 |
 |
- Search
|
|
||
See commentary "Reply to Commentary on “Classification(s) of Cervical Deformity”" in Volume 20 on page 408.
See commentary "Commentary on “Classification(s) of Cervical Deformity”" in Volume 20 on page 405.
Abstract
Cervical spine deformities (CSD) are complex surgical issues with currently heterogenous management strategies. The classification of CSD is still an evolving field. Rudimentary classification schemas were initially proposed in the late 20th century but were largely informal and based on the underlying etiology (i.e. , postsurgical, traumatic, or inflammatory). The first formal classification schema was proposed by Ames et al. in 2015 who established a standard nomenclature for describing these deformities. This classification system established 5 deformity descriptors based on curve apex location (cervical, cervicothoracic, thoracic, craniovertebral junctional, and coronal deformities) and 5 deformity modifiers which helped surgeons utilize a standard language when discussing CSD patients. Koller et al. in 2019 subsequently established a classification system for patients with rigid cervical kyphosis based on regional and global sagittal alignment. Most recently, Kim et al. in 2020 proposed an updated classification system utilizing dynamic cervical spine imaging to guide surgical treatment of CSD patients. It identified 4 major groups of deformities – (1) those with “flat-neck” deformities caused by cervical lordosis T1 slope mismatch; (2) those with focal kyphotic deformities between 2 cervical vertebrae; (3) those with cervicothoracic deformities caused by large T1 slope; and (4) those with coronal deformities. Group 2 deformities most often required combined anterior-posterior approaches with short constructs, and group 3 deformities most often required posterior-only approaches with 3-column osteotomies.
Cervical spine deformities (CSD) can significantly hinder patient quality of life [1,2]. Despite the complex surgical management required, the rarity and relative paucity of data has resulted in heterogeneous management of patients with cervical deformities. Although other spinal deformities have benefitted from established classifications [3-7], the classification of CSD is an evolving field. Recent attempts at classifications of CSD by large multi-institution studies, are helping to guide surgical treatment of these complex deformity cases [8-10].
Given the relative rarity of CSD, there was sparse literature describing the management of these deformities throughout the 20th century. Much of the early literature regarding treatment of cervical deformities, however, described anecdotal management strategies for isolated types of secondary cervical deformity. These included traumatic [11,12], postlaminectomy [13-18], neuromuscular [19], and inflammatory [20,21]. Consequently, early attempts at classifying CSD were based entirely on the underlying etiology of the deformities, not radiographic characteristics or treatment. Yasuoka et al. [22] was among the first to explicitly classify cervical deformities as: congenital, neuromuscular, traumatic, oncologic, inflammatory, and idiopathic. This classification was proposed in the setting of creating exclusion criteria for their analysis of postlaminectomy cervical deformities. No treatment-guiding classification were proposed at this time.
