Characteristics and Comparisons of Morphometric Measurements and Computed Tomography Hounsfield Unit Values of C2 Laminae for Translaminar Screw Placement Between Patients With and Without Basilar Invagination
Article information
Abstract
Objective
Patients with basilar invagination (BI) had high incidences of vertebral variations and high-riding vertebral artery (HRVA) that might restrict the use of pedicle or pars screw and increase the use of translaminar screw on axis. Here, we conducted a radiographic study to investigate the feasibility of translaminar screws and the bone quality of C2 laminae in patients with BI, which were compared with those without BI as control to provide guidelines for safe placement.
Methods
In this study, a total of 410 patients (205 consecutive patients with BI and 205 matched patients without BI) and 820 unilateral laminae of the axis were included at a 1:1 ratio. Comparisons with regard to insertion parameters (laminar length, thickness, angle, and height) for C2 translaminar screw placement and Hounsfield unit (HU) values for the assessment of the appropriate bone mineral density of C2 laminae between BI and control groups were performed. Besides, the subgroup analyses based on the Goel A and B classification of BI, HRVA, atlas occipitalization, and C2/3 assimilation were also carried out. Furthermore, the factors that might affect the insertion parameters and HU values were explored through multiple linear regression analyses.
Results
The BI group showed a significantly smaller laminar length, thickness, height, and HU value than the control group, whereas no significant difference was observed regarding the laminar angle. By contrast, the control group showed significantly higher rates of acceptability for unilateral and bilateral translaminar screw fixations than the BI group. Subgroup analyses showed that the classification of Goel A and B, HRVA, atlas occipitalization, and C2/3 assimilation affected the insertion parameters except the HU values. Multiple linear regression indicated that the laminar length was significantly associated with the male gender (B = 0.190, p < 0.001), diagnoses of HRVA (B = -0.109, p < 0.001), Goel A (B = -0.167, p < 0.001), and C2/3 assimilation (B = -0.079, p = 0.029); the laminar thickness was significantly associated with the male gender (B = 0.353, p < 0.001), diagnoses of HRVA (B = -0.430, p < 0.001), Goel B (B = -0.249, p = 0.026), and distance from the top of odontoid to the Chamberlain line (B = -0.025, p = 0.003); laminar HU values were significantly associated with age (B = -2.517, p < 0.001), Goel A (B = -44.205, p < 0.001), Goel B (B = -25.704, p = 0.014), and laminar thickness (B = -11.706, p = 0.001).
Conclusion
Patients with BI had narrower and smaller laminae with lower HU values and lower unilateral and bilateral acceptability for translaminar screws than patients without BI. Preoperative 3-dimensional computed tomography (CT) and CT angiography were needed for BI patients.
INTRODUCTION
Posterior screw placement for C2 vertebrae, including transarticular, pedicle, pars, and translaminar screw fixations, has been used for the treatment of cervical spine pathologies [1]. Among these methods, C2 pedicle and pars screw placements have been frequently applied with high safety of fixation and sufficient biomechanical stability [2-4]. However, the difficulty of accurate placement for C2 pedicle or pars increases in patients with pedicle anomalies and high-riding vertebral artery (HRVA), and the malposition might contribute to catastrophic outcomes, including injuries of the vertebral artery (VA) and spinal cord [5,6]. Translaminar screw placement (TSP), which was first introduced by Wright [7], has been regarded as an alternative strategy for C2 fixation because of its placement under direct visualization, elimination of the need for navigation or fluoroscopy, low risk of critical neurovascular injury, and comparable atlantoaxial stabilization [8-10].
For patients with basilar invagination (BI), narrow C2 pedicles and isthmuses of the pars are commonly observed, and the incidence of HRVA is remarkably increased, which reduces the safe zone for the trajectory of pedicle and pars screws [2,11,12]. Thus, the TSP is frequently utilized as a salvage method for C2 fixation in BI. Previous research primarily focuses on morphometric measurements, including laminar length, thickness, angle, and height, for translaminar screw insertion on the axis and subaxial cervical segments for people without congenital cervical vertebral anomalies, indicating that TSP can be a reliable and alternative method at these levels [8,13-17]. In addition, the acceptability of TSP is analyzed in some studies. Chan et al. [18] performed morphometric analysis of the C1 and C2 laminae and found that 65.5% of C1 and 80.3% of C2 laminae could accept 3.5 mm screws. Ma et al. [19] conducted a cadaveric specimen study to assess the applicability of C2 TSP in adult population and indicated that 5% and 9.2% specimens had a laminar thickness of ≤ 4.0 mm bilaterally and unilaterally. Nevertheless, to our knowledge, no study has been conducted to explore the characteristics of insertion parameters and feasibility of TSP on the C2 vertebrae in BI, and compared these parameters between patients with and without BI.
