A Surgical Method for Determining Proper Screw Length in ACDF
Article information
Abstract
Objective
We describe a surgical tool that uses the distractor pin as a reference for determining proper screw length in ACDF. It is critical that screw purchase depth be as deep as possible without violating or penetrating the posterior cortical wall, which ensures strong pull out strength.
Methods
We enrolled 81 adult patients who underwent ACDF using an anterior cervical plate from 2010 to 2012. Patients were categorized into Groups A (42 patients: retractor pin used as a reference for screw length) and B (39 patients: control group). Intraoperative lateral x-rays were taken after screwing the retractor pin to confirm the approaching vertebral level. The ratio of retractor pin length to body anteroposterior (A-P) diameter was measured as a reference. Proper screw length was determined by comparison to the reference.
Results
The average distance from screw tip to posterior wall was 3.0±1.4mm in Group A and 4.1±2.3mm in Group B. The ratio of screw length to body sagittal diameter was 86.2±5.7% in Group A and 80.8±9.0% in Group B. Screw length to body sagittal diameter ratios higher than 4/5 occurred in 33 patients (90%) in Group A and 23 patients (59%) in Group B. No cases violated the posterior cortical wall.
Conclusion
We introduce a useful surgical method for determining proper screw length in ACDF using the ratio of retractor pin length to body A-P diameter as a reference. This method allows for deeper screw purchase depth without violation of the posterior cortical wall.
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is an established procedure for treatment of degenerative cervical disease. Anterior cervical plating and screw fixation devices reduce the risk of non-union and hardware failure after ACDF5,7,14). To achieve successful anterior cervical plate and screw fixation, screws must have strong pull out strength. Many biomechanical studies have focused on this issue specifically. Chen IH reported that subcortically and bicortically purchased screws showed comparable stability before cyclic loading. Cyclic loading deteriorated the construct-bone relationship in both groups, yet bicortically purchased screws rendered additional stability in anterior cervical plating3,4,12). Plates without locking screws require standard cortical screws and bicortical purchase is recommended1,2). Current anterior cervical plate systems, however, are developed with locking fixation screws, which enhance fixation rigidity and pull out strength. This means that locking screws do not require penetration of the posterior vertebral cortex7,8,9,13). Because pull out strength is directly correlated with the vertebrae body antero-posterior (A-P) diameter, longer subcortical screws are crucial for the ACDF procedure14). However, deeper screw depth increases the risk of posterior cortical bone violation and can increase complications such as dural perforation, epidural hematoma, and spinal cord injury. Therefore, achieving the correct screw purchase depth without violating or penetrating the posterior cortical wall is critical. We recently developed a surgical method for this purpose. In this study, we compared our surgical method to a control group in a retrospective manner. We investigated the effectiveness of this surgical method for achieving proper screw purchase depth during ACDF procedures.
MATERIALS AND METHODS
We enrolled 81 adult patients who underwent ACDF using an anterior cervical plate at our hospital between 2010 and 2012. The patients had herniated cervical discs between levels one and three. Patients were categorized into Groups A (42 patients with retractor pins as a reference for screw length) and Group B (39 patients in the control group). Data were collected retrospectively by a single examiner using standardized data collection forms. Patient demographics indicated that there were no significant differences between the two groups (Table 1).
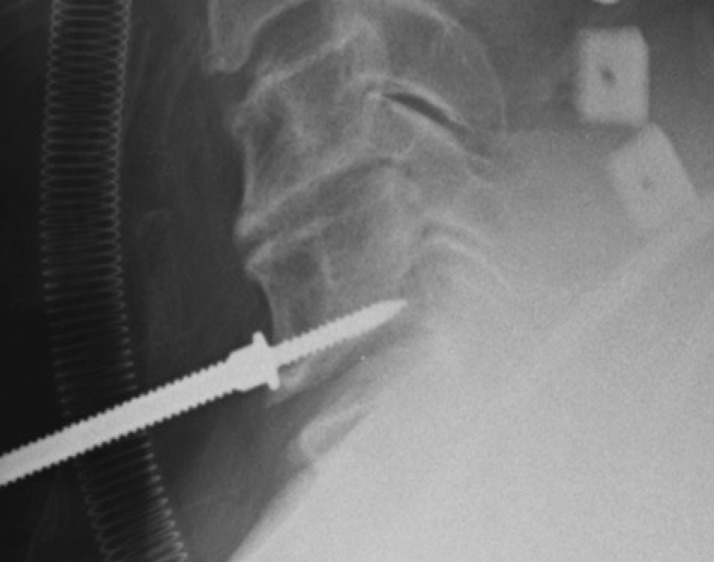
An intraoperative lateral x-ray was performed after the placement of one retractor pin to confirm the approaching vertebral level (Fig. 1). The distance between the tip of the retractor pin and the posterior cortical wall was measured as a reference to be used when deciding proper screw length for ACDF procedures. The purpose of this procedure was to select the longest length of screw possible for obtaining strong pull out strength without penetrating the posterior cortical wall. In Group B, level marking was performed by conventional methods such as disc space needling without retractor pinning. Retraction of each vertebrae was done with the vertebrae spreader. Screw length was determined by measuring the AP diameter in CT scan and the experience of the surgeon about the height, body weight and gender of the patient.
