectorial membrane [2-4]. If it develops in the caudal area of C2, dome laminoplasty of C2 could be a good option; however, it requires an even cranial area behind dens, and adequate decompression technique has not yet been developed. Furthermore, the destruction of the semispinalis cervicis (SSC) insertion during laminoplasty of the conventional C2 cranial area is unavoidable because most of the SSC muscles are attached to C2 spinous process [5-11]. Therefore, many patients complain of neck pain after this conventional laminoplasty and also, decrease in the range of neck motion [12,13]. Therefore, SSC insertion into the caudal half of C2 should be preserved to minimize axial pain and loss of lordosis. A technique for splitting laminoplasty of C2 has been developed to prevent these complications; however, splitting laminoplasty of C2 also increases the excursion of semispinalis, which results in muscle weakness.
To reduce these complains and to achieve effective direct decompression, we developed a new surgical technique – C2 double dome laminoplasty. The basic concept of thus surgical method is that it can widen the spinal canal very appropriately by a posterior approach and preserve the SSC muscle in order to decrease axial neck pain and maintain the neck lordosis.
The purpose of this study is to evaluate the technical feasibility, efficiency, and safety of this surgical procedure.
This study was approved by the Institutional Review Board of Asan Medical Center (AMC 2020-1410). All cases were performed by a single operating surgeon and were studied retrospectively. Eleven cervical myelopathy patients (female:male, 5:6) who underwent C2 double dome laminoplasty between March 2016 and March 2018 at our institution were included. The including criteria were follows: (1) cervical myelopathy patients with symptoms such as gait disturbance, hand clumsiness, and so on; (2) those who underwent C2 double dome laminoplasty due to OPLL involving the C2 cranial area; and (3) 24 months or longer follow-up period. Excluding criteria are as follows: revision operation, infection patients, cervical spondylosis radiculopathy, and so on. The pre- and postoperative clinical neurologic status of all cases were measured by the Japanese Orthopaedic Association for cervical myelopathy (C-JOA) score, and the recovery rate, using the Hirabayashi method: (postoperative score–preoperative score)× 100/(17–preoperative score). Axial neck pain was assessed according to the visual analogue scale (VAS). And all patients were checked radiographically with cervical spine x-ray at 3 months, 6 months, 1 year, and 2 years after surgery. Computed tomography (CT) scan and magnetic resonance images were conducted for all patients at 1 and 2 years after operation.
Radiologic parameter of the C2–7 Cobb angle was measured by the angle between the lower end- plates of C2 and C7 in the cervical spine via a neutral lateral x-ray of the patient. Decompression was evaluated as an increase in space available for spinal cord (SAC) at the C2 level via a midsagittal CT scan. Preoperatively, the spinal canal dimension of the midsagittal C2 vertebral body level (Y) and the spinal cord dimension (X) at the corresponding level were determined after the surgery. An increasing rate of SAC (%) was calculated as (Y–X)× 100/Y (Fig. 1). Posterior cord shift (mm) was evaluated according to the average anterior cord space of the C2 level on a midsagittal magnetic resonance image. The distance of the posterior cord shift was measured as the distance from the posterior edge of the C2 OPLL to the posterior edge of the spinal cord. Initially was measured by magnetic resonance imaging before and approximately 1 year and 2 years after the surgery.
