Clinical Outcomes of Posterior C2-C3 Fixation for Unstable Hangman's Fracture Compared with Posterior C1-C3 Fusion
Article information
Abstract
Objective
To verify the clinical outcomes of posterior C2-C3 fixation for unstable Hangman's fracture compared with posterior C1-C3 fixation.
Methods
Twenty four patients for unstable Hangman's fracture were enrolled between July 2007 and June 2010 in this study. Thirteen patients underwent posterior C2-C3 fusion and 11 patients underwent posterior C1-C3 fusion. Clinical outcomes were evaluated using Neck Disability Index (NDI) scores and Visual Analogue Scale (VAS) scores during preoperative and postoperative follow up period. Plain radiographs were obtained on postoperative 1 day, 1 week, and then at 1, 2, 6, and 12 months. CT was done at postoperative 12 months in all patients for evaluation of bone fusion. The mean period of clinical follow-up was 15 months.
Results
The mean ages were 43.3 years in C2-C3 group and 50.0 years in C1-C3 group. Mean follow-up period was 17.2 months in C2-C3 group and 16.3 months in C1-C3 group. VAS scores and NDI scores in C2-C3 group were much less than those in C1-C3 group at each follow-up period. The differences of VAS score and NDI scores between C2-C3 and C1-C3 groups at each follow-up period were statistically significant (p<0.001) by paired T-test. Solid Bone fusion was confirmed in all cases at the final follow-up.
Conclusion
C2-C3 group showed better clinical and biomechanical results than C1-C3 group in terms of axial pain and disability of neck.
INTRODUCTION
Traumatic spondylolisthesis of the axis, or Hangman's fracture, is a common injury type of high cervical spine and the second most common fracture of axis. It involves bilateral C2 pars interarticularis fracture with a variable degree of displacement of C2 on C3 vertebrae8,21). Although most Hangman's fractures are treated conservatively2,22), surgery is usually preferable in cases of highly unstable Hangman's fracture and fusion failure after rigid arthrodesis3,5,15,21,23). Surgical stabilization has been described using both anterior and posterior approaches17,20,21,26,27). Among the different surgical fixation techniques, posterior screw and rod fixation can offer better results in terms of alignment and stabilization of spine with a low level of pseudoarthrosis than those of anterior plate and screw fixation because anterior approach does not address the detached posterior arch of C2 and instability remained during flexion-extension and axial rotation12). This technique addresses the detached posterior arch of C2 by pinning the fractured pars while simultaneously addressing instability at the disc by immobilizing C2 relative to C3.
Posterior C1-C3 lateral mass screw and rod fixation can provide good alignment and firm stabilization of spine. However, this technique cannot preserve the motion at intact C1-C2 segment. Posterior C2 pedicle - C3 lateral mass screw and rod fixation can be considered to preserve the motion of the axis in cases that direct repair of the pars fracture with a screw across the fracture line is possible3,5,23). The key difference between these two techniques is preservation of C1-C2 motion which may have difference in biomechanical features as well as clinical outcomes. This study was conducted to verify the clinical outcomes of posterior C2-C3 fixation for unstable Hangman's fracture compared with posterior C1-C3 fixation.
MATERIALS AND METHODS
Twenty four consecutive patients with unstable Hangman's fracture were enrolled who required posterior surgical fixation and stabilization using the Polyaxial Screw-rod System (Synapse, Bettlach and Waldenburg, Switzerland) between July 2007 and June 2010. Thirteen patients underwent posterior C2-C3 fixation (C2-C3 group) and 11 patients underwent posterior C1-C3 fixation (C1-C3 group). The medical records of all patients were reviewed. All patients were classified and selected using Classification of hangman's fracture which was proposed by Levine and Edwards to evaluate16,17). Type I has stable and minimal translation (<3mm) without C2-C3 angulation. Type II has unstable disc disruption and significant C2-C3 angulation and translation (>3mm). Type IIA is unstable due to flexion-distraction injury and has more angulation than type 2 without translation. Type III is unstable and has severe C2-C3 angulation and translation. It has sometimes unilateral or bilateral facet dislocation. Surgical stabilization was recommended in Levine-Edwards Type IIa and III fractures with significant dislocation. Surgical treatments were performed in patient who showed poor reduction or nonunion after rigid external orthosis, neurologic deficit or unstable combination fracture at the presentation.