RESULTS
Because the actual length of threaded portion of the retractor pin is uniform(16mm), the ratio of the retractor pin to A-P diameter could be used as a reference value. If the percentage of purchased depth was more than 90% compared to the A-P diameter or if it penetrated the posterior wall, we used 14-mm screws; this occurred in 10 cases. If the depth was less than 90%, we used 16-mm screws; this occurred in 32 patients within Group A. The average distance from screw tip to posterior wall was 3.0±1.4mm in Group A and 4.1±2.3mm in Group B. The ratio of screw length to body A-P diameter was 86.2±5.7% in Group A and 80.8±9.0% in Group B. The ratio of screw length to body A-P diameter over 4/5 was 33 (90%) in Group A and 23 (59%) in Group B (Table 2). Patients in Group A were statistically more likely to have a higher ratio than Group B with an odds ratio of 6.6. There were no cases where the posterior cortical wall was violated in either group. There was only one case of disc space violation by a retractor pin in Group A(Fig. 2, 3). Fortunately, the violated disc was the lesion to be taken diskectomy and fusion and hardware-related complications did not occur in this case.
DISCUSSION
Orozcor and Llovet first approved the use of anterior cervical plate stabilization for fixation of the traumatically unstable spine in 197011). The use of anterior cervical plating devices enhance spinal stability in ACDF procedures. These plates offer advantages such as improved fusion rate and lower risk of graft failure5). Caspar et al. developed commercially available screw and plate fixation in 1989. This was an important addition to surgical treatment of cervical trauma. Caspar and Goffin emphasized the importance of penetration to the posterior vertebral body cortex for enhancing stability. Caspar reported a 5% incidence of screw pull out related to poor purchase in the posterior cortical bone of the vertebral body2). However, placement of such screws require care to assure that the posterior cortex is engaged but that the screws do not enter too deeply into the spinal canal.
A new cervical spine locking plate (CSLP) system was developed that consisted of an H-shaped plate anchored with a unicortical screw. The unicortical screw reduces risk of posterior wall penetration and provides sufficient pull out strength compared with a bicortical screw plating system4).
There are multiple factors that influence the strength of anterior cervical screw and plate fixation. These factors include bone mineral density, bone geometry, plate and screw type, and screw length. The most important parameter of pull out strength, however, is screw length. Conrad et al. reported that 1mm of increased screw length translates to 16 N of increased force of pull out in the foam bone model6). For this reason, using the longest screw possible that does not penetrate the posterior cortical wall may be the best method for promoting strong pull out strength without risk of impingement on the spinal cord6,10). In particular, strong pull out strength is required in osteoporotic patients because there needs to be enough ACDF strength for graft fusion.
To date, no literature has focused on surgical techniques of determining proper screw length in ACDF. Surgeons typically select screw length using parameters such as height, body weight, gender, and radiographs. This could result in uncertain or improper length choices. To address this problem, we describe an accurate surgical procedure that utilizes intraoperative radiographs to determine screw length. We employed an additional surgical method that utilizes the ratio of retractor pin length to body A-P diameter as a reference value. Operative X-ray film results in altered magnification. This means that the distance is not completely accurate. Comparing the ratio of the vertebrae body's A-P diameter to the retractor pin length, which is 16-mm in length, can mitigate this limitation. Another problem is that the screws have a cephalad angle of about 15 to 20 degrees. Actual screw purchase depth is somewhat shorter, about 10 to 14 percent shorter than the length of the screw. And the thickness of plate is also considered to effect the actual screw purchase depth. However, the shortening effect is no more than 2-mm in length and this difference should not affect the decision of screw length. In some cases, it is helpful to select 10% longer screw to get much deeper perchase depth.
There is risk of disc space violation at the adjacent level, but this risk can be overcome with meticulous measurements of disc angles during preoperative CT scans. Level needle localization can also be avoided with this method. As Ahmad et al. reported, incorrect needle localization is a relative risk for adjacent level disc degeneration10). Their study demonstrated that incorrectly marked disc levels have 3-fold increased degeneration. Our method of localizing the level by screwing only one retractor pin could avoid adjacent level degeneration caused by incorrect needling.
We show here that the ratio of screw length to body sagittal diameter was much higher in Group A. This means that a stronger pull out strength was obtained in Group A versus B. In summary, we used a retrospective group analysis that compared a surgical tool group with a control group. We were able to make a more accurate screw length decision in Group A, the surgical tool group.
CONCLUSION
Appropriate screw length and angles can be achieved using a retractor pin as a reference. This technique can decrease the risk of injury from mis-level disc needling. Intraoperative lateral x-ray is useful for anterior cervical screw and plate fixation in ACDF.
Notes
The authors have no actual or potetinal conflict of interest in relation to this article.