Patients were placed in the standard prone position. Through the posterior midline approach, the SSC insertion at the caudal half of the C2 lamina was minimally detached and conventional dome-like laminoplasty was performed first by using a high-speed burr. Then, the rectus capitis posterior major and obliques capitis inferior were partially detached from the cranial one-third of the C2 lamina, and another dome-like laminoplasty was performed downwards (Fig. 1). All procedures were performed safely under a microscope. After confirming that the fenestration tunnel was made underneath the entire C2 lamina, all the detached muscles were repaired meticulously (Fig. 2). And additionally, we provided meticulously repairing the muscles such as rectus capitis posterior major and obliques capitis inferior, located in the proximal portion of the C2 spinous process, which play an important role as the secondary stabilizer of neck and head extension for maintaining the muscles as much as possible and reducing neck pain. So, these muscles were performed tight and layer by layer sutures. And simultaneously, we tried to keep the anatomy of each muscle as much as possible around C2 area. Finally, we confirmed that the surgical site was well decompression through the 3-dimensional CT scan after operation (Fig. 3).
Data management and statistical analyses were conducted using the Wilcoxon signed-rank test for continuous variables and discrete variables via the IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Significance was set at p<0.05. The distributions of variables are presented as means and standard deviations.
The clinical and radiologic data of the 11 patients who underwent C2 double dome laminoplasty are listed in Table 1. For this study, we enrolled 5 women and 6 men with a mean age of 61.3±6.5 years. The average follow-up period was 34.3±7.1 months.
The mean C-JOA score improved from 12.0±1.4 preoperatively to 14.9±1.9 at the final follow-up (p=0.015). The mean recovery rate of the C-JOA score at the final follow-up was 58.0%±10.8%, and there was no neurologic deficit in all cases after the surgery. The axial neck pain VAS scores did not significantly differ before and after the operation. Only one patient reported persistent axial neck pain (VAS score of 6) at the final follow-up.
As an indicator of C2 decompression, the mean SAC improved from 6.7±1.3 mm preoperatively to 15.2±2.4 mm at the final follow-up (p<0.001). The mean increase in SAC at the C2 level was 69.7% (Fig. 4). Furthermore, the average posterior cord shift statistically improved from 3.3±1.1 mm preoperatively to 8.7±1.2 mm at the final follow-up (p<0.001). The average posterior cord shift was 5.3±0.2 mm (Fig. 5). Neck alignment was well-maintained in all cases after the operation.
No specific complications, such as C2 laminar fracture or insufficient decompression, were observed. Furthermore, no perioperative complications were observed.
