 |
 |
- Search
|
|
||
Abstract
Objective
Diseases of the craniovertebral junction (CVJ) are commonly associated with deformity, malalignment, and subsequent myelopathy. The misaligned CVJ might cause compression of neuronal tissues and subsequently clinical symptoms. The triangular area (TA), measured by magnetic resonance imaging/images (MRI/s), is a novel measurement for quantification of the severity of compression to the brain stem. This study aimed to assess the normal and pathological values of TA by a comparison of patients with CVJ disease to age- and sex-matched controls. Moreover, postoperative TAs were correlated with outcomes.
Methods
Consecutive patients who underwent surgery for CVJ disease were included for comparison to an age- and sex-matched cohort of normal CVJ persons as controls. The demographics, perioperative information, and pre- and postoperative 2-year cervical MRIs were collected for analysis. Cervical TAs were measured and compared.
Results
A total of 201 patients, all of whom had pre- or postoperative MRI, were analyzed. The TA of the CVJ deformity group was larger than the healthy control group (1.62 ± 0.57 cm2 vs. 1.01 ± 0.18 cm2, p < 0.001). Moreover, patients who had combined anterior odontoidectomy and posterior laminectomy with fixation had the greatest reduction in the TA (1.18 ± 0.58 cm2).
The craniovertebral junction (CVJ) resides between the cranium and cervical spine. Its unique structure is responsible for important functions, including head movement and protection of the nervous system [1,2]. The CVJ is composed of bony structures, ligaments and joints, including atlas, axis, transverse ligament, cruciate ligament, occipital-atlantal joint and atlantoaxial joint [3-5]. Together, these structures not only maintain the stability of the CVJ, but also are involved in the axial rotation and flexion-extension movements.
Although deformity around the CVJ is a rare condition, there are several pathologies that could affect the CVJ, such as congenital anomaly, trauma, autoimmune disease, primary or metastatic bone tumor, and ossification of the posterior longitudinal ligament (OPLL) [6-10]. These CVJ diseases consequently result in CVJ instability and alignment change. The deformed CVJ could cause significant neck pain due to arthritis or C2 foraminal stenosis and cervicomedullary compressive myelopathy [11-14].
There have been numerous diagnostic criteria for CVJ disease. However, most of the current radiographic parameters are specific for the diagnosis of certain CVJ diseases. For example, the measurement of the atlanto-dental interval was used for the diagnosis of atlantoaxial subluxation [15,16]. Meanwhile, those parameters are based on fluoroscopic examination, such that soft tissue compression cannot be appreciated in those exams. The triangular area (TA) of the CVJ, proposed by Chang et al. [17] in 2016, is a novel measurement that can quantify the degree of compression that is applied on patients with basilar invagination. The measurement of the TA is defined by the area determined by 3 points in the midsagittal magnetic resonance T2-weighted image: the lowest point of the clivus, the posterior-inferior point of the C2 vertebral body, and the most dorsal indentation point in the ventral aspect of the brain stem (Fig. 1). The application of TA was further expanded to patients with CVJ trauma and rheumatoid arthritis. Chang et al. [18] reported that patient with a TA value greater than 1.36 cm2 had high possibility to develop myelopathy that early surgical intervention was highly recommended.
Surgery of CVJ pathology can be difficult and complicated. Several aspects should be of concern before the surgery. First, the anatomy of the CVJ area is usually intricate. Bony or vascular anomalies are not uncommon in patients with CVJ disease [1,19-21]. Second, the alignment correction has a great influence on the surgical outcome. A realigned CVJ indicates the relief of cervicomedullary compressive myelopathy [22]. However, alignment correction is not always achievable in every patient with CVJ deformity. Third, a decompression maneuver, either anterior, posterior or combined, should be considered in those patients who had failed realignment of the CVJ [23,24]. Although there have been several algorithms proposed to treat CVJ deformity, there is still debate on the choice of decompression maneuver in CVJ deformity patients, and there is no definite conclusion till now. In most cases, the choice of decompression method is dependent on the surgeon’s experience. The use of the TA could quantify the degree of ventral compression to the brain stem including medulla. Therefore, it could represent clinical improvement. Using the TA might provide a useful indication to determine the way of decompression in the future. In this study, we aimed to expand the use of TA to various kinds of CVJ pathology. Comparisons were made against age- and sex-matched population-based controls without CVJ deformity. Postoperative TAs were also measured and compared according to different decompression maneuvers.
This was a retrospective comparative study that included consecutive patients who had CVJ surgery for instability. Patients who had the diagnosis of CVJ pathologies were extracted from the database for analysis. The other age- and sex-matched cohort members who had a normal CVJ (no structural CVJ anomalies on the MRI, and had an atlantodental interval less than 3 mm on the dynamic lateral radiographs) were extracted from the image data base within the same period as the CVJ deformity group. The study was approved by the Institutional Review Board of Taipei Veterans General Hospital (No. 2019-12-001AC) and patients’ informed consent was obtained.
