 |
 |
- Search
|
|
||
Abstract
Objective
The safety and clinical usefulness of minimally invasive scoliosis surgery (MISS) has been reported in various studies. However, freehand pedicle screwing in MISS remains technically challenging. The purpose of this study is to evaluate the accuracy and safety of pedicle screw placement using the freehand technique in adolescent idiopathic scoliosis (AIS) patients treated with MISS compared to conventional open scoliosis surgery (COSS).
Methods
We included 76 patients who underwent deformity correction for AIS. Computed tomography scans were used to assess screw violations divided into 2 groups according to the surgical technique: MISS or COSS. Anterior violations were classified into grade 0, 1 (no contact with internal organs), and 2 (contact with internal organs). Medial and lateral violations were classified into grade 0, 1 ( < 2 mm), and 3 ( ≥ 2 mm). grade 2 were considered critical violations.
Results
A total of 630 and 1,174 pedicle screws were inserted in the MISS and COSS groups, respectively. The overall critical violation rates of the MISS and COSS groups were 16.8% (106 screws) and 14.0% (165 screws) (p = 0.116). Medial critical violations on the left side in the middle thoracic region frequently occurred in the MISS group compared to the COSS group (p = 0.003). There were no statistical differences in the complications.
In recent decades, spine surgeries with minimally invasive surgical techniques have been applied to various spinal fields including scoliosis surgery [1]. In minimally invasive scoliosis surgery (MISS), pedicle screw insertion and correction maneuvers are performed through small 2 incisions 4 cm in length and previous studies reported that MISS for adolescent idiopathic scoliosis (AIS) showed acceptable radiological and clinical effects [2,3]. The freehand technique of pedicle screw insertion is preferable to decrease the radiation exposure that takes place more in MISS surgery due to its narrow surgical fields. However, the freehand technique of pedicle screwing in MISS has many difficulties in identifying the entry point compared to open surgery because of the limited visualization of anatomical structures underneath unincised skin. Maintaining accurate 3-dimensional trajectory in MISS also is difficult due to the limited retraction of surrounding soft tissue that interferes with proper direction orientation and positioning of probing instruments for pedicle screwing.
To the best of our knowledge, there have been few studies on the accuracy of pedicle screwing using the freehand technique in MISS.
Therefore, the authors intended to primarily examine the differences in the accuracy and safety of freehand pedicle screwing and complications in MISS through a comparative study with conventional open scoliosis surgery (COSS). Second, differences in the accuracy and safety of inserted screws with the freehand technique according to the anatomical region of the spine in MISS were evaluated.