The Hounsfield unit (HU) obtained from computed tomography (CT) has been widely used for the calculation of bone mineral density (BMD) and the estimation of bone strength [20-22]. Moreover, HU measured at a region of interest (ROI) of the screw trajectory presents the approximate BMD and correlates strongly with insertion torque and implant stability in vitro and in vivo studies [23-26]. Furthermore, Han et al. [27] demonstrated that HU values on C2–3 segments indicate a more reliable BMD level than those on C4–7 segments, and HU values of cervical CT provided reliable information regardless of measured sections, age, sex, and degree of degeneration. Therefore, the BMD, insertion torque, and implant stability of translaminar screw can be approximately compared between patients with and without BI using the HU values measured on C2 laminae.
Thus, this study aimed to evaluate the anatomic acceptability and feasibility of TSP with regard to insertion parameters and assess the approximate BMD using HU values on C2 laminae in BI patients, and these parameters were compared with those in patients without BI to provide pertinent clinical data for translaminar screw insertion. Moreover, the factors that might affect the insertion parameters and HU values were explored through multiple linear regression.
MATERIALS AND METHODS
1. Patients and Study Design
Ethical approvals were provided by the ethics committees of the First Affiliated Hospital of Anhui Medical University Ethics Committee and the First Affiliated Hospital of the University of Science and Technology of China Ethics Committee (PJ2022-09-27; 2022-RE-091). Since this is a retrospective study, formal consent is not required. A total of 205 consecutive patients diagnosed with BI according to the Chamberlain line [28] between April 2017 and April 2022 were included. Meanwhile, 205 patients without BI were randomly selected on the basis of the medical records and matched as controls based on age and sex. The inclusion criteria were as follows: (1) ages between 18 and 75 years and (2) patients undergoing 3-dimensional (3D) CT examinations of the head and cervical spine. The exclusion criteria were as follows: (1) postoperative patients whose normal anatomical structures were destroyed, (2) patients with rheumatoid arthritis on many years of steroid treatment, (3) patients with BI secondary to Paget disease, (4) diagnoses of cervical tumor and infection on occipital and cervical regions and fractures violating the pedicles and laminae on the axis, (5) images with unsatisfactory quality or mental artifacts, and (6) incomplete data for review cases.
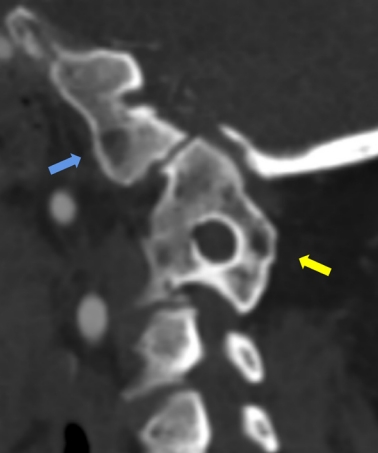
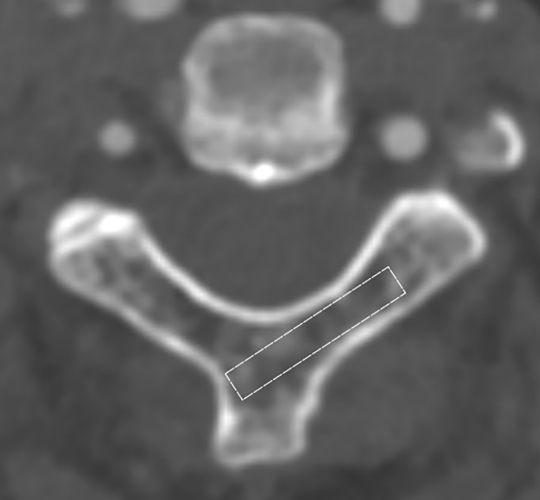
Various indications for TSP, such as criteria developed by Shin et al. [8], Alvin et al. [13], and Chan et al. [18], have been published for the safety and accuracy of fixation. In this study, the Chan criterion was used for the evaluation of the unilateral and bilateral acceptability of TSP. Subgroup analyses based on the classification of Goel type A and B subtypes in BI (Fig. 1) [29,30], HRVA (Fig. 2) [18,31], and the presences of atlas occipitalization and C2/3 assimilation (Fig. 3) were also performed to determine the characteristics of the laminar morphology and feasibility of TSP on the axis.