Cervical spine laminoplasty surgery is accepted as a safe and effective surgery for cervical myelopathy patients [14,15]. However, the following complications - decreased range of motion, loss of cervical spine lordotic angle, and the axial neck pain that occur after laminoplasty surgery have often been a problem [16-18]. Interlaminar fusion and radiologic change have been reported after surgery [18,19]. And in particular, neck pain is often complained of due to disruption of the posterior neck deep muscle including the SSC [20,21]. In particular, SSC is attached to C2 spinous process and acts as a dynamic stabilizer [22]. And this muscle acts as the most powerful extensor in the cervical spine [23,24]. However, in order to perform surgery using the conventional laminoplasty technique such as C2 laminoplasty or multilevel laminoplasty including C3, at least some of the SSC attached to C2 spinous process has to be removed. Of course, we would suture the SSC to the C2 spinous process again after surgery, but it might be difficult to restore it to the original state before surgery. Iizuka et al. [23] researched the condition of the SSC muscle using magnetic resonance image after conventional laminoplasty and reported that only approximately 18% of the SSC is maintained after surgery even if we tight repair the SSC muscle to the C2 spinous process. Therefore, many methods have been introduced to effectively decompress cervical spine without damaging not only the SSC but also the multifidus muscles [20,25,26].
Above mentioned, to overcome several complications of conventional laminoplasty and decompress the spinal cord of cervical spine, we developed a new and safe method for C2 area – C2 Double dome laminoplasty. Lee et al. [27] show that emergency reoperation was needed in patients that underwent the incomplete C2 dome shape one directional decompression surgery. However, in this study, we confirmed that cord compression of the C2 area by OPLL was effectively decompressed by double dome laminoplasty. The improvement of SAC and posterior cord shift were statistically significant compared with that before and after the surgery. The mean SAC improved from 6.7±1.3 mm to 15.2±2.4 mm at the final follow-up (p<0.001). The average increasing SAC value at C2 was 69.7%. Furthermore, the average posterior cord shift significantly improved from 3.3±1.1 mm to 8.7±1.2 mm at the final follow-up (p<0.001), and the average posterior cord shift was 5.3±0.2 mm.
The changes were also related to clinical outcome, as demonstrated by the significant improvements in C-JOA scores (from 12.0±1.4 to 14.9±1.9; mean recovery rate, 58.0%±10.8%). A high C-JOA score means that the quality of life and function are improved, and appropriate decompression surgery is correlated with a high C-JOA score [28]. Therefore, C2 double dome laminoplasty can be considered as an effective technique for decompression of the C2 area.
The most important concept of this technique is to reduce axial neck pain after surgery by taking an approach without damaging the SSC muscle. In particular, SSC of the posterior cervical muscle acts as a dynamic stabilizer, and the most powerful extensor in the cervical spine so maintain the neck alignment and lordotic angle [29,30]. Anatomically, the SSC originates from the upper thoracic transverse process and inserts to C2 spinous process. So that tis the main part among the posterior cervical spine muscles. Vasavada et al. [31] reported that SSC provides powerful extension moment-generating quantity. Therefore, we performed a tight suture in order to completely restore the SSC after laminoplasty surgery. However, if the SSC cannot