The first codified classification system for CSD was published in 2015 by Ames et al. and the International Spine Study Group. The goal of this schema was to provide a unified nomenclature system for patients with CSD. This followed similar attempts to unify nomenclature for cervical spine osteotomies and soft tissue releases [23].
The Ames classification was created utilizing a modified Delphi panel of experts who identified pertinent classification criteria based on static radiographs [8]. Classification using the Ames schema requires full-length standing anteroposterior (AP) and lateral films of the spine and dedicated AP and lateral films of the cervical spine [24]. The Ames classification system consists of 5 deformity descriptors with 5 deformity modifiers (Fig. 1). Deformity descriptors included 3 sagittal deformity groups: “C” for curves with apex deformity in the cervical spine, “CT” for curves with apex deformity at the cervicothoracic junction, and “T” with apex deformities in the thoracic spine. The other 2 classifications were “S” for coronal deformities (defined as a C2–7 cobb angle of greater than or equal to 15 degrees), and “CVJ” for deformities primarily at the craniovertebral junction.
The 5 deformity modifiers included: (1) a sagittal vertical axis (SVA) modifier, measured by the difference in C2–7 SVA; (2) a horizontal gaze modifier, measured by the chin-brow vertical angle; (3) a cervical lordosis (CL) modifier, measured by T1 slope (T1S) subtracted by CL; (4) a myelopathy modifier using the modified Japanese Orthopedic Association scores [25]; and (5) a thoracolumbar spinal deformity modifier using the validated SRS-Schwab Classification Modifier [5]. The respective grading scales for each modifier can be seen in Fig. 1. The validation study for the Ames classification showed strong intraobserve reliability.
The Ames classification provided a unified nomenclature system for deformity surgeons to use when discussing patients, and improvement in the cervical modifiers of the Ames classification has been correlated with improved postoperative radiographic aligment [8,26,27]. This classification was not based on health-related quality of life metrics, however and the classification does not guide treatment [28]. Another limitation of this classification was that it relies exclusively on static radiographs. For management of CSD, dynamic radiographs are crucial to help determine the required number of osteotomies and soft tissue procedures needed for ultimate deformity correction and fusion [29-32].
Since the publication of the Ames criteria, several validations studies have demonstrated the correlation between advanced Ames deformity modifiers and progressive deformity [33-36]. Subsequent literature has also demonstrated the clinical importance of stratifying deformities by rigidity, achieving global sagittal balance with regional alignment, and correcting of cervical alignment in extension [32,37,38].