This is a retrospective comparative study conducted at a single institution. This study was approved by the Institutional Review Board of Korea University Guro Hospital (2022GR0135). Written informed consent was obtained from the patients. From 2014 to 2020, among the 350 patients who underwent deformity correction surgeries for AIS with typical right thoracic curve, 76 patients who underwent pre- and postoperative computed tomography (CT) scans are included in this study. The patients with neuromuscular scoliosis, syndromic scoliosis, and idiopathic scoliosis with atypical curve such as left thoracic curve were excluded. Of them, 28 patients underwent surgeries using minimally invasive surgical techniques (MISS group) (Fig. 1), while 48 patients underwent surgeries using conventional techniques (COSS group). In all patients, sex, age, height, and weight were measured to identify individual characteristics between the groups. The types of scoliosis (King-Moe and Lenke classifications), fusion levels, and curve flexibility were identified and measured using plain radiography.
In the prone position, planned upper and lower instrumented vertebrae were confirmed using fluoroscope. After drawing a line connecting the center of the upper and lower vertebrae, the line was divided into upper and lower halves. An incision of 4 cm was performed at the midpoint of each site.
Following skin incision and thoracolumbar fascial exposure, skin and subcutaneous tissue were retracted using right angle retractor. Paraspinal muscle was dissected until lamina and lateral side of facet joint was exposed.
In all the enrolled patients, pedicle screws were inserted using the freehand technique which uses the base of the facet joint as a landmark for entry [4]. The entry point for pedicle screws in the thoracic spine is the lateral third of the lower border of the superior articular process, while the entry point in the lumbar spine is just lateral to the base of the facet joint [5]. After confirming the entry point with the eyes, a hole was created at the entry point using a drill. A trajectory was created perpendicular to the surface of the superior articular process using curved-shape probe, and a pedicle screw was inserted through the screw pathway [6].
Screw lengths of 25–30 mm were inserted into the upper thoracic vertebrae (T1–3), 30–35 mm in the middle thoracic vertebrae (T4–9), 35–40 mm in the lower thoracic vertebrae (T10–12), and 40–45 mm in the lumbar vertebrae. In the case of MISS, a guide pin was inserted through the screw pathway and 5.0–6.0 mm diameter cannulated screws were then inserted along the guide pin. In the case of COSS, a non-cannulated screw with a diameter of 4.0–6.0 mm was inserted.
The accuracy and safety of the inserted pedicle screws were evaluated using postoperative CT scans. To minimize the effect of metal scattering around the screw, the CT image was adjusted to the bone setting (2,000 HU window width and 500 HU window level) [7]. The measurement was made dividing the groups into screws inserted into the thoracic and lumbar regions. Screws inserted into the thoracic vertebrae were divided again into the upper (T1–3), middle (T4–9), and lower (T10–12) thoracic regions [8].
Violation of the pedicle screw was evaluated in 2 ways. First, the medial and lateral violations of the pedicle screw were defined as invasion of the medial and lateral cortices of the pedicle. Depending on the degree of violation of the screw into the medial and lateral cortical walls of the pedicle, it was classified as grade 0 (if there was no violation of the pedicle), grade 1 (pedicle violation of less than 2 mm), and grade 2 (violation of more than 2 mm). Second, the anterior violation of the pedicle screw was evaluated based on the position of the screw tip and graded as 0, 1, 2 – grade 0 is inside the vertebral body, grade 1is outside the vertebral body, but no contact with internal organs, and grade 2 is outside the vertebral body with contact with internal organs. All types of grade 2 violations were defined as “critical violations” [9-11].