Exclusion criteria were prior surgery of the CVJ and those patients who had an unidentified TA due to bony destruction. The TA measurements were performed on the Smart Iris Imaging System (Taiwan Electronic Data Processing Co., Taipei City, Taiwan), and interpreted independently by radiologists and neurosurgeons, who were blinded to the patient information. Data were collected and compared between the groups. Patients of the CVJ deformity group were followed-up regularly and MRI was arranged at 2-year postoperation. The demographic and perioperative data were also collected for comparison.
A simulated TA ventral to the brain stem was determined in the midsagittal T2-weighted MRIs of each patient on the picture archiving and communication system and calculated by its viewer. The TA was defined by 3 points: the lowest point of the clivus, the posterior-inferior point of the C-2 vertebral body, and the most dorsal indentation point in the ventral aspect of the brain stem. For the surgical cases, the pre- and postoperative 2-year TA was measured and compared [17,18].
Medcalc (Ostend, Belgium) was used for statistical analysis. Descriptive statistics were reported as means and standard deviations, and as frequencies and percentages where appropriate. Continuous variables were compared using an unpaired Student t-test, and categorical variables were compared using Pearson chi-square test. Probability values were 2-tailed and an alpha of 0.05 was considered statistically significant.
A total of 201 consecutive patients who had CVJ deformity were included in this study. Another 201 age- and sex-matched persons were included as controls. There were 101 male and 100 female patients in both groups. The mean age was, respectively, 59.8± 17.2 versus 60.2± 13.1, p= 0.78. The body mass index in the CVJ deformity group was smaller (23.5± 3.6 vs. 24.7 ± 4.9, p = 0.014). The incidence rate of hypertension was 38.8% versus 30.8%, p= 0.09, type II diabetes mellitus 13.4% versus 15.4%, p = 0.57, and ankylosing spondylitis 1.9% versus 0.9%, p= 0.41. The incidence rate of rheumatoid arthritis was significantly higher in the CVJ deformity group (10.4% vs. 0.9%, p<0.0001) (Table 1).
The type of pathology and perioperative information were listed in Table 2. There were 10 patients who had C0–2 decompressive laminectomy, 27 patients who had C1 laminectomy, and 39 patients who had C1–2 laminectomy. A total of 8 patients received anterior odontoidectomy, including 6 odontoidectomy before fusion and 2 odontoidectomy after fusion surgery. There were 142 patients who had fusion level within C1–2 and 59 patients who had fusion level spanning C1–2. The average bone density (DEXA T-score) of the CVJ deformity group was -1.39± 1.68. There were 12 patients who experienced surgical complication, including 5 cerebrospinal fluid leak, 6 wound infection/poor healing, and 1 postoperative cerebellar infarction. There was no vascular injury among all surgical cases (Table 2).
The control group had an average TA of 1.01± 0.18 cm2. The average TA of the CVJ deformity group was 1.62± 0.57, which was significantly larger than the control group. The TAs of patients with basilar invagination, odontoid fracture, os odontoideum, stenosis, atlantoaxial subluxation, C2 osteomyelitis, and C2 metastasis were significantly larger than in the control group (Table 3).
The delta TA (ΔTA) was the difference between the preoperative and postoperative 2-year TA. The ΔTA in patients who had combined anterior and posterior decompression surgery was -1.18± 0.58. The ΔTA in patients who had no decompression maneuver (fixation-alone) was -0.20 ± 0.37. The ΔTA in patients who had posterior decompression (decompressive laminectomy plus fixation) was -0.21± 0.49 (Table 4).
The cervical TA of the CVJ deformity group was significantly larger than the age- and sex-matched control group (1.62± 0.57 vs. 1.01± 0.18, p< 0.001). Furthermore, this study expanded the use of TA to various kinds of CVJ pathology. The TA in most of the CVJ pathology group was significantly larger than the TA in the control group except for several pathologies, such as aneurysmal bone cyst (ABC), combined C1 and C2 fracture, hangman fracture, OPLL and C2 multiple myeloma. Those images were reviewed to discuss why the TA did not increase in those patients. The ABC was a benign, blood-filled vascular lesion in the bone that tends to expand or grow. In our case, the ABC occurred within the C2 laminar, spinous process and bilateral pars interarticularis that caused the destruction of the bilateral atlantoaxial joint. However, the ventral side was totally free of ABC. Therefore, the TA in our ABC case was normal since it did not have any ventral compression. In combined C1 and C2 fracture and hangman fracture cases, we found the CVJs were reduced during the MRI examination that made the TA value normal. The C2 multiple myeloma was diagnosed at a very early stage, such that the destruction and deformation of the CVJ was not severe. The TA value of 3 OPLL cases were similar to the control group. That was because the OPLL started from the middle of C2, which did not cause a lot of ventral compression.