Building upon the unified nomenclature provided by the Ames Classification, Koller et al. [9] and the European Cervical Spine Research Society (ECSRS) established a treatment-guiding algorithm for patients with rigid cervical kyphosis (CK). In 2019, this research group conducted a 10-year, multicenter retrospective review of patients with rigid CK who underwent surgical correction. In this review, Koller-ECSRS classified patients into 4 deformity types based on regional and global alignment in patients: types A-D (Fig. 2). They subsequently described the surgical techniques most often used for correction of each deformity. Deformity type A corresponded to patients with cervical/cervicothoracic kyphosis with maintained global alignment. Type B corresponded to cervical/cervicothoracic kyphotic deformities with concomitant global imbalance. Type C corresponded to cervicothoracic kyphotic deformities with inadequate compensatory CL and persistent global imbalance. Type D corresponded to patients with appropriate CL and maintained global alignment. Koller et al. [9] found that this classification schema had clinical implications. Patients with type A deformities were significantly more likely to require a combined anterior/posterior surgical approach, while patients with type C deformities were more likely to undergo posterior-only correction. Type C deformities also required the highest-grade osteotomies for adequate deformity correction.
The Koller-ECSRS classification created a useful classification system for patients with rigid CK that emphasized regional and global alignment. Like the Ames classification, however, the Koller-ECSRS classification solely utilized static radiographs. Moreover, the Koller classification simply reported the most common surgical techniques utilized by their cohort of surgeons with limited discussion on the biomechanical reason for these strategies.
Given the Ames and Koller-ECSRS classifications’ reliance on static radiographs and limited ability to guide surgical correction, Kim et al. and the International Spine Group Study in 2020 published a new classification schema based on a multiinstitution 2-step cluster analysis study of patients with severe CSD. The Kim classification schema utilized dynamic cervical spine imaging to create a treatment-guiding classification schema for CSD [10]. Classification utilizing the Kim schema requires full-length standing AP and lateral spine radiographs and dedicated AP, lateral, flexion, and extension cervical spine radiographs. The Kim classification identified 4 distinct classes of CSD: (1) “flat-neck” deformities; (2) focal kyphotic deformities; (3) cervicothoracic deformities; and (4) coronal deformities (Fig. 3) [39]. Of note, coronal deformities were rare among the patient cohort and treatment recommendations were unable to be made [10,39].
To identify the structural etiology behind these CSD subtypes and recommend treatment options, the Kim classification validation study analyzed changes in T1S, C2–7 SVA, T1S-CL, and maximum kyphosis between neutral and extended neck lateral radiographs. This isolated the source of deformity in each group and allowed recommendations for necessary fusion levels (Table 1).