(A) The sagittal section of Goel A in basilar invagination. (B) The coronal section of Goel A in basilar invagination. (C) The sagittal section of Goel B in basilar invagination. (D) The coronal section of Goel B in basilar invagination.

(A) The sagittal section was identified with a line (a) transecting the midportion of the C1–2 facet joint on the coronal section. (B) The high-riding vertebral artery was defined on the sagittal section of the axis as an internal height (b) ≤ 2 mm, isthmus height (c) ≤ 5 mm, or both.
2. Radiological Measurements
A slice of CT images was 0.625 mm thick, and radiological measurements were performed along multiplanar planes, including axial, coronal, and sagittal sections, after CT reconstructions on the workstation (General Electric Medical Systems, Milwaukee, WI, USA). The measurements were independently and blindly conducted by 2 independent reviewers who were familiar with cervical anatomy. The average values of continuous variables measured by the 2 independent observers were utilized in this research. If divergence occurred during categorical grading, then a third senior independent observer will make the final decision.
3. Morphometric Measurements
The size and morphology of the laminae were measured to determine the feasibility of translaminar fixation on the axis. The following insertion parameters were evaluated on the same para-axial plane correlating with the thinnest part in the midportion of the lamina (Fig. 4A): (1) laminar length refers to the length from the contralateral junction of the lamina and spinous process to the lateral cortex of the lateral mass [32,33]; (2) laminar thickness is the shortest distance portion of the lamina [32]; (3) laminar angle is the angle from the axis of the lamina to a line passing through the spinous process and vertebral body, which represents the screw trajectory along the longitudinal axis of the lamina using the spinous process as an insertion landmark [32,33]. Moreover, laminar height refers to the length from the most rostral point and the most caudal portion of the lamina, which was assessed on the para-sagittal section (Fig. 4B) [16].
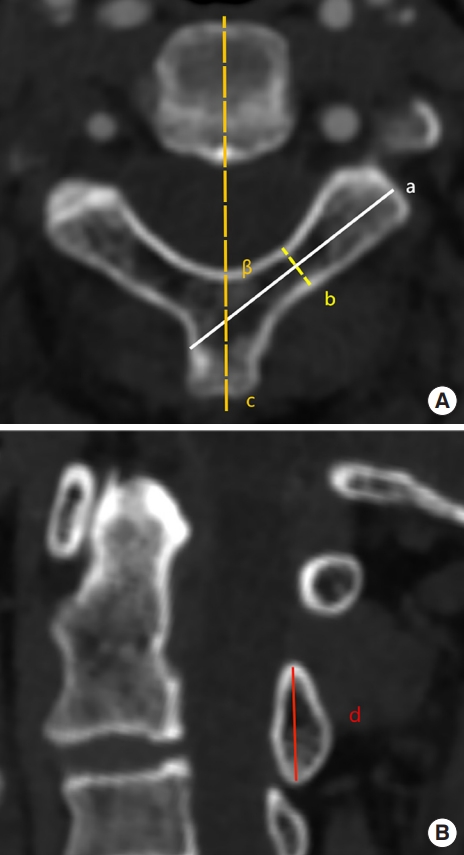
(A) Parameters measured in the para-axial section correlating with the thinnest part in the midportion of lamina. Laminar length (a), the length from the contralateral junction of lamina and spinous process to the lateral cortex of the lateral mass; laminar thickness (b), the shortest distance portion of the lamina; laminar angle (β), the angle from the axis of lamina (a) to a line (c) passing through the spinous process and vertebra body. (B) Parameters measured in the para-sagittal section of C2 lamina. Laminar height (d), the length from the most rostral point and the most caudal portion of lamina.