Dynamic plain radiographs were obtained on postoperative day 1, 1 week, and then at 1, 2, 6, and 12 months and Computed Tomographic (CT) evaluation was done at postoperative 12 months in all patients for evaluation of spinal stability and bone fusion. The adequacy of fusion was determined at approximately four, six and 12 months postoperatively. Pseudoarthrosis was defined as a motion >2.0mm between the laminae at the base of the spinous processes of the upper and lowermost fixed and fused levels on the flexion/extension plain radiographs.
Concurrently, clinical outcomes were evaluated using extent of anterior translation, rotation, Visual Analogue Scale (VAS) scores, and Neck Disability Index (NDI) scores during preoperative and every postoperative follow up visit24).
Extent of anterior translation was measured as the distance between parallel lines drawn through the posterior borders of C2 and C3 vertebral bodies (Fig. 1). Range of rotation was measured at final follow up visit when patients turned their neck to look over the both shoulders in a supine position. Postoperative pain was assessed using a 10-point VAS with end-point anchors of no pain (0 points) and severe pain (10 points). The NDI questionnaire is comprised of 10 single items related to activities of daily living. Each item has six predefined response categories, coded 0-5 on an ordinal scale. The scores reflected either the degree of neck pain or the degree of difficulty in performing certain actions due to neck pain. The lowest score (0) represented no problem or pain, whereas the highest score (5) represented maximum problems or pain. Patients who underwent anterior fixation or combined anterior and posterior fixation were excluded. The pre- and postoperative arm and neck symptom VAS scores and NDI scores were compared using two-sample t tests paired for means. A p value of <0.05 was regarded as significant.
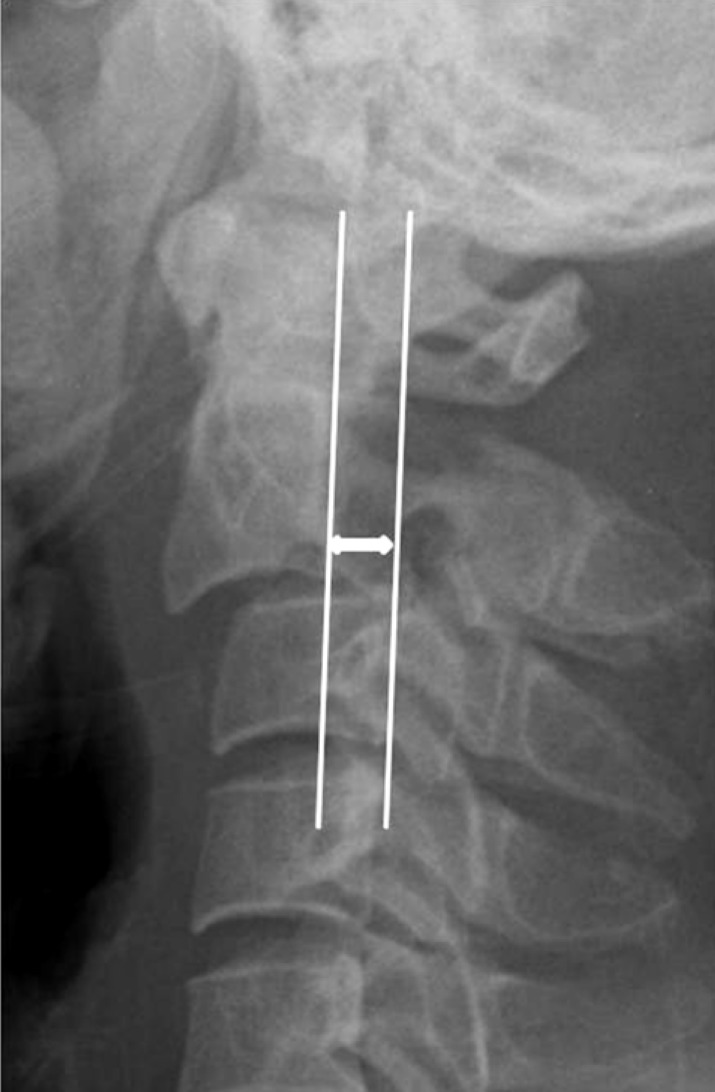
Measurement of anterior translation. The distance between parallel lines drawn through posterior borders of C2 and C3 vertebral bodies.