Regarding group 1 deformities, the Kim classification identified a mainly cervicothoracic curve was secondary to significant CL-T1S mismatch. Treatment for group 1 flat-neck deformities is heterogenous in terms of anterior versus posterior approach however these deformities most often require fusions from C2 to a high-thoracic lowest instrumented vertebrae (LIV).
Regarding group 2 deformities, the main driver was identified as focal kyphosis between 2 cervical vertebrae with overall maintained global alignment secondary to compensatory increases in T1S (> 22°). These patients often require combined anterior/posterior approaches, with shorter constructs confined to the cervical spine [10].
Regarding group 3 deformities, the main driver was identified as extremely large T1S (> 50°). Surgical treatment for these patients most often requires an isolated posterior approach with an extended constructs extending to a LIV in the midthoracic to high-lumbar region. These patients frequently require 3-column osteotomies for adequate deformity correction [10].
Given the rarity of CSD patients, classifications of these deformities are still evolving. Historical classifications of CSD focused on the etiologies of these conditions but did not provide much clinical insight. The first unified classification schema, the Ames classification, was created in 2015 which provided a unified nomenclature for describing CSD using static radiographs but did not provide treatment recommendations. The Koller-ECSRS classification subsequently utilized static radiographs to classify and guide treatment of CK based on regional and global sagittal alignment. More recently, the Kim classification was created utilizing dynamic cervical spine imaging to help guide CSD surgical planning.
NOTES
Fig. 1.
Ames Classification for cervical spine deformity – deformities broken down into 5 deformity descriptors with 5 subsequent modifiers to account for sagittal vertical axis, horizontal gaze, cervical lordosis (CL), myelopathy, and overall SRS-Schwab classification (T, thoracic; L, thoracolumbar/lumbar; D, double curve; N, no coronal curve) [8]. CBVA, chin-brow vertical angle; TS, T1 slope; mJOA, modified Japanese Orthopedic Association; PI, pelvic incidence; LL, lumbar lordosis.
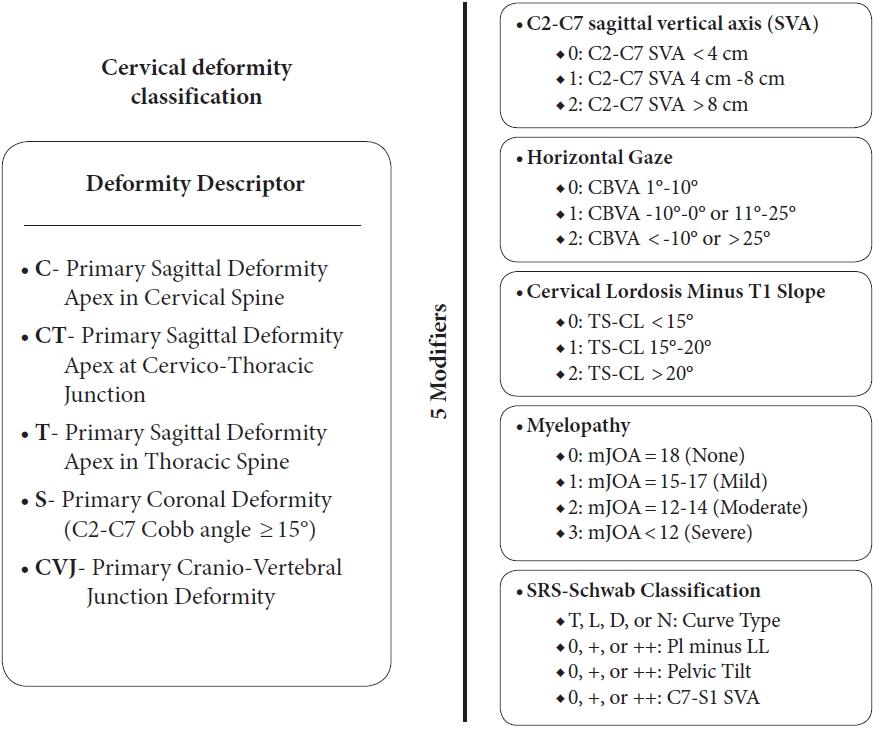
Fig. 2.
Figure demonstrating classifications of cervical sagittal balance types A-D (from left to right respectively) by Koller et al. and the European Cervical Spine Research Society [9]. SVA, sagittal vertical axis.
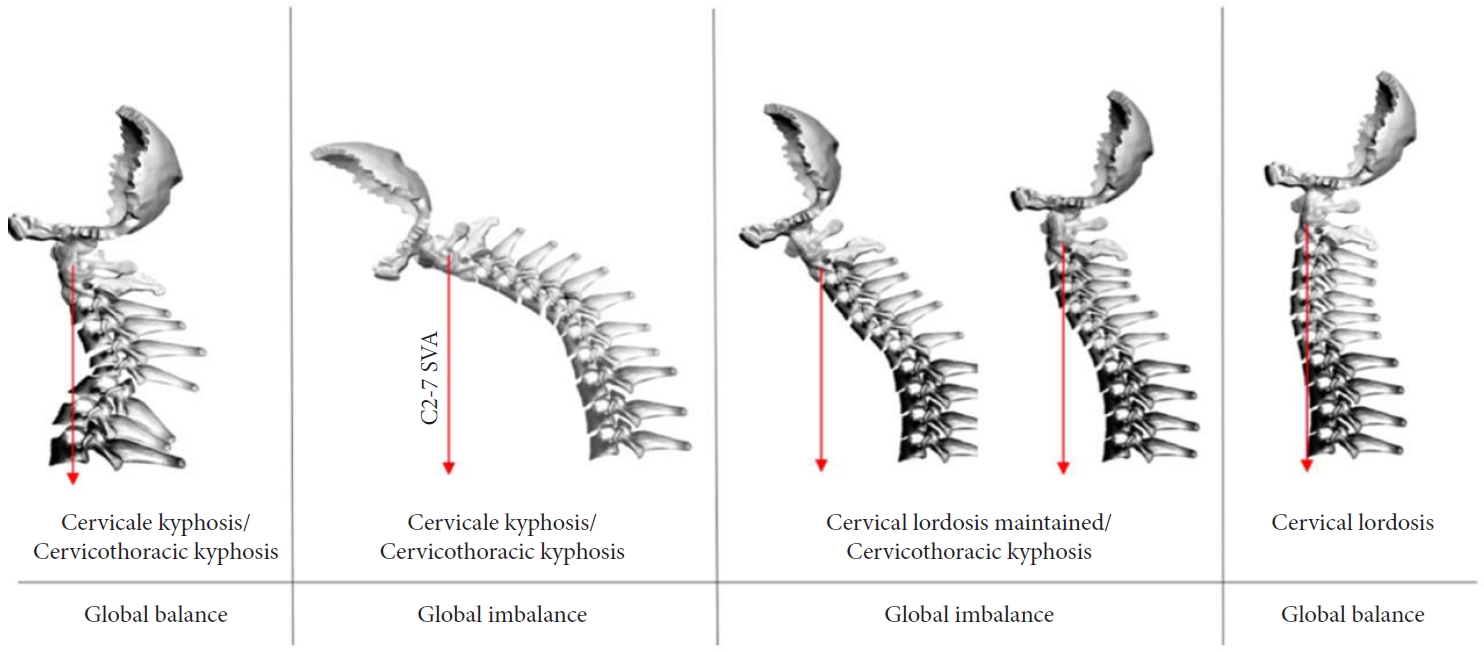
Fig. 3.
Three groups of sagittal deformities identified by Kim et al. [10] Dynamic images are utilized to identify the etiology of the deformity as well as plan surgical correction. “Ext” indicates extended neck lateral radiographs. Lat, lateral; Ext, extension; AP,
anteroposterior.
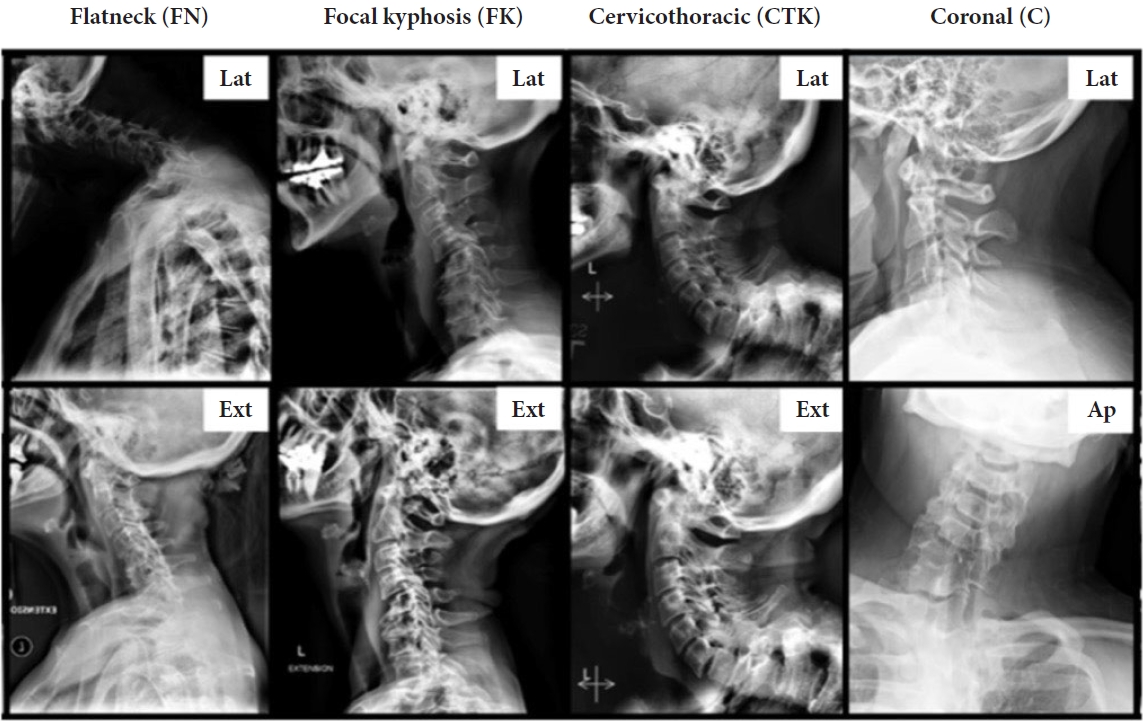
Table 1.
REFERENCES
1. Passias PG, Alas H, Bess S, et al. Patient-related and radiographic predictors of inferior health-related quality-of-life measures in adult patients with nonoperative spinal deformity. J Neurosurg Spine 2021 Apr 2:1-7. https://doi.org/10.3171/2020.9.SPINE20519. [Epub].