The measurement of the TA could quantify the degree of cervicomedullary compression in patients with a CVJ deformity. After the surgery, the change of the TA could reflect the efficacy of surgery. The improvement of the TA benefits from 3 factors; the improvement of alignment, the decompression effect, and the resorption of retro-odontoid soft tissue mass. The realignment and decompression immediately influences the TA after surgery. The resorption of retro-odontoid soft tissue mass was a delayed type of TA improvement. It has been well reported by many researchers that the retro-odontoid mass tissue disappeared after fixation of the CVJ [14,17,18,25].
Chang et al. [17] observed that the TA decreased immediately after the surgery and continued to decrease until 2 years after surgery. In this study, the ΔTA was 1.18 cm2 in patients who had combined anterior and posterior decompression surgery. Furthermore, the ΔTA was similar between the posterior decompression group and the group without decompression. This result was quite intuitive that the TA represented the ventral compression to the spinal cord. The measurement of the TA could not depict the outcome of posterior decompression.
The CVJ diseases are usually associated with structural destruction that results in CVJ instability and deformation. The malaligned CVJ causes cervicomedullary compression, so that surgical intervention was necessary to prevent brain stem or spinal cord injury. For optimal treatment, surgeons should consider the etiology, reducibility of bony parts, mechanics of compression, and the presence of an abnormal ossification center. Menezes proposed a treatment algorithm for CVJ abnormality with the primary goal to relieve compression at the CVJ [24]. For reducible lesions, the treatment key point is to maintain a neutral position and stabilization, either by external immobilization or internal fixation. Irreducible lesions require decompression at the side at which the compressions occur. The treatment algorithm was straightforward and convincing, which was supported by many published clinical series [2,7,23,26-33]. However, the surgical decision was always difficult because the reducibility was difficult to judge, especially for those patients in an acute stage. Most patients in an acute stage were afraid of moving their head and neck due to severe neck pain and muscle spasm. The results of the TA change after surgery in this study might provide a useful information for the surgical planning in the future. As mentioned before, the improvement of the TA benefits from 3 factors: the improvement of alignment (Fig. 2A, B), the decompression effect (Fig. 2C, D), and the resorption of retro-odontoid soft tissue mass (Fig. 2E, F). In this study, we found the patients who had no decompression maneuver (fixation only) had a decrease of their TA by 0.2 cm2. The decrease of the TA in this patient group was mainly attributed to the improvement of alignment. Otherwise, the combined anterior and posterior decompression group had a decrease of the TA by 1.18 cm2. Our previous study demonstrated that a TA value greater than 1.36 cm2 was highly associated with myelopathy [18]. The combined conclusions of both studies suggested that anterior odontoidectomy should be highly considered for those patients who had a TA value greater than 2.5 cm2. Once the TA value was larger than 2.5 cm2, it was less likely to have a TA smaller than 1.36 cm2 via the posterior approach only, either with decompression or not. The use of the TA could provide useful information in surgical planning.
There were limitations to this study. This was a single institute, retrospective, nonrandomized, observational study. The age- and sex-matched control cohort was chosen from the patients who had cervical MRI in our image data base with no CVJ abnormality. These patients might not be completely healthy as they could have been slightly symptomatic or had other reasons for MRI examination. There was some heterogeneity in the CVJ deformity cohort; the case numbers of certain pathologies were fewer than others. This reflects the rarity of any particular disease. Otherwise, the TA was designed for quantification of the ventral compression. For the compression from the posterior side, it was unable to be detected. However, the TA is still a very useful measurement for the CVJ, given the reason that most CVJ deformity cases resulted in anterior subluxation. Future investigations should aim to expand its use in more CVJ deformity cases to help in the surgical decision and to evaluate the efficacy of surgery.
This case-control study has expanded the use of the TA to various kinds of CVJ pathologies. The TA was significantly larger in CVJ deformity cases compared with cases without deformity as controls. After surgery, the change of the TA could reflect the realignment and decompression effect of the CVJ. Therefore, the TA is a valid measurement to quantify compression at the CVJ and to evaluate the efficacy of surgery.
NOTES
Fig. 1.
Assessment of ventral compression of the craniovertebral junction (CVJ) by the simulated triangle on the midsagittal T2-weighted magnetic resonance image of the CVJ. The 3 points of the triangle are the lowest point of the clivus, the posterior-inferior point of the axial vertebral body, and the most indented point of the dura.

