|
 |
- Search
|
|
||
See commentary "Commentary on ŌĆ£Cervical Inclination Angle: Normative Values in an Adult Multiethnic Asymptomatic PopulationŌĆØ" in Volume 20 on page 410.
Abstract
Objective
The role of the craniocervical complex in spinal sagittal alignment has rarely been analyzed but it may play a fundamental role in postoperative mechanical complications. The aim of the study is to analyze the normative value of the cervical inclination angle (CIA) in an adult asymptomatic multiethnic population.
Methods
Standing full-spine EOS of adult asymptomatic volunteers from 5 different countries were analyzed. The CIA was analyzed globally and then in each decade of life. Different ethnicities were compared. Comparisons between different groups was performed using a t-test and statistical significance was considered with a p-value < 0.05.
Results
EOS of 468 volunteers were analyzed. The global mean CIA was 80.2┬░ with a maximum difference of 9┬░ between T1 and T12 (p < 0.001). The CIA remains constant until 60 years old then decreases significantly passing from a mean value before 20 years old of 82.25┬░ to 73.65┬░ after 70 years old. A statistically significant difference was found between the Arabics and other ethnicities with the formers having an inferior CIA: this was related to a mean older age (p < 0.05) and higher body mass index (p < 0.05) in the Arabics.
Conclusion
The CIA remains constant until 60 years old and then reduces slightly but never under 70┬░. This angle is helpful to evaluate the lever arm at the upper instrumented vertebra after an adult spinal deformity surgery and could predict the occurrence of a proximal junctional kyphosis when its value is lower than normal. Further clinical studies must confirm this theory.
With the improvements in health care and life expectancy we witness a raise in adult spinal deformity (ASD) incidence with a reported prevalence up to 68% in patients over 60 years [1-4].
When treating ASD, it is mandatory to respect the appropriate sagittal and coronal alignments to have good clinical outcomes and prevent mechanical complications [5-8]. The necessity to keep the head over the pelvis is a fundamental rule firstly supported by Dubousset [5,9]: this means that the cervical spine and the head must be included in the balance analysis.
The principal reported mechanical complication in ASD surgery is proximal junctional kyphosis (PJK) that can affect up to 60% of patients undergoing ASD correction with long or short instrumentations with a consequent high rate of reinterventions [4,10-12]. This complication was first defined by Glattes et al. [13] as a kyphotic angle greater than 10┬░ between the upper instrumented vertebra (UIV) and 2 vertebrae above. Several risk factors have been advocated as responsible for the development of PJK and different attempts have been made to classify this complication to reduce its occurrence [4,10,11,14,15].
The role of the craniocervical complex (CCC) and the upper thoracic spine has rarely been analyzed and only recently Cerpa et al. [16] have proposed that the posterior skull plumbline anterior to the UIV on postoperative standing x-rays may be a risk factor for PJK. To analyze the role of the CCC on the global spinal alignment and on the risk of PJK, a new angle was proposed: the cervical inclination angle (CIA), defined as an angle between the center of the odontoid, the midpoint of each thoracic vertebra superior endplate and a horizontal line starting from the center of each thoracic vertebra endplate [17,18]. This angle was described to avoid the drawbacks of the C7 sagittal vertical axis which is measured in millimetres and has the inconvenient to be dependant of the length of the spine and the magnification calculation. With the CIA those 2 inconvenient are avoided.