return as completely as it was before surgery, then we should avoid damaging it as much as possible. Thus, the preservation of SSC muscles is associated with a reduction in axial neck pain, which prevents deterioration in the patient’s quality of life due to postoperative neck pain. In addition, we provided meticulously repairing the muscles such as rectus capitis posterior major and obliques capitis inferior, located in the proximal portion of the C2 spinous process, which play an important role as the secondary stabilizer of neck and head extension for maintaining the muscles as much as possible and reducing neck pain.
Qi et al. [28] demonstrated that the group that underwent cervical deep muscle preserving laminoplasty showed better results in cervical spine function than the group that received conventional laminoplasty. Another study reported that among these extensor muscles, SSC, in particular, acts as a key muscle in maintaining neck function and neck alignment [32]. This effort to preserve the cervical deep extensor muscle preserves blood flow to that muscle and maintains the muscle volume, so prevents atrophy of the theses muscle as well as surrounding ligaments contracture. And this procedure would make decrease the patient’s complications and increase the function of the neck. And the patient’s quick recovery can be expected even after muscle preserving laminoplasty technique. And therefore, the recovery of muscle control is promoted [28]. Furthermore, in this study, there was almost no difference in neck pain before and after surgery, and cervical lordosis was well-maintained. However, in one case, the patient experienced an increase in neck pain at the final follow-up, which may have been due to the additional detachment of the SSC during the initial steps of this technique.
C2 double dome laminoplasty is a safe and useful technique for patients with cervical myelopathy due to C2 OPLL. However, the surgeon should check whether there is any anatomical variation in the surrounding the structure when performing this operation. Therefore, we recommend that you check the surgical site through CT scan and magnetic resonance image before surgery.
We recommend double dome laminoplasty for treating patients with cervical myelopathy, especially involving the C2 area. And we believe that this surgical technique can not only avoid C2 laminectomy, but also decrease the neck pain and maintain the cervical alignment, which surgeon wanted to overcome in the conventional laminoplasty. Furthermore, this new technique is a safe and effective way to decompress the spinal canal in the cervical area. Double dome laminoplasty might be a widely used method without complications for C2 decompression surgery.
SUPPLEMENTARY MATERIALS
Supplementary video clip can be found via https://doi.org/10.14245/ns.2143028.514.
Fig. 1.
Diagram of C2 double dome osteotomy. (A) There is the diffuse OPLL (black star) at C2 level, preoperatively. The 2 dotted lines indicate the part where osteotomy will be performed using high-speed burr. (B) This is the diagram after surgery with double dome osteotomy is performed, the enlarged spinal canal can be observed (Y). The spinal canal dimension of the midsagittal C2 vertebral body level (Y) and the spinal cord dimension (X) at the corresponding level were determined after the surgery. An increasing rate of SAC (%) was calculated as (Y–X) × 100/Y. OPLL, ossification of the posterior longitudinal ligament; SAC, space available for spinal cord.
