|
 |
- Search
Abstract
Anterior cervical discectomy and fusion (ACDF) has been performed for degenerative and traumatic cervical diseases to improve pain and neurologic symptoms including sensory change and motor weakness. Infection, however, is a rare complication of ACDF, and late infection is even much rarer. We present a case of late Infection from ACDF C4-5 using Biocompatible Osteoconductive Polymer (BOP) after twenty years in the absence of an esophageal perforation, Zenker's diverticulum, or recent surgery or bacteremia. Late infection from ACDF after 20 years is extremely rare in the literature. However, possibility of such a late complication should be appreciated during the follow-up period and surgical resection will be required for proper treatment.
Anterior cervical discectomy and fusion (ACDF) has been performed for degenerative and traumatic cervical diseases to improve pain and neurologic symptoms including sensory change and motor weakness.
It has a very low infection rate of 0.1% to 1.6%1,2). Most infections occur in the early postoperative period as a result of intraoperative bacterial seeding or postoperative poor wound care.
However late infections may be associated with an esophageal perforation and seeding of the deep prevertebral space with oropharyngeal flora3,4,8,9,11,12). Other causes of late infections associated with implant migration3,4,8,9,11,12), Zenker's diverticulum10) or bacterial seeding from other surgical site or bacteremia7).
We present a case of late Infection from ACDF after twenty years in the absence of an esophageal perforation, Zenker's diverticulum, or recent surgery or bacteremia.
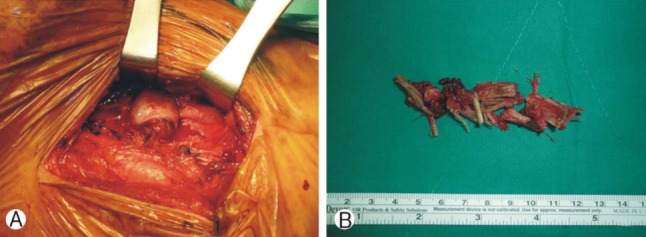
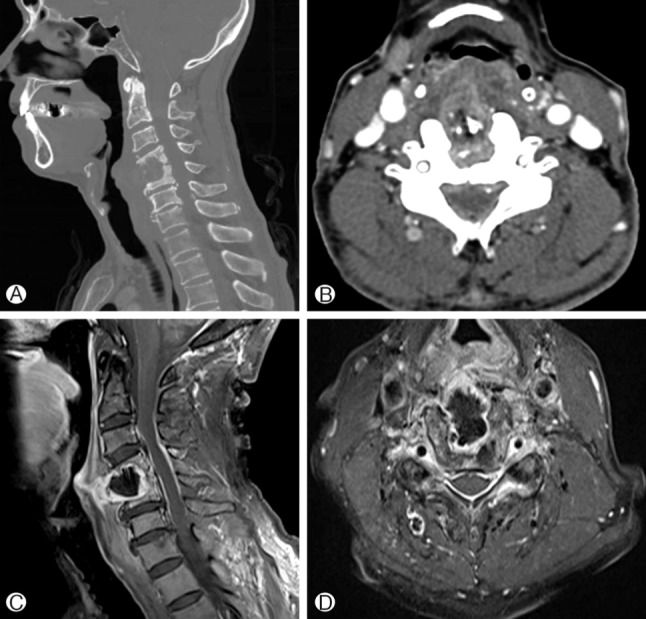
A 74-year-old male patient was referred from department of otolaryngology with the complaint of blood tinged sputum for four months and a laryngeal mass. He did not complain of dysphagia, neck pain, arm pain. Review of the past history revealed that ACDF had been performed for cervical disc herniation at C4-5 using Biocompatible Osteoconductive Polymer (BOP, BOP-DTI Medical) material in other hospital in 1992. He did not have risk factor, such as Diabetes or immunocompromised disease. Systemic examination was unremarkable. Laboratory examination revealed normal levels of erythrocyte sedimentation rate (ESR, 9mm/hr, normal range 0-9), C-reactive protein (CRP, 0.282mg/dL, normal range 0.02-0.3) and white blood cell count (4.40×103/uL, normal range 4.5×103-11.0×103). In laryngoscopic examination, submucosal mass-like lesion was seen at superior part of esophagus entrance (Fig. 1). Plain radiograph showed destruction and collapse of C4 and C5 vertebral bodies (Fig. 2). In neck computer tomography scan and cervical spine magnetic resonance imaging, peripheral enhancing bony destructive lesion (about 2.9×2.0 cm) was demonstrated at C4-5 intervertebral disc space with anterior protrusion to the prevertebral and retropharyngeal spaces at the level of oropharynx and hypopharynx (Fig. 3).
The patient underwent anterior cervical approach in a diagnosis of C4-5 spondylitis with large bony destruction and abscess. During the surgery, gray-yellowish mucoid fluid was evacuated and several pieces of foreign body were removed from the intervertebral disc space of C4-5 (Fig. 4). After thorough debridement, C4 corpectomy and ACDF was performed at C3-5 using mesh cage, plate and screws. Culture revealed no growth of microorganism from the foreign body and surrounding tissues and mucoid fluid. The postoperative course was entirely uneventful. The patient was placed on Flomoxef, Netilmicin, Metronidazole for 11 days. Histopathologic report confirmed chronic active inflammation. Postoperative cervical spine radiographs at 14 months demonstrated complete healing of the graft without any complications (Fig. 5).