Inclusion criteria for posterior C2-C3 fixation included as below; linear fracture without bony particles in a gap of fracture, ≤5mm of displacement between C2 and C3, ≤11 degree of angulation between C2 and C3, and no injury of C1. Posterior C1-C3 fixation had been perform in cases with communited fracture of C2 isthmus, >6 mm of displacement between C2 and C3, >12 degree of angulation between C2 and C3, narrow or cortical pedicle of C2, and existence of C1 injury or C1-C2 instability (Fig. 2).
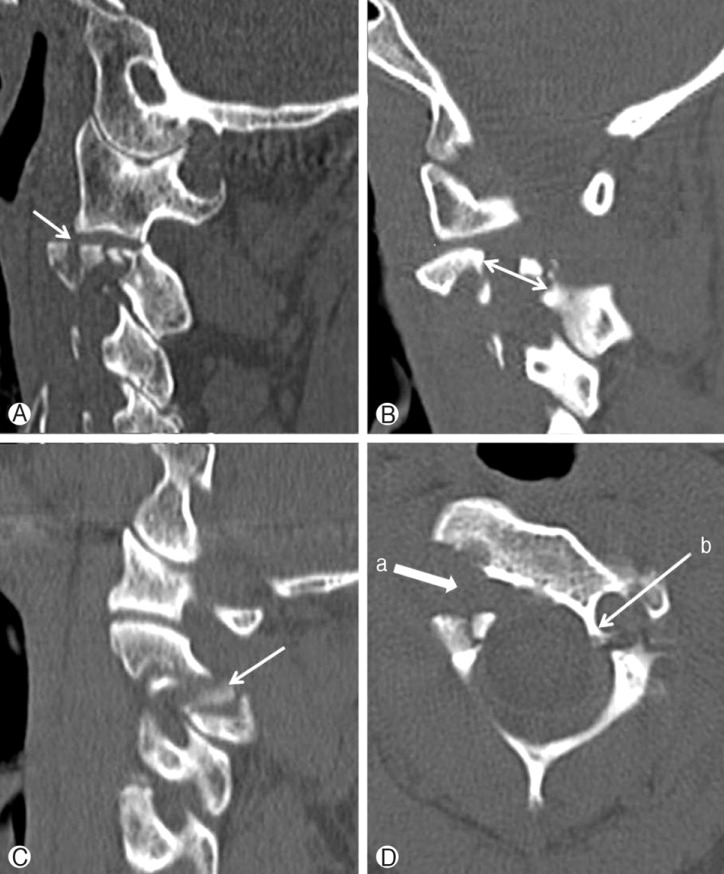
Inclusion criteria for posterior C1-C3 fixation. (A) communited fracture of C2 isthmus, (B) >6mm of displacement between C2 and C3, (C) bony particles in a gap of fracture, (D-a) >12 degree of angulation between C2 and C3, (D-b) narrow or cortical pedicle of C2, and existence of C1 injury or C1-C2 instability.
1. Surgical Technique
The surgery was performed in a consistent fashion. A standard midline incision was made above the C1-C4 levels. The lateral masses were exposed in a subperiosteal fashion to the lateral margins of the facet joints. Once the displacement was reduced, the lateral masses to be fused were decorticated with the drill. Great care was taken not to disturb the capsule at adjacent levels in order to prevent any iatrogenic instability.
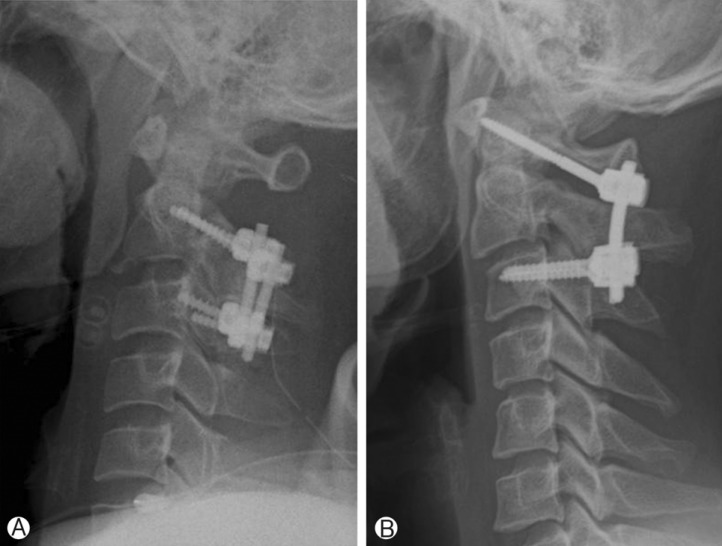
Pedicle screws were used at C2 vertebra and lateral mass screws were used at C3 vertebra under the C-arm guidance for C2-C3 fixation (Fig. 3A). Lateral mass screws were used at C1 and pedicle screws or lateral mass screws were used at C3 vertebra for C1-C3 fixation (Fig. 3B). Pedicle screw insertion for C2 vertebra was done unilaterally or bilaterally as possible. A rod was prepared to the appropriate length and contour that it would easily pass through the heads of all polyaxial screws. Once the rod was positioned, it was secured to the heads of the screws using outer nuts.