CT evaluations were performed by a spine-trained orthopedic surgeon (YN) and a general orthopedic surgeon (SL) on 2 different occasions (2 weeks apart) to determine inter- and intraobserver reliabilities. Two observers held a consensus meeting prior to each evaluation. After the second evaluation, both observers had a final meeting to decide on the violation grades. If both observers agreed on the grade, this grade was used. If there was a discrepancy between the observers, the higher grade was used. The interobserver reliability between the 2 observers was moderate (κ= 0.534) at the first evaluation and substantial (κ= 0.744) at the second evaluation. The intraobserver reliability of the observers was substantial (κ= 0.645, 0.702).
After surgery, complications such as hemothorax, infection, wound dehiscence, and neurological deficit were evaluated. Reoperation due to screw malposition was also evaluated.
Data analysis was performed using the IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Student t-test was used for the analysis of continuous variables, and the chi-square test and Fisher exact test were used for the analysis of categorical variables. Statistical significance was set at p< 0.05. Inter- and intraobserver reliability were evaluated using Cohen kappa.
There were no statistically significant differences between the 2 groups in age, height, weight, body mass index, curve type, preoperative Cobb angle, and flexibility of the curve (all p> 0.05). There was a difference in sex between the 2 groups (p= 0.046). Detailed demographic data are presented in Table 1.
A total of 1,804 pedicle screws were analyzed using CTs. Among them, 630 pedicle screws were inserted in the MISS group and 1,174 pedicle screws in the COSS group.
In the MISS group, 14, 320, 168, and 128 screws were inserted in the upper thoracic, middle thoracic, lower thoracic, and lumbar vertebrae, respectively. In the COSS group, 71, 555, 280, and 268 screws were inserted in the upper, middle, lower thoracic, and lumbar vertebrae, respectively. Table 2 provides details on the anatomical regions and the proportion of pedicle screws for each group.
In the MISS group, 106 out of 630 pedicle screws (16.8%) were identified as critical violations. In the COSS group, 165 of the 1,174 pedicle screws (14.0%) were identified as critical violations. There was no difference in the rate of critical violations between the 2 groups (p= 0.116). When divided by the direction of critical violations, lateral critical violations occurred most frequently as seen in 74 cases (11.7%) in the MISS group and 121 cases (10.3%) in the COSS group (p= 0.348). Medial critical violations were the next most frequent occurrence in the MISS group as seen in 30 cases (4.8%) and in 39 cases in the COSS group (3.3%) (p= 0.128). Anterior critical violations occurred in 8 cases (1.3%) in the MISS group and 19 cases (1.6%) in the COSS group (p= 0.561) (Table 3).
In the thoracic region, medial critical violations occurred more frequently in 28 cases (5.6%) in the MISS group compared to the 27 cases (3.0%) in the COSS group (p = 0.016). There was no difference in the anterior and lateral critical violation rates between the 2 groups (p = 0.334, p = 0.401). In the lumbar region, there was no difference in the critical violation rate in every direction between the 2 groups (Table 4).