Biocompatible Osteoconductive Polymer (BOP) consists of 50% matrix (75% copolymer 1-vinyl 2-pyrrolidone and methyl methacrylate+25% calcium gluconate) and 50% polyamide-6 fibers. It was hypothesized that calcium gluconate as a degradable substance would dissolve after insertion, leaving pores in BOP blocks that would be progressively filled by vascular ingrowth and eventually bony tissue5).
BOP block use in anterior cervical discectomy has now been practised for several years. Recently, its use has declined in many centers due to its high complication rates. BOP block extrusion may be clinically silent and difficult to detect as the graft is radiolucent and only be detectable with the use of CT or MRI6).
McLorinan et al.6) reported a case of acute laryngeal obstruction secondary to BOP block extrusion in a 59-year-old male 10 months after an ACDF.
In the cervical spine procedures, there are several complications, including postoperative hematoma, recurrent laryngeal nerve palsy, Horner's syndrome, dural perforation, worsening of radiculopathy/myelopathy, spinal cord contusion, thoracic duct injury, pneumothorax, vertebral artery laceration, carotid artery or jugular vein injury, graft extrusion, superficial and deep wound infection, epidural abscess, spondylodiscitis, Zenker's diverticulum, pharyngoesophageal perforation, and dysphagia2).
Compared to other spinal regions, wound infections occur rarely after ACDF. Several reports document the incidence of 0.1% to 1.6%2). Even though it is rare, wound infections generally tend to occur in the early postoperative period. If they occur after an interval of time after surgery, the possibility of an associated esophageal perforation should be relatively high. Various symptoms and signs could be presented by wound infections including neck pain, dysphagia, and fever accompanied with laboratory abnormalities such as elevated white blood cells count, ESR, and CRP11).
The presence of spinal implants as a foreign body may be a risk factor for deep, delayed wound infections. Most of spinal implants used today are made of inert metals which have smooth surfaces in order to prevent bacterial adherence7). However, a glycocalyx biofilm, made by pyogenic bacteria, have been known to form on the surface of the foreign body instruments, which facilitates the adherence of bacteria7). That is why a spinal implant in the presence of bacteremia is an important risk factor for postsurgical wound deep infections.
Christiano et al.1) reported late infection in a 54-year-old female 2 years after an ACDF with unicortical cancellous allograft and plate-screw construct. The patient complained dysphagia that complete inability to swallow. She had a low-grade fever of 38℃, a white blood cell count of 11,700, ESR of 32, and CRP of 91. She evaluated a CT, MRI, barium-swallow study for esophageal perforation and performed surgical exploration and debridement. Cultures from the operating room resulted Streptococcus intermedius and the patient was placed on clindamycin for 6 weeks. After surgery, the patient's dysphagia improved remarkably.
Unlike the common findings we mentioned above, our patient showed no other clinical symptoms but only blood tinged sputum, and all the laboratory tests were normal as well.
And there was no evidence of bacteremia. And on the intraoperative culture study collected at the previous operative site, the result was negative as well.
In our case, the cause of infection is elusive. There was no recent infection or surgeries, predisposing medical history, or risk factor that would make him vulnerable to infection. We cannot be ruled out the spontaneous infection. But it would be very unlikely in a healthy, adult patient.
This is a rare case in the absence of implant migration, diverticulum, and other previously reported risk factors for late infection.
However, possibility of such a late complication should be appreciated during the follow-up period and surgical resection will be required for proper treatment.
References
1. Christiano LD, Goldstein IM. Late prevertebral abscess after anterior cervical fusion. Spine 2011 36:E798-E802. PMID: 21289574.


2. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine 2007 32:2310-2317. PMID: 17906571.


3. Geyer TE, Foy MA. Oral extrusion of a screw after anterior cervical spine plating. Spine 2001 26:1814-1816. PMID: 11493857.


4. Lu DC, Theodore P, Korn WM, Chou D. Esophageal erosion 9 years after anterior cervical plate implantation. Surgical Neurology 2008 69:310. -312. discussion 312-313. PMID: 18261766.


5. Madawi AA, Powell M, Crockard HA. Biocompatible osteoconductive polymer versus iliac graft. A prospective comparative study for the evaluation of fusion pattern after anterior cervical discectomy. Spine 1996 21:2123. -2129. discussion 2129-2130. PMID: 8893437.


6. McLorinan GC, Choudhari KA, Cooke RS. Life threatening complication of biocompatible osteoconductive polymer graft after anterior cervical discectomy. Br J Neurosurg 2001 15:363-365. PMID: 11599456.


7. Naderi S, Acar F, Mertol T. Is spinal instrumentation a risk factor for late-onset infection in cases of distant infection or surgery? Case report. Neurosurgical Focus 2003 15:E15PMID: 15347233.

8. Pompili A, Canitano S, Caroli F, Caterino M, Crecco M, Raus L, et al. Asymptomatic esophageal perforation caused by late screw migration after anterior cervical plating: report of a case and review of relevant literature. Spine 2002 27:E499-E502. PMID: 12461406.


9. Solerio D, Ruffini E, Gargiulo G, Camandona M, Raggio E, Solini A, et al. Successful surgical management of a delayed pharyngo-esophageal perforation after anterior cervical spine plating. Eur Spine J 2008 17(Suppl 2):S280-S284. PMID: 18224356.


10. Summers LE, Gump WC, Tayag EC, Richardson DE. Zenker diverticulum: a rare complication after anterior cervical fusion. J Spinal Disord Tech 2007 20:172-175. PMID: 17414989.


11. Violon P, Patay Z, Braeckeveldt J, Pirotte B, Kentos A, Brotchi J, et al. An atypical infectious complication of anterior cervical surgery. Neuroradiology 1997 39:278-281. PMID: 9144677.


12. von Rahden BH, Stein HJ, Scherer MA. Late hypopharyngoesophageal perforation after cervical spine surgery: proposal of a therapeutic strategy. Eur Spine J 2005 14:880-886. PMID: 16151718.


Fig. 1
A laryngoscopic view of the protruded laryngeal mass. There is a submucosal mass-like lesion at superior part of esophagus entrance.
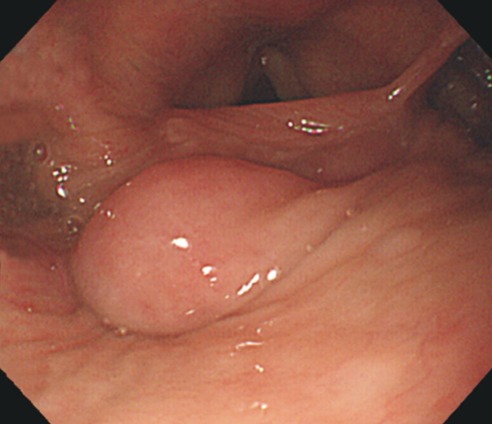
Fig. 3
Cervical spine CT images demonstrating osteolytic lesion in C4 and C5 bodies. Sagittal image (A) and axial image (B). Cervical spine MRI. Gadolinium-enhanced sagittal T1-weighted image (C) and axial T1-weighted image (D) show enhancement of the protruded prevertebral soft tissue and old graft at C4-5.

- TOOLS
-
METRICS

-
- 11 Crossref
- Scopus
- 7,681 View
- 75 Download
- Related articles in NS
-
Journal Impact Factor 3.2