2. Smith JS, Shaffrey CI, Kim HJ, et al. Comparison of best versus worst clinical outcomes for adult cervical deformity surgery. Global Spine J 2019;9:303-14.




3. Lenke LG, Betz RR, Haher TR, et al. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine (Phila Pa 1976) 2001;26:2347-53.

4. Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83:1169-81.

5. Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 2012;37:1077-82.

6. Terran J, Schwab F, Shaffrey CI, et al. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 2013;73:559-68.

7. Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J 2011;20 Suppl 5(Suppl 5):641-6.




8. Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83.


9. Koller H, Ames C, Mehdian H, et al. Characteristics of deformity surgery in patients with severe and rigid cervical kyphosis (CK): results of the CSRS-Europe multi-centre study project. Eur Spine J 2019;28:324-44.



10. Kim HJ, Virk S, Elysee J, et al. The morphology of cervical deformities: a two-step cluster analysis to identify cervical deformity patterns. J Neurosurg Spine 2019 Nov 15:1-7. https://doi.org/10.3171/2019.9.SPINE19730. [Epub].

11. Roy-Camille R, Saillant G, Mazel C, et al. The surgical treatment of post-traumatic vertebral deformities. Ital J Orthop Traumatol 1986;12:419-26.

12. Stauffer ES, Rhoades ME. Surgical stabilization of the cervical spine after trauma. Arch Surg 1976;111:652-7.


13. Callahan RA, Johnson RM, Margolis RN, et al. Cervical facet fusion for control of instability following laminectomy. J Bone Joint Surg Am 1977;59:991-1002.


14. Cattell HS, Clark GL. Cervical kyphosis and instability following multiple laminectomies in children. J Bone Joint Surg Am 1967;49:713-20.


15. Shields CL, Stauffer ES. Late instability in cervical spine fractures secondary to laminectomy. Clin Orthop Relat Res 1976;(119):144-7.