Based on the Chan criterion [18], for laminae undergoing unilateral placement, the minimum laminar thickness and height should not be less than 4.5 mm if a 3.5-mm screw was inserted with a margin of error of 0.5 mm on each side, and the minimum laminar length must be 20 mm; for patients receiving bilateral placement, the bilateral laminar thickness, bilateral length, and bilateral height should be ≥ 4.5, ≥ 20, and ≥ 9 mm, respectively. In addition, for patients with laminar assimilation of C2/3, the measurement of laminar height was abandoned, and it was assumed that the height of the lamina was large enough to accommodate the safe unilateral placement of the screw. On the contrary, patients with C2/3 assimilation were excluded from the assessment of bilateral placement because of limited data of laminar height.
We reported 2 sets of quantitative data of C2 laminae, namely, measured values for unilateral laminae suitable for screw placement and values for all included unilateral laminae. The former indicated the values of laminae that met the Chan criterion for TSP to provide useful guidelines for their safe placement, whereas the latter showed the demographic characteristics of unilateral laminae between patients with and without BI.
4. CT Hounsfield Unit Values
A ROI was selected using para-axial slices of C2 laminae on the GE workstation for the calculation of an average HU value. The ROI was fixed at 20 mm× 4.5 mm, which represented the Chan criterion [18] for TSP, and all cortical regions (inner and outer walls of the laminae) were avoided during HU attenuation measurement (Fig. 5). In addition, for patients with laminar thickness or length less than the abovementioned ROI (20 mm× 4.5 mm), the ROI was adjusted by reducing the length or width for the accommodation in the laminae and avoidance of overlapping with cortical bone that would falsely elevated HU values.
5. Statistical Analyses
Statistical analyses were completed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). Independent t-test and analysis of variance test were performed to compare 2 sets and multiple sets of quantitative data based on normal distribution. Otherwise, the Wilcoxon test and Kruskal-Wallis test were used for 2 and multiple sets of continuous variables. The nominal p-value was adjusted as 0.05 for multiple comparisons. The categorical variables were compared using the chi-square test. In addition, multiple imputation was performed to obtain missing data. Furthermore, factors that affect the insertion parameters, including sex, age, classification of Goel A and B subtypes, distance from the top of odontoid to the Chamberlain line, diagnosis of HRVA, atlas occipitalization, and C2/3 assimilation, were analyzed using multiple linear regression. By contrast, factors that affect the CT HU values, including the abovementioned possible risk factors, laminar length, laminar thickness, and laminar angle, were explored using multiple linear regression. A p-value of < 0.05 was considered statistically significant.
RESULTS
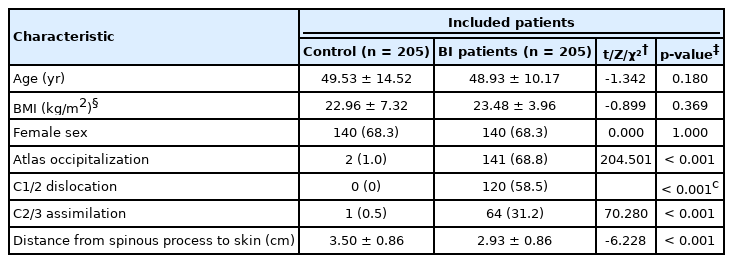
1. Patient Demographic Data
In this comparative study, a total of 410 patients with and without BI were included at a 1:1 ratio. In the BI group, 59.02% of patients (121 of 205) were diagnosed with Goel A type, and the remaining 40.98% of patients (84 of 205) were diagnosed with Goel B type. No significant differences in mean demographic profiles, including age, body mass index (BMI), and gender, were observed between BI and control groups (p > 0.05) (Table 1) and between Goel A and B groups (p > 0.05) (Supplementary Table 1). A total of 31 (15.1%) and 24 patients (11.7%) in the BI and control group, respectively, lacked the BMI information of medical records and missing data were addressed by using a multiple imputation model. Furthermore, the BI group and Goel A group showed significantly higher rates of atlas occipitalization, C1/2 dislocation, and C2/3 assimilation, and significantly shorter distance from the spinous process to the skin than the control group and Goel B group (p < 0.001) (Table 1, Supplementary Table 1).
2. Acceptability of Unilateral and Bilateral TSPs
The acceptable rates of unilateral and bilateral translaminar fixations using the criteria of Shin, Alvin, and Chan are shown in Supplementary Tables 2 and 3.