Fig. 2.
Pre- and postoperative 2-year (A, B) image of a patient with atlantoaxial subluxation. The TA decreased due to improvement in alignment. Pre- and postoperative 2-year (C, D) image of a patient with os odontoideum. The TA decrease benefitted from the anterior odontoidectomy. Pre- and postoperative 2-year (E, F) image of a patient with rheumatoid arthritis and atlantoaxial subluxation. The TA decrease was due to the disappearance of the retro-odontoid mass.
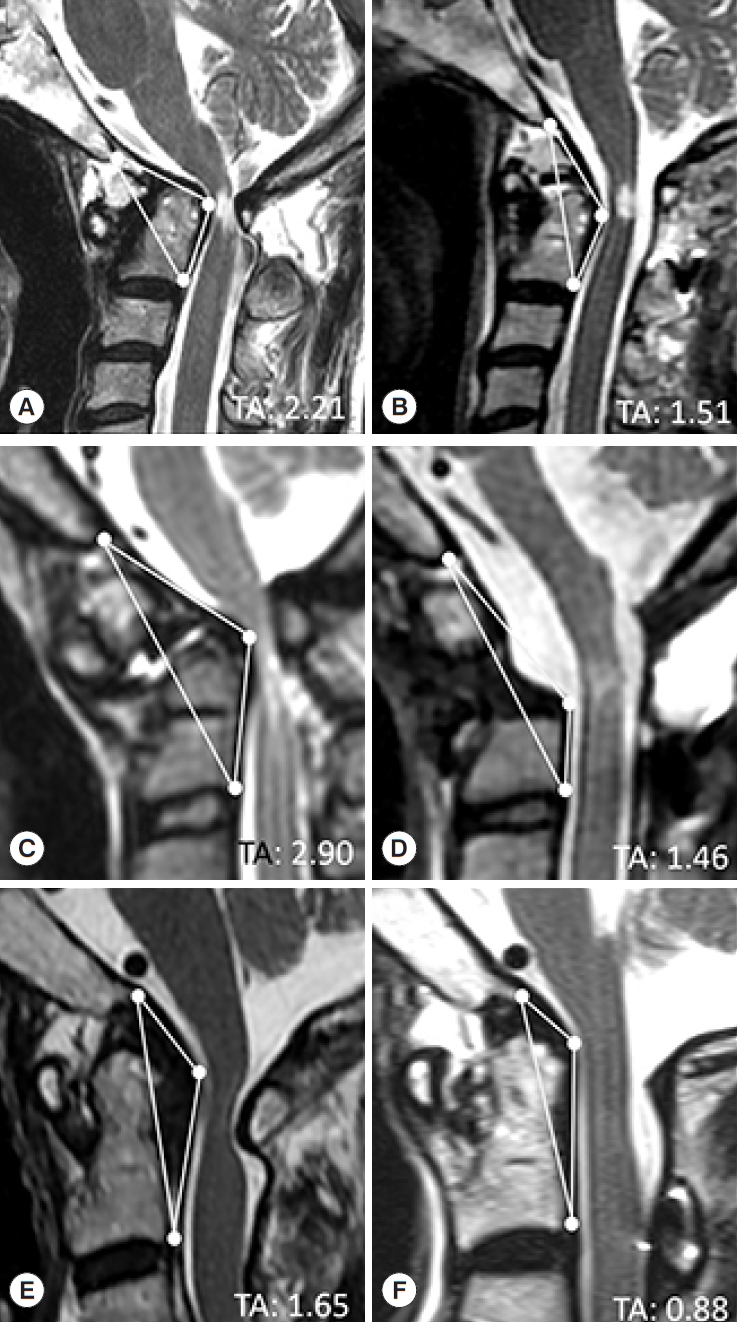
Table 1.
Comparison of clinical characteristics between craniovertebral junction (CVJ) deformity cases and age-sex-matched controls
| Characteristics | CVJ deformity (n = 201) | Controls (n = 201) | p-value |
|---|---|---|---|
| Sex | 1.00 | ||
| Male | 101 | 101 | |
| Female | 100 | 100 | |
| Age (yr) | 59.8 ± 17.2 | 60.2 ± 13.1 | 0.78 |
| Body mass index (kg/m2) | 23.5 ± 3.6 | 24.7 ± 4.9 | 0.014* |
| Comorbidity | |||
| Hypertension | 78 (38.8) | 62 (30.8) | 0.09 |
| Type II diabetes mellitus | 27 (13.4) | 31 (15.4) | 0.57 |
| Rheumatoid arthritis | 21 (10.4) | 2 (0.9) | < 0.001* |
| Ankylosing spondylitis | 4 (1.9) | 2 (0.9) | 0.41 |
Table 2.
Type of pathology and perioperative information
Table 3.
