Migration of Rod into Retroperitoneal Region: A Case Report and Review of the Literature
Article information
Abstract
Spinal stabilization with fusion is the widely used method for traumatic or pathologic fracture of spine, spinal stenosis, and spondylolisthesis. Complications may emerge during or after the operations. Infection, hematoma and neurological deficits are early noticed findings. Screw and/or rod fractures present in long-term after surgery. Rod migration in out of the spinal column is a rare entity. A 67-year-old woman was visited our clinic for right leg pain. She had a previous spinal instrumentation surgery for spondylolisthesis in another center 6 years before. After radiological work-up, a distally migrated rod piece was observed in the retroperitoneal portion. The patient was operated for degenerative change; old instruments were replaced and extended to the L2 level with posterior spinal fusion. After the operation, her right leg pain improved. The asymptomatic migrated rod piece has regularly been followed clinically and radiologically, since then. Although it has rarely been reported, migration of the instrumentation material should be kept in mind. Spinal fixation without fusion makes the mechanical system vulnerable to motion effects of spine, especially in a degenerative and osteoporotic background. Long-term, even life-long follow-up is necessary for late term complications.
INTRODUCTION
Spinal stabilization with instrumentation is a widely used method for spinal traumas, degenerative spinal disease, and sometimes at congenital spinal malformations. Complications may occur perioperatively or after surgery, such as soft tissue injuries, neurological deficits, acute respiratory failure, hematomas, infections, failure of fusion, breakage or dislodgement of screw or rod1,4,8,10). Even rod migration through the spinal column may occur8). We are describing a case of migrated rod to the retroperitoneal area proven with radiological imaging modalities. In the literature, a few cases of distal migration of rod have been reported (Table 1)1,2,3,4,5,6,7,8,9,11,12).
CASE REPORT
A 67-year-old woman visited our outpatient clinic in September 2012 with right leg pain persisting for 3 months. She had been operated in another center in 2006 for degenerative lumbar spondylolisthesis. There was no history of trauma or vascular pathology. She was on carbamazepine for trigeminal neuralgia. Her laboratory test results were normal. Physical examination was within normal limits. There was right leg weakness, motor strength of the right lower extremity muscles was as follows: iliopsoas: 3/5, gluteus maximus: 5/5, hamstrings 5/5, quadriceps femoris: 4/5, anterior tibialis: 4/5, extensor hallucis longus: 4/5, extensor digitorum longus: 4/5, gastrocnemius: 5/5, soleus: 5/5, posterior tibialis: 5/5. On the left side; anterior tibialis, extensor hallucis longus and extensor digitorum longus had a motor deficit of 1/5: the other muscle groups were normal in strength. Deep tendon reflexes were normoactive. Also, there was bilateral neurogenic intermittent claudication. On EMG, there were acute right L2, L3 radiculopathic, and chronic bilateral L5-S1 neuropathic findings.
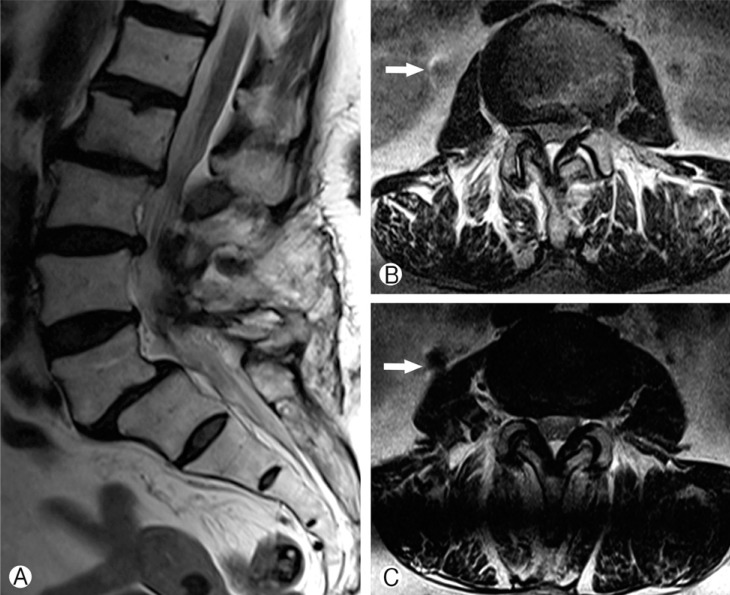
On 2-plane lumbosacral radiography, bilateral transpedicular screws were observed at L5 and S1 vertebral segments. On lateral lumbar X-ray, a linear hyperdense mass, corresponding to a rod piece was lying in front of the vertebral column (Fig. 1A, C). On axial-plane lumbar computed tomography (CT) imaging, the hyperdense foreign body was present between the lower pole of the right kidney and right iliopsoas muscle (Fig. 2C-E). Also, the rod piece on the right side was missing in the screw heads. No fusion mass was observed in the treated segments. On T2-weighted magnetic resonance imaging (MRI), there was L5-S1 spondylolisthesis and intervertebral disc bulging at L2-3 and L3-4 segments. On axial and coronal images, a hypointense linear mass was observed in the same location as in the CT(Fig. 2A, B and Fig. 3). The patient had a previous lumbar A-P/lateral roentgenogram showing the migrated rod in the same location as in the new films (not shown). In the operation, total laminectomies were performed between L3 and L5 vertebrae. The old instrumentation system was replaced with the new one, from L2 to S1; decorticated bone auto-graft was used as fusion mass bilaterally (Fig. 1B, D). The migrated rod piece was present in front of the psoas major muscle. To extract the rod piece, an additional anterior approach was necessary. After the operation, the patient's symptoms related to spinal stenosis diminished. There were no symptoms for the migrated rod piece. The rod piece had been in the same location for 3 years. We put her on regular clinical and radiological follow-ups. At her 12th month follow-up period, she did not have any spinal complaints; she was asymptomatic for the migrated rod piece and her X-rays showed fusion of the lumbosacral spine.