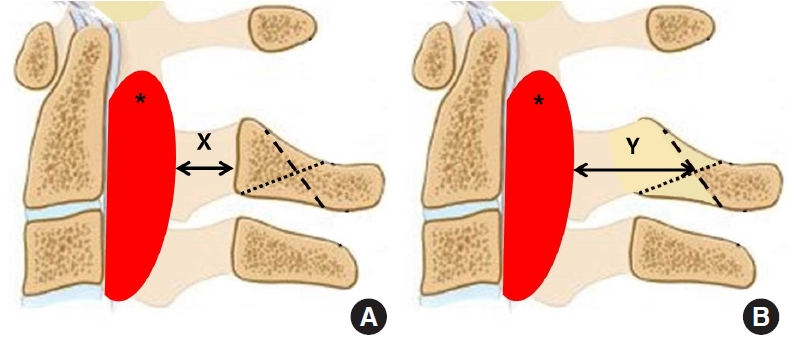
Fig. 2.
These serial photos were taken during surgery through a microscope. In each medical photos, the top is the cranial side and the bottom is the caudal side. (A) And C2 spinous process indicates the white star. Through the posterior midline approach, the semispinalis cervicis (black star) insertion at the caudal half of the C2 lamina was minimally detached and the rectus capitis posterior major (white arrowheads) and obliques capitis inferior (black arrowhead) were partially detached from the cranial one-third of the C2 lamina. (B) For fenestrating tunnel which is made underneath the entire C2 lamina, we confirmed safely using by the penfield.
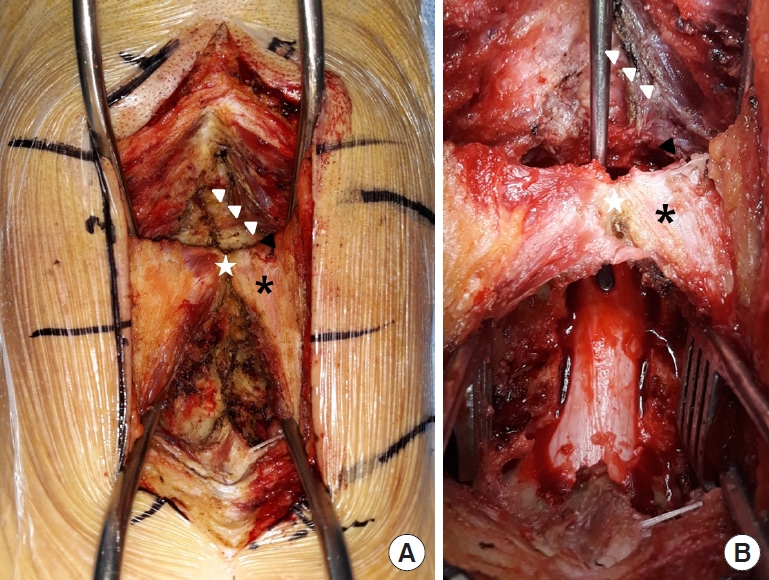
Fig. 3.
Preoperative and postoperative 3-dimensional (3D) reconstruction computerd tomography (CT) images. (A) This 3D CT image shows a well of the patient’s bone structure, preoperatively. (B) Postoperative 3D CT image which was taken postoperative 2 years shows definitely decompression at the C2 area through the double dome laminoplasty. And patient underwent the partial laminectomy of C3 and conventional laminoplsty of C4 and C5 for additional decompression.
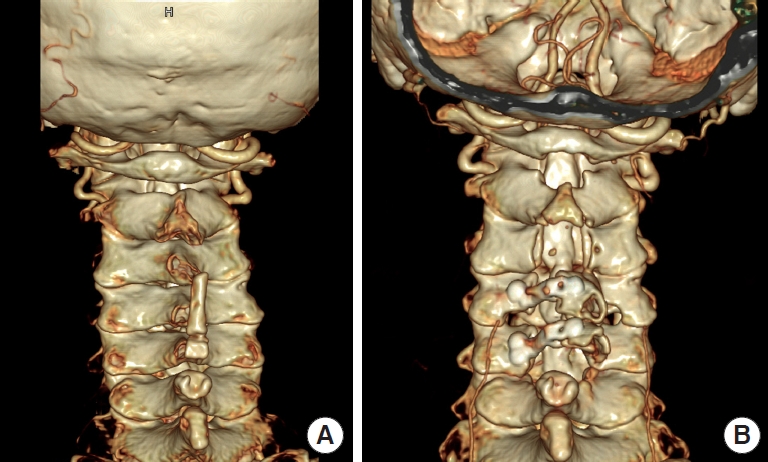
Fig. 4.
Preoperative and postoperative sagittal/axial computed tomography (CT) images. (A, C) Preoperative image demonstrates severe spinal canal stenosis due to huge OPLL at C2 level. And red dotted line represents cranial cutting line, also yellow dotted line represents caudal cutting line. (B, D) This CT image which was taken postoperative 2 years shows definitely decompression at the same area. Spinal canal diameter indicates the white line with both arrows. OPLL, ossification of the posterior longitudinal ligament.
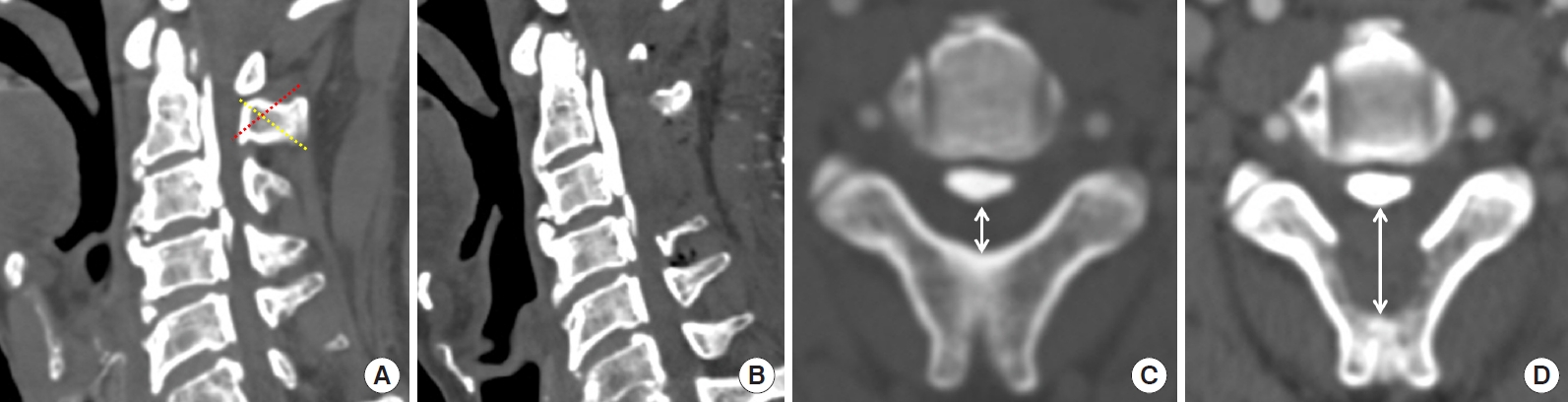
Fig. 5.
Magnetic resonance sagittal image before and after surgery. (A) The preoperative magnetic resonance image shows that the spinal cord is severely compressed due to C2 OPLL (white arrow). (B) This magnetic resonance image was taken postoperative 2 years. In this image, C2 double dome osteotomy was performed, resulting in sufficient decompression of the spinal canal at the same level (white arrow). OPLL, ossification of the posterior longitudinal ligament.
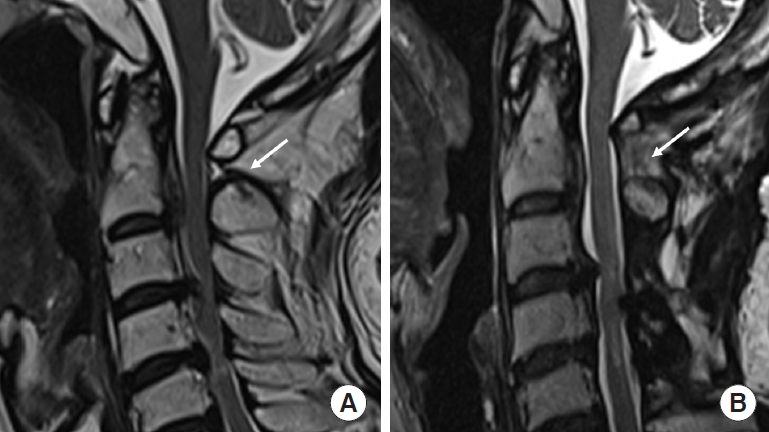
Table 1.
Clinical data and surgical outcomes of all patients
| Age (yr)/sex | F/U (mo) | Increasing rate of SAC (%) | Posterior cord shift (mm) |
C-JOA score |
VAS |
C2–7 Lordosis* |
|||
|---|---|---|---|---|---|---|---|---|---|
| Pre-OP | Post-OP | Pre-OP | Post-OP | Pre-OP | Post-OP | ||||
| 51/M | 46 | 71.1 | 5.3 | 11 | 13 | 2 | 2 | -8 | -9 |
| 55/F | 44 | 68.4 | 5.2 | 14 | 17 | 2 | 6 | -10 | -10 |
| 60/M | 40 | 69.6 | 5.3 | 11 | 14 | 2 | 2 | -11 | -10 |
| 57/M | 37 | 69.3 | 5.6 | 10 | 13 | 3 | 3 | -11 | -10 |
| 63/F | 36 | 70.1 | 5.1 | 12 | 14 | 3 | 3 | -13 | -12 |
| 59/M | 34 | 68.5 | 5.2 | 13 | 17 | 2 | 1 | -11 | -11 |
| 73/F | 31 | 70.2 | 5.1 | 13 | 16 | 2 | 2 | -15 | -14 |
| 61/M | 31 | 70.6 | 5.4 | 10 | 13 | 2 | 2 | -12 | -11 |
| 69/F | 30 | 69.8 | 5.3 | 14 | 17 | 1 | 1 | -14 | -13 |
| 64/F | 25 | 68.8 | 5.4 | 13 | 17 | 1 | 1 | -9 | -9 |
| 68/M | 24 | 70.5 | 5.4 | 11 | 13 | 2 | 2 | -13 | -13 |
REFERENCES
1. Stapleton CJ, Pham MH, Attenello FJ, et al. Ossification of the posterior longitudinal ligament: genetics and pathophysiology. Neurosurg Focus 2011 30:E6.

