Discal Cyst of the Lumbar Spine: A Case Report
Article information
Abstract
Discal cysts are a rare cause of lumbar radiculopathy. There are only a few reports of this disease in medical literature. The authors describe the case of a 40-year-old man with a lumbar discal cyst that led to radiculopathy. An intraspinal extradural cystic mass was responsible for low and high signal intensities observed in lumbar lesions on T1 and T2 weighted magnetic resonance images. This cyst was a grossly spherical mass with clear serous fluid, which was connected to an adjacent intervertebral disc. Histopathology of the cystic walls revealed fibrous connective tissues without specific cell linings. Clinical symptoms were promptly relieved after surgical resection. Further research on the pathophysiology and treatment of discal cysts are needed.
INTRODUCTION
Debilitating conditions, such as disc herniation or lumbar spinal stenosis, are one of the most common causes of lumbago and lumbar radiculopathy. It may be easily recognized by their clinical symptoms and signs. Magnetic resonance imaging (MRI) helps establish a definitive diagnosis. Nevertheless, there are uncommon causes of lumbago or radiculopathy, which include intraspinal extradural masses, such as synovial cyst, ganglion cyst, pseudocyst, hematoma and metastatic tumor, as well as arachnoid cysts. On the basis of clinical examination and history taking, these uncommon causes are generally difficult to distinguish from those that are more common. Of these uncommon causes, intraspinal extradural cysts that communicate with the intervertebral discs are quite rare. This is a case report of a lumbar discal cyst in a patient with low back pain and pain that radiates to the legs.
CASE REPORT
A 40-year-old man disclosed a 6-months history of aggravated lumbago and pain that radiated to the left buttock and the leg. The patient also had complaint of numbness and tingling sensations below the knee. However, there was no history of trauma or constitutional symptoms. On examination, he showed paravertebral tenderness in the lower lumbar spine with lumbar motion limitation secondary to pain. A neurologic examination was remarkable for a grade 3/5 dorsiflexion weakness in his left ankle. His extensor hallucis longus showed a grade 4/5 dorsiflexion weakness. Otherwise, motor examinations of the remaining muscles were within normal levels.
He had sensory abnormalities on the L4 dermatome area of the left leg. The straight leg raising test on the left was positive at an angle of 45 degrees (45°). There were no bladder or bowel disturbances. The VAS score of lumbago was 4 (pain was scored on a VAS from 0=no pain to 10=strongest pain imaginable) and that of radiating pain was 8. Lumbar radiography showed a minimal degenerative change. An MRI scan revealed a disc extrusion at L3/4 and a large spherical lesion behind the L4 vertebral body. A mass lesion revealed a low signal intensity on T1-weighted image and high signal intensity on T2-weighted images, which were located in the left ventromedial aspect of the extradural space at the L4 body level, compressing the thecal sac and left L4 nerve root dorsally (Fig. 1). There was a central disc bulging with a ligamentum flavum thickening at the L4/5 intervertebral disc levels, while a narrowing was detected at the left L4/5 intervertebral foramen. Based on further enhanced imaging studies, the cystic mass was well enhanced and seemed to be connected like a stalk between the L3/4 intervertebral disc spaces.

Magnetic resonance imaging scan. (A) The mass lesion (white arrow) was revealed low signal intensity on T1-weighted image. (B) High signal intensity on T2 weighted images. (C) and (D) The cystic mass is well enhanced marginally, seemed to be connected between intervertebral disc on the enhancing imaging scan (black arrow: channel-like connection with adjacent intervertebral disc).
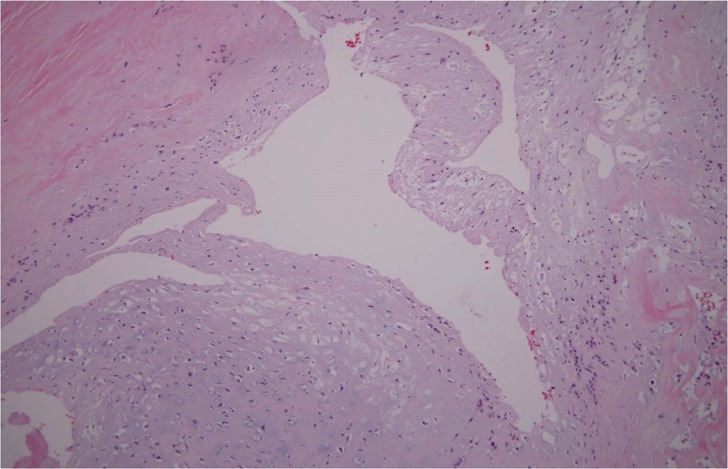
The EMG(Electromyography)/NCV(Nerve conduction velocity) was consistent with left L4 radiculopathy. This patient unsuccessfully underwent a conservative treatment with rest, NSAIDs (Non-Steroridal Anti-Inflammatory Drugs) and an epidural steroid injection at a local clinic. Owing to worsening of sensory and motor abnormalities in the lower extremities, surgery was indicated. A left partial laminectomy was performed at L4 (due to the location of a mass lesion behind the L4 body). A darkish red cyst was seen underneath the left L4 nerve root, compressing the thecal sac and displacing the left L4 nerve root dorsally. A meticulous dissection was necessary for the severe adhesions between the cystic mass and nerve root as well as dura mater (Fig. 2). Grossly, the cystic mass was round and 1.2×1.1 cm in size. Serous hemorrhagic fluid was aspirated with a 22-gauge syringe and sent for both pathologic study and culture (Fig. 3). After removal of the cyst, the channel-like soft tissues adjoining the intervetebral disc were identified and cauterized. Then, disectomy was performed at L3/L4. Histologically, the cyst walls were constituted with dense fibrous connective tissues without cell linings or disc materials. (Fig. 4) Cultures of the cystic hemorrhagic fluid were negative. The patient's radicular pain resolved promptly after surgery and only slight numbness overlying his left anterior thigh was reported during the follow-up observation period of two (2) years.