In the thoracic regions, there was no difference in the medial critical violation rate between the 2 groups of the upper and lower thoracic regions. In the middle thoracic region, medial critical violations occurred more frequently as seen in 25 cases (7.8%) in the MISS group than the COSS group with 16 cases (2.9%) (p = 0.010) (Table 4). Among the critical violations in the middle thorax, screws on left side exhibited a difference in critical violations (p= 0.003) (Table 4). The medial critical violation rate of the inserted screw at each level is shown in Fig. 2.
There were no postoperative neurologic deficits or revision surgeries due to screw malposition. There was no difference in complications such as hemothorax, wound dehiscence, and infection between the 2 groups (Table 5).
The safety and clinical usefulness of MISS surgery has been reported in various studies [12]. However, because of the limited surgical fields of view creating difficulty in identifying and maintaining the pedicle screw trajectory, freehand pedicle screwing in MISS surgery remains technically challenging. In MISS, 2 skin incisions of 4 cm in length are used for pedicle screw insertion and correction maneuvering of the curve. Due to the 4-cm incision, the surgical field consisting of only the 4-cm skin-incised area creates difficulty in identifying the entry point and trajectory due to other areas underneath the skin that are unincised. As a result, the accuracy of the pedicle screw in MISS can be quite different from that of open scoliosis surgery. Therefore, the authors conducted a study related to the accuracy of the pedicle screw according to the anatomical region of the vertebral body in MISS [13].
The critical violation rate of inserted pedicle screws in the MISS group was 16.8%, which was slightly higher compared to the COSS group (14.0%) with no statistical significance. The critical violation rate of 16.8% in the MISS group is considered to be similar to the violation rate of 10% to 12% reported in COSS in previous studies [9,11].
Eight cases (1.2%) of critical anterior violations occurred in the MISS group. The pedicle screws with anterior critical violations were in contact with the lung in 7 cases and the psoas muscle in 1 case of the MISS group. However, no signs of injury such as hemorrhage were identified in the internal organs. During the follow-up, no complications requiring reoperation or repositioning of screws developed. According to previous studies, screws that are in contact with organs do not always cause complications [9,14,15]. However, the thoracic aorta and the esophagus on the left side and the azygous vein and inferior vena cava on the right side of the vertebral column were at the greatest risk for injury in anterior violations [16]. There was no statistical difference in anterior critical violations between the MISS and COSS groups (p= 0.561).
In the MISS group, 30 cases (4.8%) of critical medial violations occurred. Medial critical violations occurring in the thoracic spine were identified in 28 cases (11 cases on the right side and 17 cases on the left side). However, none of the 28 patients exhibited neurological symptoms. According to a study by Liljenqvist et al. [17], the safety space for the spinal cord in scoliosis changes according to the concavity with the maximum width of the safety space being approximately 5 mm on the convex side. Due to this wide safety margin on the convex side of scoliosis patients, no neurological injuries developed. In this study, neurological deficits were not observed despite screw violations into the medial wall of the pedicle by more than 2 mm. This could be explained by shifting of the dura mater and spinal cord on the side of the screw [18].