The results showed that based on the Shin criterion, the control group was associated with a significantly higher rate of acceptability for unilateral translaminar fixation than the BI group (p < 0.001); meanwhile, the Goel A group showed a significantly lower rate of acceptability for unilateral translaminar fixation than the Goel B group (p = 0.010). Based on the Alvin criterion, the control group indicated a significantly higher rate of acceptability for unilateral translaminar fixation than the BI group (p < 0.001), but no significant difference was observed between Goel A and B groups (p = 0.897).
Based on the Chan criterion, the control group showed significantly higher rates of acceptability for unilateral and bilateral translaminar fixations than the BI group (p < 0.001), but such differences were not significant between Goel A and B groups (p > 0.05).
3. Comparative Outcomes Between the Control and BI Groups
For the unilateral C2 laminae suitable for screw placement (Table 2) and the overall unilateral C2 laminae (Supplementary Table 4), the BI group showed significantly smaller laminar length, thickness, height, and HU values than the control group (p < 0.05), whereas no significant difference in laminar angle was observed between the 2 groups.
4. Subgroup Comparisons Based on Goel Classification
For the unilateral C2 laminae suitable for screw placement (Table 3) and the overall unilateral C2 laminae (Supplementary Table 5), the Goel A group showed significantly smaller laminar length, larger laminar angle, and larger laminar height than the Goel B group (p < 0.05), but no significant difference in laminar thickness and HU values was observed between the 2 groups.
5. Subgroup Comparisons Based on the Diagnosis of HRVA
For the unilateral C2 laminae suitable for screw placement (Table 4) and the overall unilateral C2 laminae (Supplementary Table 6), the HRVA group had a significantly smaller laminar height than the non-HRVA group in the control cohort (p = 0.028) and a significantly shorter laminar length and thickness in the BI cohort (p < 0.001).

Subgroup comparisons of morphometric measurements and computed tomography HU values for unilateral C2 laminae suitable for screw placement between the control and BI groups based on the diagnosis of HRVA
Moreover, we found that for unilateral laminae with HRVA, the BI group had significantly smaller laminar length, height, and HU values than the control group; for unilateral laminae without HRVA, the BI group had significantly smaller laminar height and HU values than the control group (p < 0.05).
6. Subgroup Comparisons Based on Goel Classification and the Diagnosis of HRVA
For the unilateral C2 laminae suitable for screw placement (Table 5) and the overall unilateral C2 laminae (Supplementary Table 7), the HRVA group was significantly associated with shorter laminar length and height compared with the non-HRVA group in Goel A cohorts (p < 0.001). In the Goel B cohort, no significant differences in morphometric measurements and HU values were observed between HRVA and non-HRVA groups (p > 0.05).
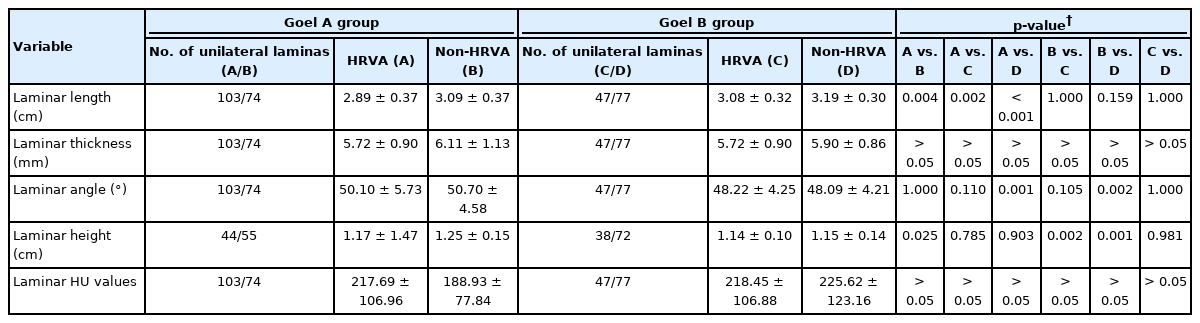
Subgroup comparisons of morphometric measurements and computed tomography HU values for unilateral C2 laminae suitable for screw placement between Goel A and B groups based on the diagnosis of HRVA
However, for the overall unilateral C2 laminae (Supplementary Table 7), the HRVA group was significantly associated with shorter laminar thickness compared with the non-HRVA group in Goel A cohorts (p < 0.001).