17. Fairbank TJ. Spinal fusion after laminectomy for cervical myelopathy. Proc R Soc Med 1971;64:634-6.




18. Sim FH, Svien HJ, Bickel WH, et al. Swan-neck deformity following extensive cervical laminectomy. A review of twenty-one cases. J Bone Joint Surg Am 1974;56:564-80.

19. Simmons EH, Bradley DD. Neuro-myopathic flexion deformities of the cervical spine. Spine 1988;13:756-62.


20. Simmons EH. The surgical correction of flexion deformity of the cervical spine in ankylosing spondylitis. Clin Orthop Relat Res 1972;86:132-43.


21. Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop Relat Res 1977;(128):65-77.

22. Yasuoka S, Peterson HA, Laws ER, et al. Pathogenesis and prophylaxis of postlaminectomy deformity of the spine after multiple level laminectomy: difference between children and adults. Neurosurgery 1981;9:145-52.

23. Ames CP, Smith JS, Scheer JK, et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine 2013;19:269-78.

24. Cho SK, Safir S, Lombardi JM, et al. Cervical spine deformity: indications, considerations, and surgical outcomes. J Am Acad Orthop Surg 2019;27:e555-67.


25. Smith JS, Lafage V, Ryan DJ, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S161-70.

26. Passias PG, Jalai CM, Smith JS, et al. Characterizing adult cervical deformity and disability based on existing cervical and adult deformity classification schemes at presentation and following correction. Neurosurgery 2018;82:192-201.



27. Horn SR, Passias PG, Passfall L, et al. Improvement in some Ames-ISSG cervical deformity classification modifier grades may correlate with clinical improvement. J Clin Neurosci 2021;89:297-304.


28. Tan LA, Riew KD, Traynelis VC. Cervical spine deformityPart 1: biomechanics, radiographic parameters, and classification. Neurosurgery 2017;81:197-203.



29. Song KJ, Johnson JS, Choi BR, et al. Anterior fusion alone compared with combined anterior and posterior fusion for the treatment of degenerative cervical kyphosis. J Bone Joint Surg Br 2010;92:1548-52.



30. Mummaneni PV, Dhall SS, Rodts GE, et al. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine 2008;9:515-21.


31. O’Shaughnessy BA, Liu JC, Hsieh PC, et al. Surgical treatment of fixed cervical kyphosis with myelopathy. Spine (Phila Pa 1976) 2008;33:771-8.


32. Klineberg EO, Lafage R, Mundis GM, et al. 297. Preoperative extension lateral cervical radiographs are associated with osteotomy type, approach and postoperative cervical alignment following cervical deformity surgery. Spine J 2019;19(9 Suppl):S144-5.

33. Passias PG, Bortz C, Horn S, et al. Drivers of cervical deformity have a strong influence on achieving optimal radiographic and clinical outcomes at 1 year after cervical deformity surgery. World Neurosurg 2018;112:e61-8.


34. Hyun SJ, Han S, Kim KJ, et al. Assessment of T1 slope minus cervical lordosis and C2-7 sagittal vertical axis criteria of a cervical spine deformity classification system using longterm follow-up data after multilevel posterior cervical fusion surgery. Oper Neurosurg (Hagerstown) 2019;16:20-6.


35. Pierce KE, Passias PG, Brown AE, et al. Prioritization of realignment associated with superior clinical outcomes for cervical deformity patients. Neurospine 2021;18:506-14.




36. Bakouny Z, Khalil N, Otayek J, et al. Are the sagittal cervical radiographic modifiers of the Ames-ISSG classification specific to adult cervical deformity? J Neurosurg Spine 2018;29:483-90.


37. Sivaganesan A, Smith JS, Kim HJ. Cervical deformity: evaluation, classification, and surgical planning. Neurospine 2020;17:833-42.





- TOOLS
- Related articles in NS
-
Reply to Commentary on “Classification(s) of Cervical Deformity”2023 March;20(1)
Commentary on “Classification(s) of Cervical Deformity”2023 March;20(1)
Circumferential Operations of the Cervical Spine2021 March;18(1)
Three-Column Osteotomy for the Treatment of Rigid Cervical Deformity2020 September;17(3)
Complex Revision Surgery for Cervical Deformity or Implant Failure2020 September;17(3)
-
Journal Impact Factor 3.2



