Twenty-five cases of critical medial violations occurred in the middle thoracic region. It is interesting that screws only on the left side exhibited differences with statistical significance (p= 0.003). The possible explanation for the common development of critical violations in the left side of the middle thorax are as follows: firstly, the left side of the middle thoracic region is close to the apical vertebra of the concave side where the vertebral column is most severely rotated placing it more vulnerable to medial violations with high convergent screw trajectories. Secondly, the middle thoracic vertebrae are located distal to the skin incision, making approaches difficult with limited visualization of the surgical field (Fig. 3A, B). Narrow surgical fields and soft tissue obstacles interfere with the proper positioning for screw trajectories and probing of the hole with ball tips. For palpation of the continuity of medial wall of the pedicle with ball tip probes, the probes require convergent angles and sufficient soft retraction (Fig. 4A–C). As a result of higher convergent screw trajectories and narrow surgical fields with difficult soft tissue retraction, the safety of the medial wall of the pedicle could not be clearly confirmed and may have resulted in a higher rate of medial wall violations of the left side of the middle thoracic region.
In the MISS group, lateral critical violations occurred in 74 cases (11.7%), but there were no complications after surgery. There was no statistically significant difference, even when compared with the COSS group. When additionally classified by anatomical region, lateral critical violations occurred more frequently in the thoracic region (13.3%) compared to the lumbar region (5.5%). Lateral critical violations in the thoracic region are not “critical” because the lateral pedicle wall at the thoracic region is covered with a rib. Therefore, surgeons tend not to mind lateral violations that occur in the thoracic region.
This study demonstrated the accuracy and safety of pedicle screws using freehand techniques in MISS compared to COSS, but there were limitations. Not all patients who underwent surgeries were included, only patients who underwent both preoperative and postoperative CT scans. The retrospective design and small sample size, especially in the upper thoracic region, limits the statistical power.
Pedicle screws using the freehand technique in MISS provide similar accuracy and safety when compared with COSS. MISS could be a safe option for the treatment of AIS. Pedicle screws inserted on the left side of the thoracic region, especially the middle thoracic region, exhibited more medial critical violations in the MISS group. Cautious placement of pedicle screws is recommended when inserting pedicle screws into the left side of middle thoracic regions in MISS.
NOTES
Fig. 1.
A 21-year-old female with a Lenke type 3 curve. Twenty-six pedicle screws were inserted from T4 to L4. The surgery was performed through 2 skin incisions.
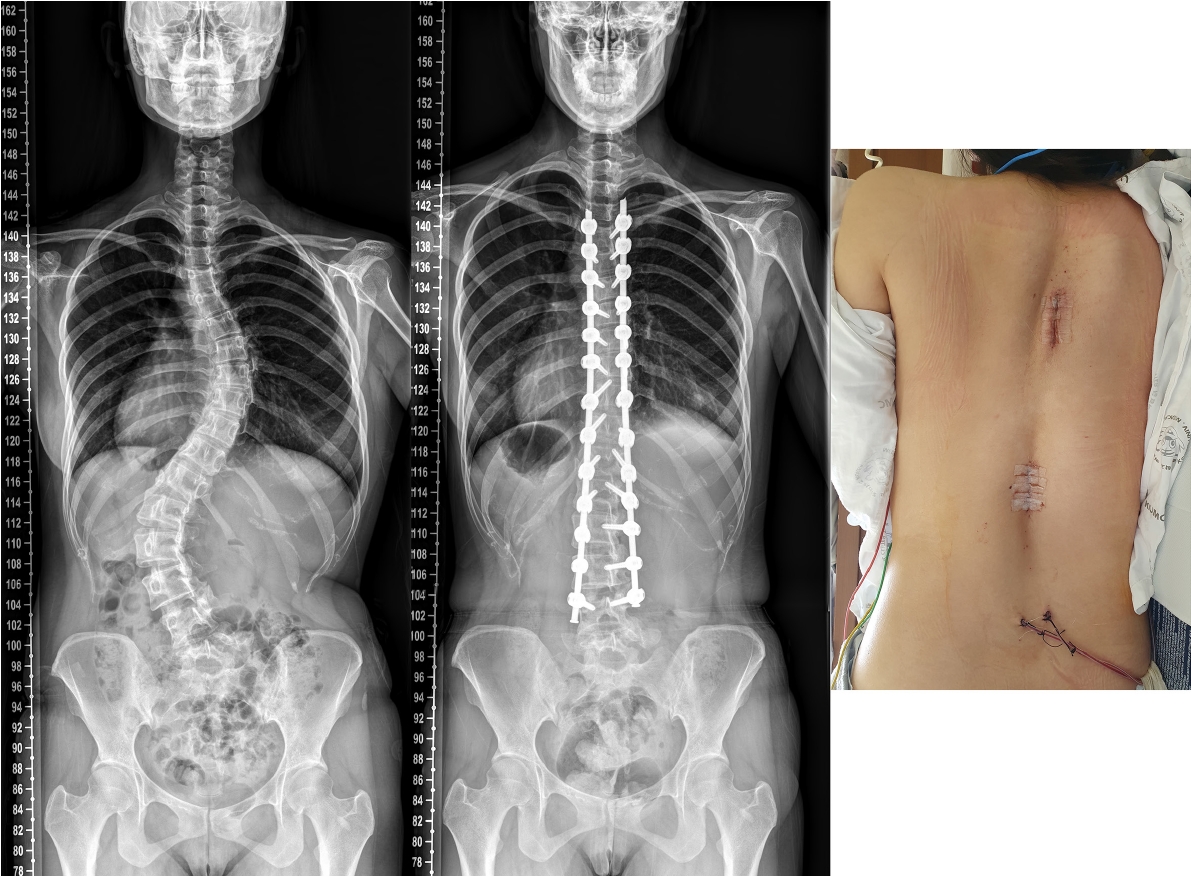
Fig. 2.
The medial critical violation rate of pedicle screw insertions from T1 to L5. The screws inserted in T8 on the left side show a statistically significant difference between minimally invasive scoliosis surgery (MISS) and conventional open scoliosis surgery (COSS).