Comparison of preoperative triangular area between craniovertebral junction (CVJ) deformity cases and normal controls
| Variable | Preoperative triangular area (cm2) | p-value |
|---|---|---|
| Controls | 1.01 ± 0.18 | - |
| CVJ deformity | 1.62 ± 0.57 | < 0.001* |
| Aneurysmal bone cyst | 1.01 | - |
| Basilar invagination | 1.94 ± 0.48 | 0.02* |
| Combined C1 and C2 fracture | 1.07 | - |
| Jefferson fracture | 1.55 | - |
| Hangman fracture | 1.11 ± 0.27 | 0.13 |
| Odontoid fracture | 1.55 ± 0.56 | < 0.001* |
| Os odontoideum | 2.11 ± 0.62 | < 0.001* |
| Stenosis | 2.18 ± 0.45 | < 0.001* |
| Atlantoaxial subluxation | 1.63 ± 0.52 | < 0.001* |
| OPLL | 0.92 ± 0.12 | 0.39 |
| C2 osteomyelitis | 1.84 ± 0.68 | < 0.001* |
| C2 metastasis | 1.31 ± 0.41 | < 0.001* |
| C2 multiple myeloma | 1.18 | - |
Table 4.
Comparison of ΔTA between different decompression maneuvers
|
Decompression type |
|||
|---|---|---|---|
| Without decompression | Posterior decompression | Combined anterior and posterior decompression | |
| ΔTA (cm2) | -0.20 ± 0.37 | -0.21 ± 0.49 | -1.18 ± 0.58* |
REFERENCES
1. Lee DH, Hong JT, Sung JH, et al. Morphologic analysis of occipital sinuses for occipital screw fixation using digital subtraction angiography. World Neurosurg 2016;91:279-84.