2. Choi SH, Kang CN. Degenerative cervical myelopathy: pathophysiology and current treatment strategies. Asian Spine J 2020 14:710-20.



3. Saetia K, Cho D, Lee S, et al. Ossification of the posterior longitudinal ligament: a review. Neurosurg Focus 2011 30:E1.

4. Lee SE, Jahng TA, Kim HJ. Surgical outcomes of the ossification of the posterior longitudinal ligament according to the involvement of the C2 segment. World Neurosurg 2016 90:51-7.


5. Matsuzaki H, Hoshino M, Kiuchi T, et al. Dome-like expansive laminoplasty for the second cervical vertebra. Spine 1989 14:1198-203.


6. Matsunaga S, Nakamura K, Seichi A, et al. Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine 2008 33:2648-50.


7. Odate S, Shikata J, Soeda T, et al. Surgical results and complications of anterior decompression and fusion as a revision surgery after initial posterior surgery for cervical myelopathy due to ossification of the posterior longitudinal ligament. J Neurosurg Spine 2017 26:466-73.


8. Kim GU, Chang MC, Kim TU, et al. Diagnostic modality in spine disease: a review. Asian Spine J 2020 14:910-20.



9. Seng C, Tow BP, Siddiqui MA, et al. Surgically treated cervical myelopathy: a functional outcome comparison study between multilevel anterior cervical decompression fusion with instrumentation and posterior laminoplasty. Spine J 2013 13:723-31.