7. Subgroup Comparisons Based on the Presence of Atlas Occipitalization
For the unilateral C2 laminae suitable for screw placement (Supplementary Table 8) and the overall unilateral C2 laminae (Supplementary Table 9), the control group without atlas occipitalization had significantly smaller laminar height and HU values than BI groups with and without atlas occipitalization (p < 0.01). In the BI cohort, the atlas occipitalization group was associated with significantly smaller laminar length and angle than the non-atlas occipitalization group (p < 0.001).
8. Subgroup Comparisons Based on the Presence of C2/3 Assimilation
For the unilateral C2 laminae suitable for screw placement (Supplementary Table 10) and the overall unilateral C2 laminae (Supplementary Table 11), the control group without C2/3 assimilation had significantly smaller laminar length and HU values than BI groups with and without C2/3 assimilation (p < 0.05). In the BI cohort, the C2/3 assimilation group was associated with significantly smaller laminar length and angle than the non-C2/3 assimilation group (p < 0.001).
9. Multiple Linear Regressions
Multiple linear regressions were performed on the basis of the overall 820 unilateral C2 laminae, whereas factors affecting laminar height were explored on the basis of the 690 unilateral laminae. The results showed that the laminar length was significantly associated with the male gender (B = 0.190, p < 0.001), diagnoses of HRVA (B = -0.109, p < 0.001), Goel A (B = -0.167, p < 0.001), and C2/3 assimilation (B = -0.079, p = 0.029); the laminar thickness was significantly associated with the male gender (B = 0.353, p < 0.001), diagnoses of HRVA (B = -0.430, p < 0.001), Goel B (B = -0.249, p = 0.026), and distance from the top of odontoid to the Chamberlain line (B = -0.025, p = 0.003); the laminar angle was significantly associated with Goel A (B = 1.841, p < 0.001), C2–3 assimilation (B = 1.461, p = 0.001), and distance from the top of odontoid to the Chamberlain line (B = -0.195, p < 0.001); the laminar height was significantly associated with the male gender (B = 0.068, p < 0.001), diagnoses of HRVA (B = -0.041, p < 0.001), Goel B (B = -0.052, p < 0.001), and distance from the top of odontoid to the Chamberlain line (B = -0.007, p < 0.001); laminar HU values were significantly associated with age (B = -2.517, p < 0.001), Goel A (B = -44.205, p < 0.001), Goel B (B = -25.704, p= 0.014), and laminar thickness (B = -11.706, p = 0.001) (Supplementary Tables 12–16).
DISCUSSION
As an effective salvage method for axis fixation, translaminar screw might be frequently applied in patients with BI, for whom a high rate of contraindications for C2 pedicle or pars screw placement existed because of morphologic anomalies and the presence of HRVA [11,12,33,34]. However, the malposition of laminar screw can breach the inner cortex of laminae and damage the dura mater and spinal cord [19]. In addition, the morphologic variation of C2 laminae in BI and the effect of their morphologic characteristics and bone quality on safe placement and fixation stability of translaminar screw remain unclear.
Our study showed a screw acceptability rate in the control group similar to that of Chan et al. [18], who performed a CT image measurement in an Asian population and reported unilateral screw acceptability of 85.8% and 88.8% in the right and left laminae, respectively, and bilateral screw acceptability of 80.3% for C2. We also revealed that the BI group had subsequently lower rates of unilateral and bilateral screw acceptability than the control cohort. By contrast, no remarkable differences were observed between Goel A and B types in BI. In addition, majority of studies reported the insertion parameters of C2 translaminar screw in patients without congenital cervical vertebral anomalies [14,18,19,32,35-38]. The mean laminar length of 3.16±0.27 cm in the control group of our study was similar to that of studies conducted by Wang et al. [14], Kim et al. [35], and Xin-yu et al. [37] Meanwhile, the mean laminar thickness of 5.81±1.18 mm, mean laminar angle of 49.51°±3.03°, and mean laminar height of 1.24±0.13 cm in the control group were consistent with reports by Dean et al. [32], Ma et al. [19], and Chan et al. [18] in adult population. Compared with the control group, we found that the laminar length, thickness, and height in the BI cohort were remarkably smaller. These results might be attributed to craniovertebral anomalies in BI patients who had high incidence of morphological variations, atlas occipitalization, C2/3 assimilation, and pathogenesis of posterior axial elements, including the absence and incompleteness of the isthmus and spinous process, thereby increasing the risk of malposition of translaminar screws [34,39,40]. Moreover, except for congenital morphological anomalies, patients with BI likely suffered from developmental central or axial atlantoaxial instability, which further increased the difficulty of accurate screw placement [39,41].