2. Goel A, Sathe P, Shah A. Atlantoaxial fixation for basilar invagination without obvious atlantoaxial instability (Group B Basilar Invagination): outcome analysis of 63 surgically treated cases. World Neurosurg 2017;99:164-70.


3. Debernardi A, D’Aliberti G, Talamonti G, et al. The craniovertebral junction area and the role of the ligaments and membranes. Neurosurgery 2015;76 Suppl 1:S22-32.



4. Deepak AN, Salunke P, Sahoo SK, et al. Revisiting the differences between irreducible and reducible atlantoaxial dislocation in the era of direct posterior approach and C1-2 joint manipulation. J Neurosurg Spine 2017;26:331-40.


5. Yin YH, Tong HY, Qiao GY, et al. Posterior reduction of fixed atlantoaxial dislocation and basilar invagination by atlantoaxial facet joint release and fixation: a modified technique with 174 cases. Neurosurgery 2016;78:391-400. discussion 400.


6. Kukreja S, Ambekar S, Sin AH, et al. Occipitocervical fusion surgery: review of operative techniques and results. J Neurol Surg B Skull Base 2015;76:331-9.



7. Taggard DA, Menezes AH, Ryken TC. Instability of the craniovertebral junction and treatment outcomes in patients with Down’s syndrome. Neurosurg Focus 1999;6:E5.

8. Molliqaj G, Dammann P, Schaller K, et al. Management of craniovertebral junction tuberculosis presenting with atlantoaxial dislocation. Acta Neurochir Suppl 2019;125:337-44.


9. Moulding HD, Bilsky MH. Metastases to the craniovertebral junction. Neurosurgery 2010;66(3 Suppl):113-8.


10. Krauss WE, Bledsoe JM, Clarke MJ, et al. Rheumatoid arthritis of the craniovertebral junction. Neurosurgery 2010;66(3 Suppl):83-95.


11. Salunke P, Sahoo S, Deepak AN. Different facets in management of congenital atlantoaxial dislocation and basilar invagination. Neurosurgery 2015;77:E985-7.


12. Salunke P, Sahoo SK, Deepak AN, et al. Comprehensive drilling of the C1-2 facets to achieve direct posterior reduction in irreducible atlantoaxial dislocation. J Neurosurg Spine 2015;23:294-302.


13. Benglis D, Levi AD. Neurologic findings of craniovertebral junction disease. Neurosurgery 2010;66(3 Suppl):13-21.


14. Ferrante A, Ciccia F, Giammalva GR, et al. The craniovertebral junction in rheumatoid arthritis: state of the art. Acta Neurochir Suppl 2019;125:79-86.


15. Boden SD. Rheumatoid arthritis of the cervical spine. Surgical decision making based on predictors of paralysis and recovery. Spine (Phila Pa 1976) 1994;19:2275-80.


16. Boden SD, Dodge LD, Bohlman HH, et al. Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am 1993;75:1282-97.


17. Chang PY, Yen YS, Wu JC, et al. The importance of atlantoaxial fixation after odontoidectomy. J Neurosurg Spine 2016;24:300-8.


18. Chang CC, Wu CL, Tu TH, et al. Cranio-vertebral junction triangular area: quantification of brain stem compression by magnetic resonance images. Brain Sci 2021;11:64.



19. Salunke P, Futane S, Sahoo SK, et al. Operative nuances to safeguard anomalous vertebral artery without compromising the surgery for congenital atlantoaxial dislocation: untying a tough knot between vessel and bone. J Neurosurg Spine 2014;20:5-10.


20. Wakao N, Takeuchi M, Nishimura M, et al. Vertebral artery variations and osseous anomaly at the C1-2 level diagnosed by 3D CT angiography in normal subjects. Neuroradiology 2014;56:843-9.



21. Yamazaki M, Okawa A, Furuya T, et al. Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography: analysis of 100 consecutive surgical cases and review of the literature. Spine (Phila Pa 1976) 2012;37:E1389-97.


22. Chandra PS, Goyal N, Chauhan A, et al. The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Neurosurgery 2014;10 Suppl 4:621-9. discussion 9-30.


23. Hong JT, Kim IS, Lee HJ, et al. Evaluation and surgical planning for craniovertebral junction deformity. Neurospine 2020;17:554-67.




24. Menezes AH. Craniovertebral junction database analysis: incidence, classification, presentation, and treatment algorithms. Childs Nerv Syst 2008;24:1101-8.



25. Fiani B, Houston R, Siddiqi I, et al. Retro-odontoid pseudotumor formation in the context of various acquired and congenital pathologies of the craniovertebral junction and surgical techniques. Neurospine 2021;18:67-78.




27. Menezes AH. Craniovertebral junction abnormalities with hindbrain herniation and syringomyelia: regression of syringomyelia after removal of ventral craniovertebral junction compression. J Neurosurg 2012;116:301-9.


28. Menezes AH. Craniovertebral junction anomalies: diagnosis and management. Semin Pediatr Neurol 1997;4:209-23.


29. Menezes AH. Craniovertebral junction neoplasms in the pediatric population. Childs Nerv Syst 2008;24:1173-86.



30. Menezes AH, Traynelis VC, Gantz BJ. Surgical approaches to the craniovertebral junction. Clin Neurosurg 1994;41:187-203.

31. Dlouhy BJ, Policeni BA, Menezes AH. Reduction of atlantoaxial dislocation prevented by pathological position of the transverse ligament in fixed, irreducible os odontoideum: operative illustrations and radiographic correlates in 41 patients. J Neurosurg Spine 2017;27:20-8.






