It is known that to maintain an ergonomic sagittal alignment, with less paravertebral muscular effort, the thoracic and cervical spine should be aligned and have small anterior lever arms: each centimetre of anterior displacement of the gravity line results in +3.5 Nm bending moment that raises the risk of vertebral fracture and discal damage [17,18].
The aim of this paper is to confirm the reproducibility of the CIA in an adult asymptomatic population and then to analyze its correlation with the other main sagittal parameters.
Asymptomatic adult volunteers between the ages of 18ŌĆō80 years were enrolled prospectively across 5 different countries/centers (France, Japan, Singapore, Tunisia, and United States) forming the MEANS cohort. The study was approved by all local Institutional Ethics Review Boards for each respective center. Volunteers included in the study reported no significant neck or back pain (visual analogue scale Ōēż 2), nor any known spinal disorder(s), and had no history of prior surgical or nonsurgical treatment for a spine related disorder. All volunteers underwent a standing full body or full-spine low-dose stereoradiograph (EOS Imaging, part of ATEC Spine, Inc, Carlsbad, CA, USA) for enrolment in the study. Those with an abnormal vertebral count or transitional anatomy were excluded from the analysis. Following exclusion, a total of 468 patients were included in MEANS. Basic demographic data included age, sex, body mass index (BMI), and ethnicity. Oswestry Disability Index (ODI) scores were also obtained.
All radiographic measurements were performed using a 2D/3D sterEOS modelling software (EOS Imaging). The following sagittal parameters were analyzed for the study: pelvic incidence (PI), pelvic tilt (PT), L1S1 lumbar lordosis (LL), thoracic kyphosis (TK), C7 slope, odontoid-hip axis angle (OD-HA), CIA, and odontoid-thoracic distance (Th-OD) (defined as the distance from the odontoid plumbline and the center of each thoracic vertebra superior endplate). This distance represents the lever arm applied on each vertebral plateau (Fig. 1).
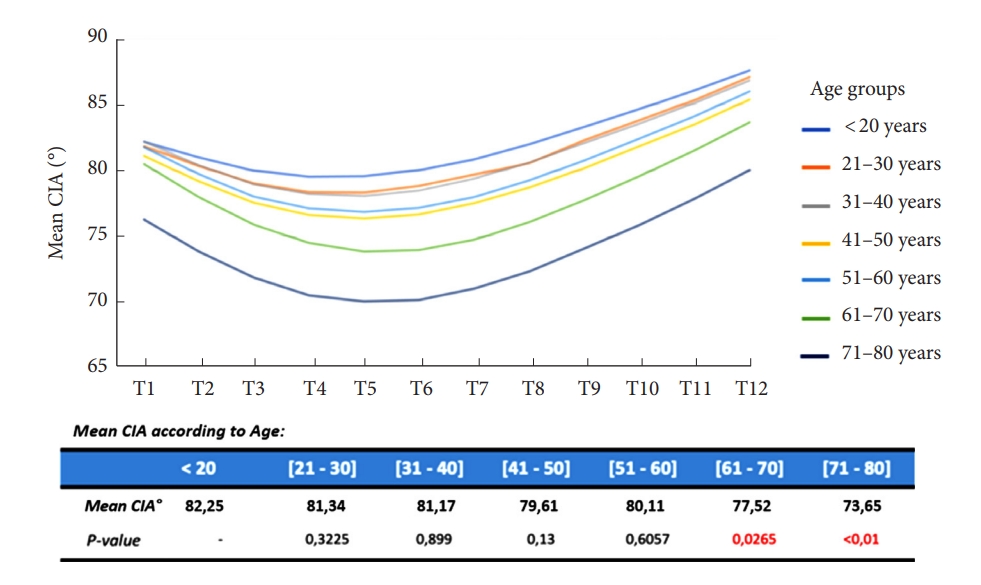
The CIA was first analyzed globally and then in each decade of life (< 20 years [n=12], 21ŌĆō30 years [n=143], 31ŌĆō40 years [n=108], 41ŌĆō50 years [n=94], 51ŌĆō60 years [n=58], 61ŌĆō70 years [n=40], 71ŌĆō80 years [n=19]).
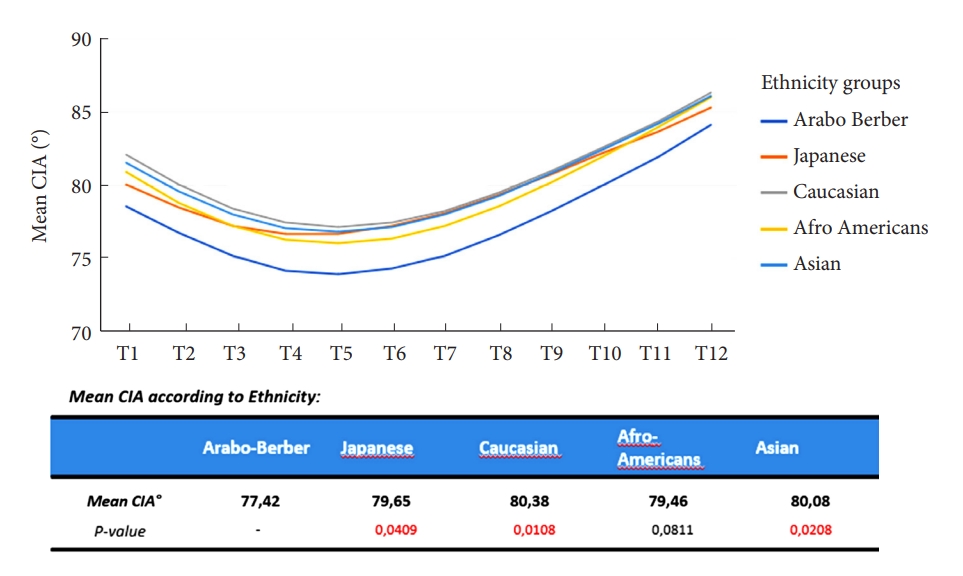
The global population was then divided into 5 different major ethnicities (Caucasian, Japanese, Afro-Americans, Arab-Berber, Asians) and an analysis was performed to identify if the CIA remained constant and reproducible.
The CIA was then analyzed in relation to the BMI and, finally, based on volunteers Roussouly type dividing the population in 3 groups according to the PI value (PI< 45┬░=Roussouly 1 and 2; PI 45┬░ŌĆō60┬░=Roussouly 3; PI> 60┬░=Roussouly 4) [19].
Statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Categorical variables were expressed as number of cases and percentage. Continuous variables were reported as mean┬▒standard deviation; means were compared with the Student t-test. Two-sided p-values and/or 95% confidence interval (CI) were reported, and significance was accepted at p < 0.05.