The classification of Goel A and B types in BI was based on the abnormal increase in atlantodental or clivodental interval, which represented atlantoaxial instability [42]. The atlantoaxial instability was considered abnormally and excessively mobile in Goel A but stable and subtle in Goel B [41]. In subgroup analyses of Goel A and B types, the laminar length, angle, and height in the Goel A group were substantially smaller than those in the Goel B group. Thus, the morphological anomaly of Goel B type was found to be more stable than that of Goel A type. Nevertheless, multiple linear regression revealed that the Goel B type independently contributed to smaller laminar thickness and height, whereas the Goel A type was independently associated with a smaller laminar length and larger laminar angle. Therefore, the classification of Goel A and B types was required preoperatively through 3D CT for the clarification of morphological deformity and personalized treatment to reduce the risk of malposition.
We also investigated the effects of HRVA on the insertion parameters of TSP in control and BI cohorts. In previous studies, the diagnosis of HRVA was remarkably associated with a narrow pedicle and a thin isthmus on the C2 vertebra [5,43]. However, whether a narrow and short lamina existed in the presence of HRVA remained unclear. In the current study, we found that the insertion parameters had no substantial differences between unilateral laminae with and without HRVA in the control group. By contrast, for patients with BI, unilateral laminar length and thickness, the critical parameters for TSP, were remarkably smaller in the HRVA group than those in the nonHRVA group. In further subgroup analyses of Goel A and B types, no substantial differences in insertion parameters were found between laminae with and without HRVA in the Goel B group, but the HRVA cohort had remarkably smaller laminar length, thickness, and height than the non-HRVA group for all included laminae in the Goel A group. In addition, multiple linear regression analyses indicated that the presence of HRVA was an independent factor for the smaller laminar length, thickness, and height on the C2 lamina. Thus, the diagnoses of HRVA and Goel A in BI contributed to a narrow lamina, which might increase the risk of malposition, and the preoperative evaluation of VA should be performed to avoid potential neurovascular injuries.
The insertional torque of a screw and the ultimate fixation strength of a device had positive correlations with BMD, which can be approximately assessed on the basis of HU values obtained from CT [44,45]. We found that a reduced bone quality evaluated by HU values was present in the trajectory of the laminar screw for the BI group compared with that for the control cohort, and no remarkable differences in HU values were found between Goel A and B groups. Meanwhile, subgroup analyses demonstrated that the BMD was not affected by the presences of HRVA, atlas occipitalization, and C2/3 assimilation except for the diagnosis of BI. Moreover, the multiple linear regression revealed that older age, smaller laminar thickness, and diagnosis of Goel A or B type independently contributed to low HU values. Elderly patients had a high risk of osteoporosis, an age-related disease, thereby resulting in low bone quality. Besides, Goel A and B types, which were the diagnosis of BI, might be associated with lower BMD. The mean HU value in the BI cohort was 226.21±121.78, which was higher than the determination for osteoporosis, with a HU interval value of 90.9 to 138.7.45 The low BMD and bone quality in BI might result from the complication of osteogenesis imperfecta and related osteochondrodysplasias, and these so-called “bone softening” disorders further contributed to progressive deformity and neurological dysfunction [46,47].
It should be noted that the gold standard for the assessment of BMD is the dual-energy x-ray absorptiometry (DXA). Studies have found a correlation between HU values and BMD based on DXA [21,48-50]. Pinto et al. [45] performed a meta-analysis based on 18 studies comparing HU values from spine CT scans to the T scores of gold-standard DXA for the prediction of regional BMD, concluding that the bone quality can be assessed according to HU values obtained from CT. Thus, the HU values in the BI and control groups can approximately show the differences of BMD and bone quality between the 2 groups. Although the HU values have not been widely used for the assessment of BMD in the clinical practice, using HUs values to infer bone quality has a thorough clinical relevance as it could be used for the classification of patients at at risk for osteoporotic and fragility fractures [45].