Fig. 3.
(A) Illustration of the scoliosis curve and location of skin incisions in minimally invasive scoliosis surgery. (B) Visibility is obtained just below the skin incision. However, there is a possible blind spot in the middle thoracic region between the 2 skin incisions.
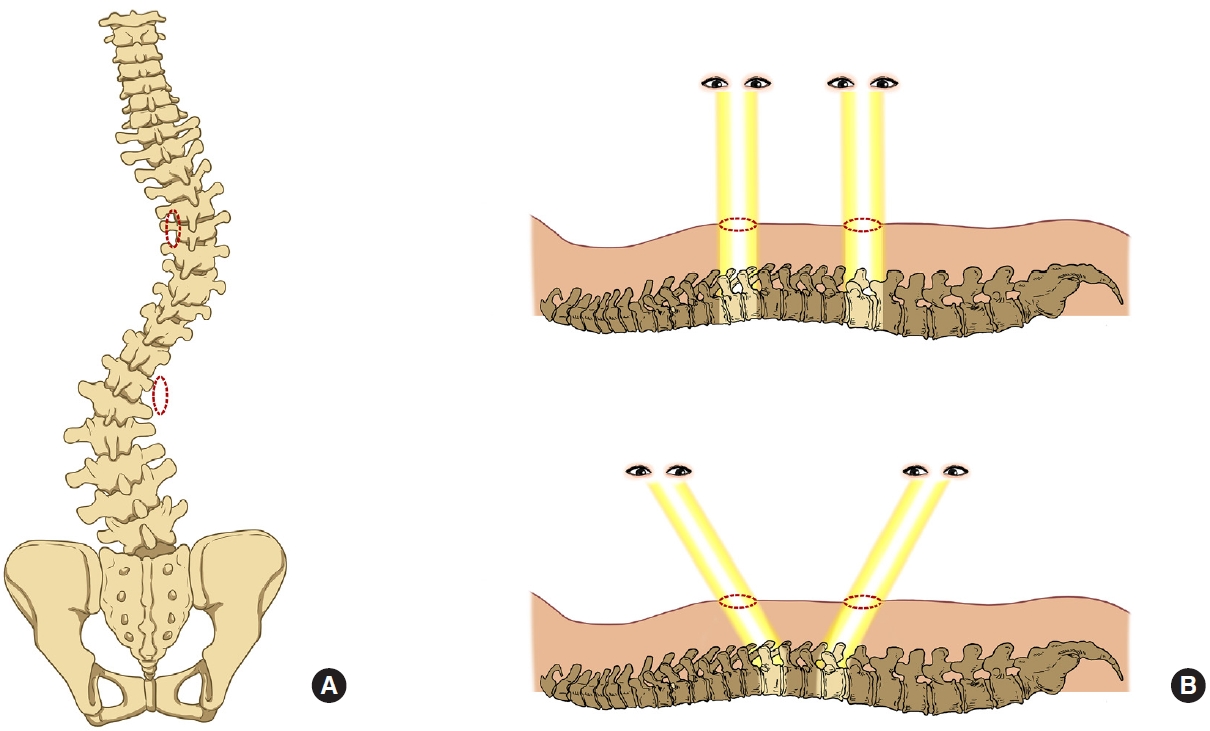
Fig. 4.
(A) The ideal trajectory of the pedicle screw (dotted line) is located toward the left of the skin incision. (B) The surgeon can check the medial wall violation using a ball tip probe without soft tissue tension as seen in conventional open scoliosis surgery. (C) Soft tissue tension acts as an obstacle for the ball tip probe in identifying medial wall violations in minimally invasive scoliosis surgeries (cross-mark).
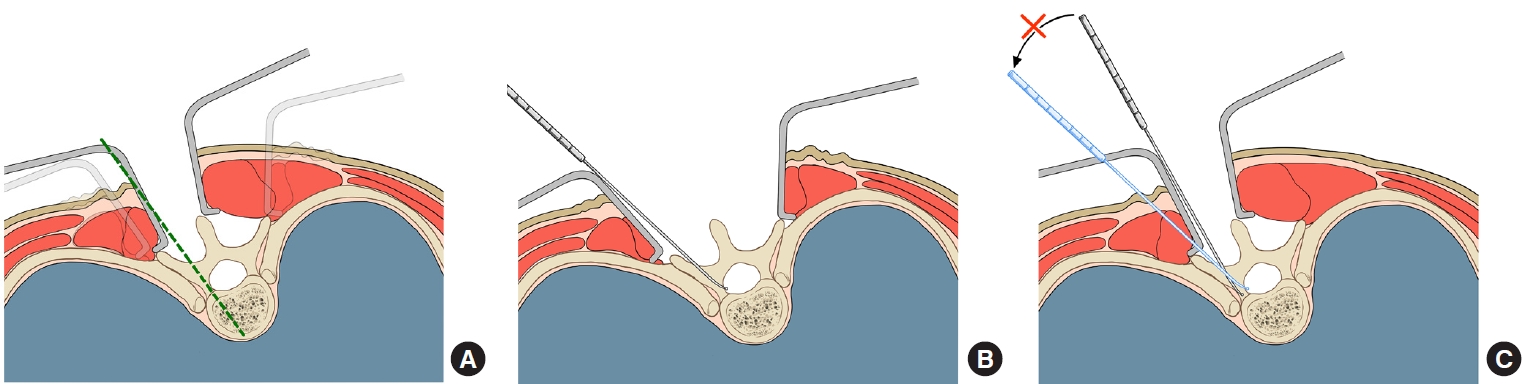
Table 1.
Demographic data of the patients
Table 2.
Number and proportion of inserted pedicle screws by anatomical region
Table 3.
Number of critical violations and critical violation rate by the direction of the violation
| Direction | MISS group | COSS group | p-value |
|---|---|---|---|
| Anterior | 8 (1.3) | 19 (1.6) | 0.561 |
| Medial | 30 (4.8) | 39 (3.3) | 0.128 |
| Lateral | 74 (11.7) | 121 (10.3) | 0.348 |
| Overall | 106 (16.8) | 165 (14.0) | 0.116 |
Table 4.
Number of critical violations and critical violation rate by anatomical region
REFERENCES
1. Park J, Ham DW, Kwon BT, et al. Minimally invasive spine surgery: techniques, technologies, and indications. Asian Spine J 2020;14:694-701.