Comparisons between different age groups and ethnicities was performed using a t-test and statistical significance was considered with a p < 0.05. Correlations between CIA and BMI, and between CIA and Roussouly type, were performed with a Mann-Whitney test and significance was assessed for a p < 0.05.
Finally, correlations between the CIA and the other major sagittal parameters were assessed with a Pearson correlation coefficient (R: -1 to +1; where -1 identifies a negative correlation while +1 a positive correlation) and significance was assessed for p < 0.05.
Four hundred sixty-eighty adult asymptomatic volunteers were included in the analysis (176 Caucasians, 119 Japanese, 12 Afro-Americans, 80 Arab-Berber, 81 Asians). The mean age was 40,4┬▒14,8 years (95% CI, 39.1ŌĆō41.7) and the mean BMI was 24.5┬▒5.3 kg/m┬▓ (95% CI, 24.0ŌĆō25.1). The male to female ratio was 184:284. The mean visual analogue score was 0.3┬▒0.5 (95% CI, 0.2ŌĆō0.3) and the ODI score was 2.2%┬▒4.1% (95% CI, 1.9ŌĆō2.6).
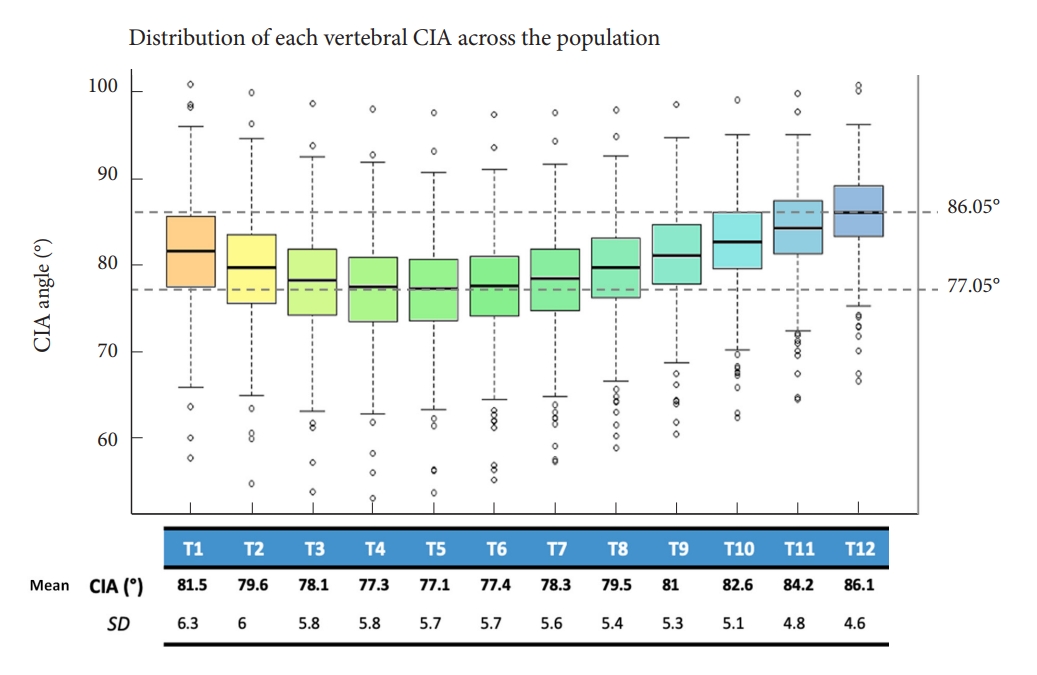
The global CIA mean value was 80.12┬░┬▒2.8┬░ (95% CI, 78.28ŌĆō81.96) with a maximal difference of 9┬░ between all thoracic vertebrae (min T5= 77.05┬░ to max T12= 86.05┬░, p < 0.001) (Fig. 2).
Of the included volunteers 12 had Ōēż 20 years, 142 had 21 to Ōēż 30 years, 107 had 31 to Ōēż 40 years, 93 had 41 to Ōēż 50 years, 57 had 51 to Ōēż 60 years, 39 had 61 to Ōēż 70 years, and 18 were older than 70 years old. When analyzing the CIA by different decades of life, we observed a significant decrease of the angle after 60 years old: the CIA remains constant until 60 years old (p > 0.05) and then decreases at all thoracic levels passing from 82.25┬░ to 73.65┬░ of mean value (p < 0.05) (Fig. 3).
Considering the ethnicities, a difference was observed between the Arab-Berbers and the other populations. The Arab-Berber had a statistically lower CIA mean value at each thoracic level (p < 0.05) (Fig. 4). It should be highlighted that the Arab-Berber population had an older age (45.48┬▒14.77 years vs. 39.35┬▒14.58 years, p < 0.05) and a higher BMI (27.13┬▒5.23 kg/m┬▓ vs. 23.86┬▒5.15 kg/m┬▓, p < 0.001) compared to the other populations.
When analyzing CIA in relation to BMI, no statistically significant correlation was observed between these 2 parameters (p = 0.100). Furthermore, Roussouly type (group 1 = PI < 45┬░, Roussouly 1 and 2; group 2 = PI 45┬░ŌĆō60┬░, Roussouly 3; group 3= PI> 60┬░, Roussouly 4) did not have an influence on CIA values (group 1 vs. group 2, p = 0.748; group 1 vs. group 3, p = 0.446; group 2 vs. group 3, p = 0.578).
The CIA demonstrated good negative correlations with the Th-OD distance (p < 0.001), the OD-HA angle (p < 0.001), the C7 slope (p < 0.001), the TK (p < 0.001) whereas no or little correlations were observed with the LL, lower LL (L4S1), and the PT (p > 0.05) (Table 1).
The goal of an ASD corrective surgery should be a satisfying global sagittal balance so that the patient may have a horizontal gaze and an upright position with the head over the hips [5].
Despite all the efforts made to avoid postoperative mechanical complications, the rate of PJKŌĆÖs is still very high [4]. Several factors have been advocated as responsible for this event but rarely the effect of an excessive lever arm on the UIV has been discussed [10,11,14]. To analyze this lever arm, the CIA has been proposed with a mean reported value of 77,7┬░ [17].