Inconsistencies in insertion parameters were found in the results of some studies [15,36,38], which might be attributed to the following reasons. First, different methods of measurement were used. For example, a different measurement method for laminar length performed by Cassinelli et al. [15] was performed from the contralateral spinolaminar junction to the lamina/lateral mass junction, which resulted in smaller outcomes compared with the current study. Second, patients with different ethnicities were included. The studies from Korean, Malay, Indian, and American populations conducted by Kim et al. [35], Chan et al. [18], Srivastava et al. [16], and Cassinelli et al. [15], respectively, showed the discrepancies of the same insertion parameters among different ethnicities. Third, different planes were selected for measurement. Ma et al. [19] found a high variability of thickness for the C2 lamina: the thinnest cranial portion, averaging 2.71 mm; the thickness of the caudal edge, averaging 4.46 mm; the thickest portion at the midportion of the lamina, averaging 5.87 mm. Fourth, the included population had different ratios of gender. Cassinelli et al. [15] reported that males had a greater C2 laminar thickness than females. Our study also found that the male gender was independently associated with larger laminar length, thickness, and height. Therefore, the conditions where the parameters were measured should be clarified before utilization in clinical practice.
This study had some limitations. First, given the lack of BMI in medical records for some patients, missing data were obtained by multiple imputation. Thus, the outcomes regarding BMI should be interpreted cautiously. Second, this study was limited to the Eastern Asian population, which has limited generalizability of measured outcomes. Therefore, the morphometric measurements and HU values among different ethnicities must be further investigated. Third, subgroup comparison based on gender, left or right side, were not performed, and biases resulting from 2 factors were reduced by matching gender and the number of included patients between BI and control groups in this study. Fourth, the measurements were performed using 3D CT images without actual clinical application, and the confirmative study concerning the insertion parameters on cadaveric specimens should be carried out.
CONCLUSION
Patients with BI had narrower and smaller laminae with lower HU values and lower unilateral and bilateral acceptability for translaminar screws than patients without BI. The morphometric measurements were affected by gender, classification of Goel A and B types, and the presence of HRVA and C2/3 assimilation, and HU values were affected by age, classification of Goel A and B types, and laminar thickness for C2 laminae.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1-16 can be found via https://doi.org/10.14245/ns.2244730.365.
Descriptive statistics of the patients in Goel A and B groups
Feasibility and acceptability of laminar screw on unilateral C2 laminae with published criteria
Feasibility and acceptability of laminar screw on bilateral C2 laminae with published criteria
Comparisons of morphometric measurements and computed tomography HU values for overall unilateral C2 laminae between the control and BI groups
Comparisons of morphometric measurements and computed tomography HU values for overall unilateral C2 laminae between the Goel A and B groups
Subgroup comparisons of morphometric measurements and computed tomography HU values for overall unilateral C2 laminae between the control and BI groups based on the diagnosis of HRVA
Subgroup comparisons of morphometric measurements and computed tomography HU values for overall unilateral C2 laminae between Goel A and B groups based on the diagnosis of HRVA
Subgroup comparisons of morphometric measurements and computed tomography HU values for unilateral C2 laminae suitable for screw placement between the control and BI groups based on the diagnosis of atlas occipitalization
Subgroup comparisons of morphometric measurements and computed tomography HU values for overall unilateral C2 laminae between the control and BI groups based on the diagnosis of atlas occipitalization
Subgroup comparisons of morphometric measurements and computed tomography HU values for unilateral C2 laminae suitable for screw placement between the control and BI groups based on the diagnosis of C2-3 assimilation
Subgroup comparisons of morphometric measurements and computed tomography HU values for overall unilateral C2 laminae between the control and BI groups based on the diagnosis of C2–3 assimilation
Multiple linear regression on laminar length
Multiple linear regression on laminar thickness
Multiple linear regression on laminar angle
Multiple linear regression on laminar height
Multiple linear regression on laminar HU values
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: LPZ, JS, RJZ, CLS; Data curation: LPZ, ZGZ, ZFJ, HQZ, CYJ, RJZ; Formal analysis: LPZ, JS, ZGZ, ZFJ, HQZ, CYJ, RJZ; Methodology: LPZ, JS, ZGZ, CYJ, RJZ, CLS; Project administration: CLS; Visualization: CLS; Writing - original draft: LPZ; Writing - review & editing: LPZ, JS, ZGZ, ZFJ, HQZ, CYJ, RJZ, CLS.