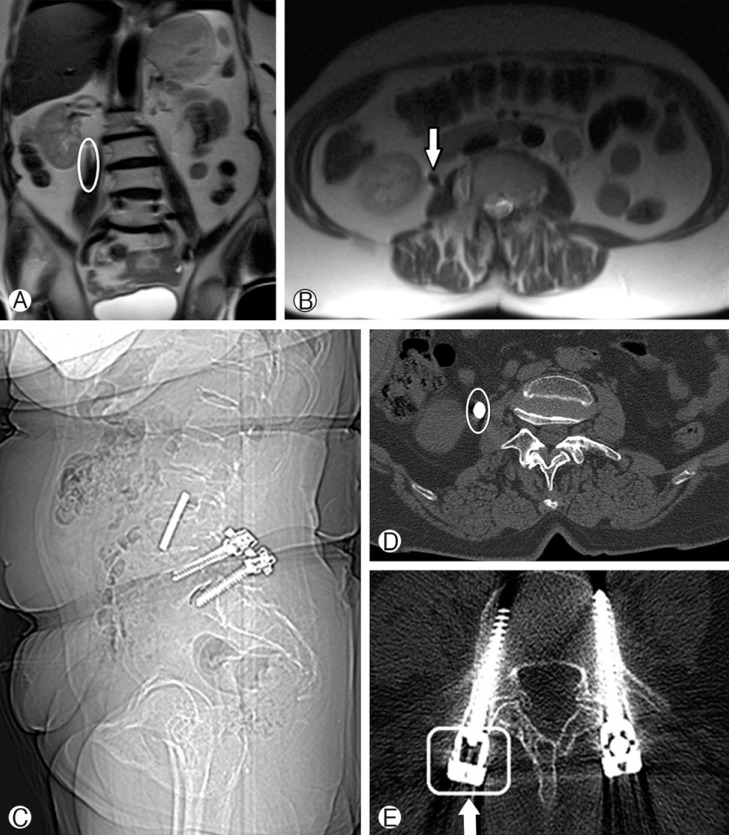
Migrated rod piece has a lower signal intensity and is present near the right kidney on MRI (small white arrow) (A, B). Appearance of hyperdense rod fragment in abdominal CT with missing rod piece in right screw head (big white arrow) (C-E).
DISCUSSION
Spinal instrumentation is used to correct spondylotic process and spinal instability secondary to degenerative, traumatic, idiopathic or congenital processes. Acute and late complications may present after spinal stabilization procedures. In long term, broken instrumentations are mostly noticed if fusion does not occur at the surgical sites. Rod fracture incidence is between 2 and 11%4). Its migration out of spinal column is extremely uncommon4,8). When this occurs, it may result in catastrophic outcomes such as visceral and vascular injury4). Al-Binali et al.1) reported a spinal instrumented case with acute lower gastrointestinal bleeding. The rod had migrated through the iliac wing into the pelvis and caused internal iliac artery laceration. In another case reported by Fitchett et al.5) a patient, admitted with acute abdominal pain, was detected to have a painful mass in the right iliac fossa. Harrington rod piece was taken out through an abdominal incision. Distal rod migration to the posterior cranial fossa, lung pleura, and leg has also been notified in the literature3,4,6,11). Sometimes, patients did not have any symptoms and they were diagnosed during their routine clinical controls or they presented with symptoms related to instability due to ineffective arthrodesis like in our case3,8,11). Table 1 presents in detail, distally migrated rod cases with clinical presentations, treatment approaches and instrumentation types used in their previous surgery. Our case was totally asymptomatic for the migrated rod piece.
Improperly tightened screws may loosen and rod may slip from its place with gravity and movements of the body. In our case, the screw heads were very tight. However, fusion mass was not observed in the treated segments. Thus, the rod might have moved due to unbalanced motion at instrumented levels without any fusion3,8,11). This may have led to fatigue of the instrumentation with mobile segments and then may have freed rod piece. The rod fragment might have moved through the iliopsoas muscle, again with the help of body movements. The migrated fragment was in the retroperitoneum near the right kidney. Dhatt et al. proposed that proper spinal fixation with dual rods would compensate rotational, bending and extending forces of the body4). In our case, the rod got loosened and migrated out of spinal column despite dual rod system.
Approximately half of migrated rod cases in the literature had remained asymptomatic4). Some authors preferred follow-up instead of removal of the rod fragment11). In our case, our patient's main complaint was related with spinal stenosis with inadequate previous spinal fusion. We first aimed to decompress the stenotic segments, relieve the nerve roots. For this purpose we used a posterior approach. After revision surgery, patient's symptoms regressed. The migrated rod piece was not broken and did not have sharp ends, which could have more devastating results. Also, it had remained in the same location for 3 years. During this time period, fibrosis may have occurred around the migrated rod piece and would cause vascular injury while taking out it. So, we put her on regular clinical follow-ups. Thus, close follow-up of our patient will continue even if she is symptom-free.
CONCLUSION
Spinal instrumentation with fusion is a very useful technique for spinal column stability. This case showed us that spinal fixation without fusion makes the mechanical system vulnerable to motion effects of spine, especially in a degenerative and osteoporotic background. Although it has been rarely reported, migration of the instrumentation material should be kept in mind. Long-term, even life-long follow-up, is necessary for late complications, if there is no fusion. In a case with distant migration of instruments, surgery for instrument removal should be considered if the patient is symptomatic.
Notes
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.