On operative field, a yellowish cystic mass (black arrow) was seen underneath the left L4 nerve root (white arrow) compressing the thecal sac, and displacing the left L4 nerve root dorsally.

The cystic mass (cutting image) was a grossly round, 1.2×1.1 cm in size. Serous hemorrhagic fluid was aspirated with a 22-gauge syringe.
DISCUSSION
Intraspinal extradural masses causing lumbago or lumbar radiculopathy are uncommon. Many articles have been reported about intraspinal extradural masses such as synovial cysts, ganglion cyst, perineural cyst, chordoma and metastatic tumor. Among them, intraspinal cystic mass originating from an adjacent intervertebral disc is very rare. The first case was reported in 19999). Less than one hundred (100) case reports and small case series for discal cysts have been published to date1,10). The majority of discal cyst cases were seen in the young Asian population1). The fact that discal cysts may be present in the absence of additional spinal pathology and most commonly affect young males may be distinctive characteristics that are different from other degenerative conditions.
Several pathogeneses may be suggested, such as degenerative changes due to previous herniated disc material, hematoma associated with a disc herniation, and mucoid degeneration. However, the etiology for discal cysts is debatable. Kono et al. mentioned that the pathogenesis of discal cysts is similar to that of meniscal cysts of the knee and synovial cysts of the facet joint9). Based on this hypothesis, focal degeneration of the intervertebral disc may lead to leakage of fluid into the spinal canal producing an inflammatory reaction. This causes a formation of the pseudomembrane around the fluid. Chiba et al. proposed that discal cysts would arise from hemorrhage of an epidural venous plexus due to mechanical forces transmitted by a herniated annular fissure2). Marshman et al. suggested that discal cysts were similar to ganglion cysts of the posterior longitudinal ligament or annulus fibrosus12).
The clinical symptoms and signs of discal cysts resemble those found in patients with a lumbar disc herniation. Plain radiographs have a low diagnostic value except for identifying other conditions, such as degenerative spondylolisthesis and spondylosis. However MR imaging can be used to identify discal cysts accurately2,5,8,12). MR Imaging demonstrates the nature of the cystic lesion and its relationship to the corresponding disc. Like a normal intervertebral disc, a discal cyst reveals a low signal on T1-weighted imaging and a high signal on T2-wighted imaging. In addition, the surrounding rim and contents of a cyst may show enhancement in a contrast enhanced MRI. These MR imaging characteristics are the keys to differentiating discal cysts from lumbar disc herniation11). Further diagnostic evaluation for a suspected discal cyst may include discography and CT discography13). CT-discography was not incorporated owing to the possibility of aggravating the patient's motor weakness, which could be provoked by contrast media. Preoperative MRI findings demonstrated adequate information for discal cyst. Moreover, it was possible to confirm the connection between the corresponding disc and cyst intraoperatively. The natural history of the discal cyst is still unknown and therapeutic guidelines have not been established. Spontaneous regression of a discal cyst has been reported4,14), as well as regression after intradiscal and epidural steroid injections8). However, the management of a discal cyst is similar to that of a lumbar herniation6). An initial nonoperative treatment is reasonable for neurologically-intact patients. CT-guided percutaneous aspiration can be considered as another initial treatment option for a discal cyst, because it has several potential advantages, including faster recovery, low complication rates and avoidance of general anesthesia3,7,8). Surgical resection of a discal cyst is reserved for patients with persistent symptoms. In this case study, conservative treatment was not effective for several months. This patient's symptoms totally resolved after surgical excision and he remained nearly asymptomatic postoperatively for two years and thereafter.
CONCLUSION
Intervertebral discal cysts are exceedingly rare. They should remain in the differential diagnosis of any intraspinal extradural mass lesion compressing the thecal sac and nerve root. MR imaging helps to confirm the diagnosis, while surgical excision of a cyst should be considered for persistently symptomatic patients.