10. Lin S, Zhou F, Sun Y, et al. The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J 2015 24:127-35.


11. Kiyoshi T, Ko I, Keiichiro I, et al. Radiographic and clinical results of C1 laminoplasty for the treatment of compressive myelopathy. Asian Spine J 2020 14:459-65.



12. Liu J, Ebraheim NA, Sanford CG Jr, et al. Preservation of the spinous process-ligament-muscle complex to prevent kyphotic deformity following laminoplasty. Spine J 2007 7:159-64.


13. Bu G, Shuang F, Liu G, et al. Efficacy and safety of one-stage selective discectomy combined with expansive hemilaminectomy in the treatment of cervical spondylotic myelopathy. World Neurosurg 2016 94:507-12.


14. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine 1988 13:870-6.


15. Kawaguchi Y, Kanamori M, Ishihara H, et al. Minimum 10-year follow up after en bloc cervical laminoplasty. Clin Orthop Relat Res 2003 411:129-39.

16. Kimura I, Shingu H, Nasu Y. Long-term follow-up of cervical spondylotic myelopathy treated by canal-expansive laminoplasty. J Bone Joint Surg Br 1995 77:956-61.


17. Sasai K, Saito T, Akagi S, et al. Cervical curvature after laminoplasty for spondylotic myelopathy-involvement of yellow ligament, semispinalis cervicis muscle, and nuchal ligament. J Spinal Disord 2000 13:26-30.


18. Seichi A, Takeshita K, Ohishi I, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 2001 26:479-87.


19. Iizuka H, Iizuka Y, Nakagawa Y, et al. Interlaminar bony fusion after cervical laminoplasty: its characteristics and relationship with clinical results. Spine 2006 31:644-7.


20. Shiraishi T, Fukuda K, Yato Y, et al. Results of skip laminectomy-minimum 2-year follow-up study compared with open-door laminoplasty. Spine 2003 28:2667-72.


21. Takeshita K, Seichi A, Akune T, et al. Can laminoplasty maintain the cervical alignment even when the C2 lamina is contained? Spine 2005 30:1294-8.


22. Nolan JP Jr, Sherk HH. Biomechanical evaluation of the extensor musculature of the cervical spine. Spine 1988 13:9-11.


23. Iizuka H, Shimizu T, Tateno K, et al. Extensor musculature of the cervical spine after laminoplasty: morphologic evaluation by coronal view of the magnetic resonance image. Spine 2001 26:2220-6.


24. Conley MS, Meyer RA, Bloomberg JJ, et al. Noninvasive analysis of human neck muscle function. Spine 1995 20:2505-12.


25. Shiraishi T. Skip laminectomy - a new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: a preliminary report. Spine J 2002 2:108-15.

26. Otani K, Sato K, Yabuki S, et al. A segmental partial laminectomy for cervical spondylotic myelopathy: anatomical basis and clinical outcome in comparison with expansive open-door laminoplasty. Spine 2009 34:268-73.


27. Lee BJ, Lee SB, Jeon SR, et al. A new indicator predicting the degree of cord shift after posterior decompression of cervical ossification of the posterior longitudinal ligament extended to the C2 level and its clinical usefulness. Turk Neurosurg 2021 31:866-72.


28. Qi Q, Chen Y, Ling Z, et al. Modified laminoplasty preserving the posterior deep extensor insertion into C2 improves clinical and radiologic results compared with conventional laminoplasty: a meta-analysis. World Neurosurg 2018 111:157-65.


29. Esmende SM, Daniels AH, Paller DJ, et al. Cervical total disc replacement exhibits similar stiffness to intact cervical functional spinal units tested on a dynamic pendulum testing system. Spine J 2015 15:162-7.


30. Miyamoto S, Yonenobu K, Ono K. Experimental cervical spondylosis in the mouse. Spine 1991 16(10 Suppl):S495-500.






