2. Yang JH, Chang DG, Suh SW, et al. Safety and effectiveness of minimally invasive scoliosis surgery for adolescent idiopathic scoliosis: a retrospective case series of 84 patients. Eur Spine J 2020;29:761-9.



3. Yang JH, Kim HJ, Chang DG, et al. Minimally invasive scoliosis surgery for adolescent idiopathic scoliosis using posterior mini-open technique. J Clin Neurosci 2021;89:199-205.


4. Modi HN, Suh SW, Fernandez H, et al. Accuracy and safety of pedicle screw placement in neuromuscular scoliosis with free-hand technique. Eur Spine J 2008;17:1686-96.




5. Chung KJ, Suh SW, Desai S, et al. Ideal entry point for the thoracic pedicle screw during the free hand technique. Int Orthop 2008;32:657-62.



6. Kim TH, Lee SH, Yang JH, et al. Clinical significance of superior articular process as a reference point for free-hand pedicle screw insertion in thoracic spine. Medicine (Baltimore) 2018;97:e9907.



7. Stradiotti P, Curti A, Castellazzi G, et al. Metal-related artifacts in instrumented spine. Techniques for reducing artifacts in CT and MRI: state of the art. Eur Spine J 2009;18 Suppl 1(Suppl 1):102-8.



8. Kim YJ, Lenke LG, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976) 2004;29:333-42.


9. Kwan MK, Chiu CK, Gani SMA, et al. Accuracy and safety of pedicle screw placement in adolescent idiopathic scoliosis patients: a review of 2020 screws using computed tomography assessment. Spine (Phila Pa 1976) 2017;42:326-35.

10. Rao G, Brodke DS, Rondina M, et al. Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg 2002;97:223-6.


11. Samdani AF, Ranade A, Sciubba DM, et al. Accuracy of free-hand placement of thoracic pedicle screws in adolescent idiopathic scoliosis: how much of a difference does surgeon experience make? Eur Spine J 2010;19:91-5.



12. Neradi D, Kumar V, Kumar S, et al. Minimally invasive surgery versus open surgery for adolescent idiopathic scoliosis: a systematic review and meta-analysis. Asian Spine J 2022;16:279-89.



13. Wu C, Deng J, Li T, et al. Percutaneous pedicle screw placement aided by a new drill guide template combined with fluoroscopy: an accuracy study. Orthop Surg 2020;12:471-9.




14. Belmont PJ Jr, Klemme WR, Dhawan A, et al. In vivo accuracy of thoracic pedicle screws. Spine (Phila Pa 1976) 2001;26:2340-6.


15. Di Silvestre M, Parisini P, Lolli F, et al. Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976) 2007;32:1655-61.


16. Vaccaro AR, Rizzolo SJ, Balderston RA, et al. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am 1995;77:1200-6.


- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