Bony fusion was performed by packing allograft bone and demineralized bone matrix (DBM) into the facet joints, around the decorticated lateral masses lateral to the rod and laminae. Bone graft was placed between the posterior arch of C1 and the lamina-spinous process of C2 vertebra after C1-C3 fixation. During the entire procedure, the retractors were intermittently released to avoid denervation of the erector spinal muscles. Routine closure was carried out and drains were left in place as needed.
RESULTS
Twenty four patients were enrolled in this study. Demographic and clinical data of the patients were shown in Table 1. C2-C3 group consisted of 8 men and 5 women whose mean age was 43.3 years (range 29-57). C1-C3 group consisted of 6 men and 5 women whose mean age was 50.0 years (range 26-68). All patients were regularly seen in the follow-up clinic at periodic interval after the procedure. Mean follow-up period was 17.2 months in C2-C3 group and 16.3 months in C1-C3 group. Solid bone fusion was confirmed in all cases at postoperative 1 year follow-up on both C2-C3 and C1-C3 fixation groups (Fig. 4).

Solid bone fusion was confirmed in all cases at postoperative 1 year on both posterior C2-C3 fixation (A) and posterior C1-C3 fixation (B)
The average translations were 4.7±1.16 in C2-C3 group and 8.54±2.34 in C1-C3 group at presentation. The average translations were 1.2±1.02 in C2-C3 group and 2.3±1.57 at final follow-up. Although degree of reduction showed much higher in C1-C3 group, restoration to normal cervical alignment could be achieved in C2-C3 group compared with C1-C3 group at final follow-up.
The average ranges of rotation were 120±6.15° in C2-C3 group and 19.8±3.54° in C1-C3 group at final follow-up.
In C2-C3 group, the average VAS score for neck pain was 8.3±1.1 1 day after the surgery. VAS score was gradually decreased during the follow-up period and the mean VAS score was decreased up to 2.07±0.8 at final follow-up (Fig. 5). In C1-C3 group, the average VAS score for neck pain was 9.45±0.5 1 day after the surgery. VAS score was slowly decreased during the follow-up period and the mean VAS score was decreased up to 3.45±0.7 at final follow-up. VAS scores in C2-C3 group were much less than those in C1-C3 group at each follow-up period. The differences of VAS score between C2-C3 and C1-C3 groups at each follow-up period were statistically significant (p<0.001) by paired T-test.

The postoperative change of VAS scores for neck pain. VAS scores in C2-C3 group were much less than those in C1-C3 group at each follow-up period. The differences of VAS score between C2-C3 and C1-C3 groups at each follow-up period were statistically significant (p<0.001) by paired T-test, except immediate postoperative period.
In C2-C3 group, the average NDI score was 84.1±2.6 1 day after the surgery. NDI score was gradually decreased during the follow-up period and the mean NDI score was decreased up to 22.6±2.8 at final follow-up (Fig. 6). In C1-C3 group, the average NDI score was 89.0±2.1 1 day after the surgery. NDI score was slowly decreased during the follow-up period and the mean NDI score was decreased up to 44.1 ±5.1 at final follow-up. NDI scores in C2-C3 group were much less than those in C1-C3 group at each follow-up period. The differences of NDI score between C2-C3 and C1-C3 groups at each follow-up period were statistically significant (p<0.001) by paired T-test.