Here we confirm the reproducibility of this angle with a reported mean value of 80.12┬░┬▒2.8┬░ and we were able to confirm that the CIA remains constant through different ages, despite BMI and Roussouly type, until 60 years old. When planning an ASD correction, the surgeon should keep this angle in mind and try to restore the sagittal alignment avoiding an excessive lever force on the UIV (CIAŌēł80┬░).
The value of the CIA is confirmed by its correlation to other important sagittal parameters. Here we have observed a strong negative correlation with the C7 slope, TK, OD-HA, and ThOD: this means that the increasing value of these parameters correspond to a reduction in the CIA. It is well known that with aging the TK raises due to disc degeneration, vertebral body wedging and reduce paravertebral muscle strength [17]. The increase in TK corresponds to a major C7 slope and to a forward displacement of the trunk with a consequent higher OD-HA angle and higher Th-OD distance [20]. The anterior shift of the trunk raises the bending moment and consequently the risk of a vertebral fracture or PJK [17]. In this scenario an excessive reduction of the CIA at the UIV corresponds to an increased risk of mechanical complications.
We have observed a lower normative value of this angle in the Arabo-Berber population, but as reported previously, this might be influenced by the mean older age in this population. The role of the aging process on the CIA has been demonstrated in this study. Concerning the BMI, it is uncertain if this could directly influence the value of the CIA, especially because we did not find significant correlations between higher body weight and CIA, but high BMI has already been reported as a minor risk factor for PJK [4,21,22].
We are aware that this study has some limitations as it is a descriptive analysis of an adult asymptomatic population and the role of the CIA in prevention of PJK should be confirmed with further clinical investigations. Nevertheless, we have demonstrated the reproducibility of this angle despite age, ethnicities or Roussouly type and its implications in the analysis of the global sagittal balance when planning an ASD correction surgery.
The CIA remains constant through ages until 60 years old and then reduces slightly but never under 70┬░. This angle might be a helpful tool to evaluate the lever arm at UIV on the thoracic spine after an ASD surgery and could predict the occurrence of a PJK when its value is lower than normal. Our experience support this feeling but further clinical studies must confirm this theory.
NOTES
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JCLH; Data curation: ZMS, EQ, MC, MPK, HWDH, HKW, HR, LGL, SB; Formal analysis: ZMS, EQ, MC, MPK, SB; Methodology: SB; Project administration: JCLH, ZMS, MPK, KH, HWDH, HKW, HR, LGL, SB; Visualization: JCLH, KH, LGL, SB; Writing - original draft: EQ; Writing - review & editing: JCLH.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Beatrice Dozin for her assistance in data analysis.
Fig.┬Ā2.
Graphic of the cervical inclination angle (CIA) value according to the thoracic vertebra. SD, standard deviation.
Table┬Ā1.
CIA correlations with OD-HA, C7 slope, TK, and Th-OD distance
REFERENCES
1. Youssef JA, Orndorff DO, Patty CA, et al. Current status of adult spinal deformity. Global Spine J 2013;3:51-62.




2. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082-5.


3. Ames CP, Scheer JK, Lafage V, et al. Adult spinal deformity: epidemiology, health impact, evaluation, and management. Spine Deform 2016;4:310-22.


4. Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 2014;39:2093-102.

5. Le Huec JC, Thompson W, Mohsinaly Y, et al. Sagittal balance of the spine. Eur Spine J 2019;28:1889-905.



6. Yilgor C, Sogunmez N, Boissiere L, et al. Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 2017;99:1661-72.


7. Obeid I, Berjano P, Lamartina C, et al. Classification of coronal imbalance in adult scoliosis and spine deformity: a treatment-oriented guideline. Eur Spine J 2019;28:94-113.



8. Le Huec JC, Faundez A, Dominguez D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal disease: a literature review. Int Orthop 2015;39:87-95.

9. Dubousset J. Three-dimensional analysis of the scoliotic deformity. In: Weinstein Set al., editors. The pediatric spine: principles and practice. New York: Raven Press; 1994. p. 479-96.
10. Lafage R, Beyer G, Schwab F, et al. Risk factor analysis for proximal junctional kyphosis after adult spinal deformity surgery: a new simple scoring system to identify high-risk patients. Global Spine J 2020;10:863-70.




11. Sakuma T, Kotani T, Akazawa T, et al. Incidence, risk factors, and prevention strategy for proximal junctional kyphosis in adult spinal deformity surgery. Spine Surg Relat Res 2020;5:75-80.



12. Hyun SJ, Kim YJ, Rhim SC. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J 2016;16:1095-101.


13. Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643-9.

14. Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 2012;37:1479-89.

15. Kim YJ, Bridwell KH, Lenke LG, et al. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine (Phila Pa 1976) 2007;32:2653-61.

16. Cerpa M, Sardar Z, Lenke L. Revision surgery in proximal junctional kyphosis. Eur Spine J 2020;29(Suppl 1):78-85.



17. Le Huec JC, Richards J, Tsoupras A, et al. The mechanism in junctional failure of thoraco-lumbar fusions. Part I: Biomechanical analysis of mechanism responsible of vertebral overstress and description of cervical inclination angle (CIA). Eur Spine J 2018;27(Suppl 1):129-38.



18. Faundez AA, Richards J, Maxy P, et al. The mechanism in junctional failure of thoraco-lumbar fusions. Part II: Analysis of a series of PJK after thoraco-lumbar fusion to determine parameters allowing to predict the risk of junctional breakdown. Eur Spine J 2018;27(Suppl 1):139-48.



19. Laouissat F, Sebaaly A, Gehrchen M, et al. Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J 2018;27:2002-11.



20. Amabile C, Le Huec JC, Skalli W. Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J 2018;27:458-66.


21. Scheer JK, Fakurnejad S, Lau D, et al. Results of the 2014 SRS Survey on PJK/PJF: a report on variation of select SRS member practice patterns, treatment indications, and opinions on classification development. Spine (Phila Pa 1976) 2015;40:829-40.

22. Kim JH, Lenke LG, Shaffrey CI, et al. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: a systematic review. Spine (Phila Pa 976) 2012;37(22 Suppl):S144-64.