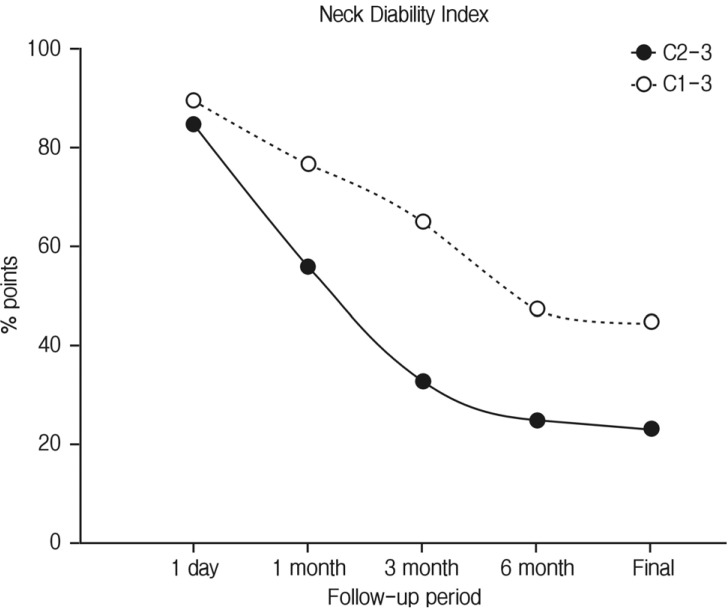
The postoperative change of NDI scores. NDI scores in C2-C3 group were much less than those in C1-C3 group at each follow-up period. The differences of NDI score between C2-C3 and C1-C3 groups at each follow-up period were statistically significant (p<0.001) by paired T-test.
There were one case of wound infection and 1 case of screw loosening in C2-C3 group. Revision surgery for screw repositioning was needed in case of screw loosening. There was no complication in C1-C3 group.
DISCUSSION
Hangman's fracture is the second most common fracture of the second cervical vertebra (C2). It involves a bilateral arch fracture of the C2 pars interarticularis with variable displacement of C2 on C37). Among different classifications for Hangman's fracture, Levine-Edward's is the most frequently used8,9,10,16). Type I lesion is usually considered stable with no angulation and displacement on C2-C3, whereas Types II, IIa, and III are usually considered unstable. These unstable types are combined with the injury of the C2-C3 disc and the anterior longitudinal ligament. In Type II and type III Hangman's fracture, extension forces have been implicated in the disruption of the anterior longitudinal ligament, posterior longitudinal ligament, and C2-C3 disc.
In most cases of Hangman's fracture, the conservative treatment is the most indicated4,6,9,22,23,25). Semirigid collars are used for cases with a small degree of dislocation. Rigid immobilizations such as halo-vest are used for cases of great displacement. In regard to the unstable Hangman's fracture, the treatment is still controversial. Pseudoarthrosis, anterior dislocation, angulation of C2 over C3, and recurrent axial pain were observed in about 60% of the cases of Types II, IIa, and III, which were primarily treated with conservative therapy9,10,22). Majority of authors recently suggested that the presence of discoligamentous injury on top of bony injury would require surgery. Another reason for surgery is the shortening the course of treatment3,4,18,21,23,26,27).
The goals in the surgical treatment of Type II and III Hangman's fractures are reduction, stabilization, and maintenance of alignment. Although method of surgical stabilization is selected according to severity of C2 fracture and degree of displacement, specific anatomical aspect of atlantoaxial complex should be also considered C2 vertebra is designed to provide a bearing surface on which the atlas may rotate and pars interarticularis is most stressed by translational movement between adjacent segments in cervical spine7,8). Surgical stabilization has been described in both anterior and posterior approaches. Among the different posterior approaches, direct repair of the pars fracture with a screw across the fracture line has the advantage of preserving motion of the axis3,5,17). However, direct pars repair does not address instability at the disc. The main advantage of this technique is not having to sacrifice any normal motion of the C2 segment and fixating only the fractured bones of C2. However, it can be used only in cases with minimal or no C2-C3 disc injury. The application of posterior C2 and C3 fixation to a highly unstable hangman's fracture results in the aggravation of the forward displacement of C2 due to the intraoperative prone position, particularly with the extremely unstable state of C25,11,17-18,27). This phenomenon can cause iatrogenic injury and may lead to extremely negative consequences. Posterior C1-C3 wiring techniques have also been described, these techniques require postoperative halothoracic immobilization4). Anterior C2-C3 interbody fusion was currently attempted first, followed by the procedure involving direct one-stage posterior C2 and C3 pedicle screw fixation in the fracture at the isthmus position18). Two separate incision and fusion surgery is needed, although it seems to provide adequate spinal immobilization.
Polyaxial screw and rod fixation system has been developed and is widely used as a standard instrument. Posterior C1-C3 lateral mass screws and rods fixation has been performed with satisfactory fusion rate6,13,14). Recent studies have also reported that the biomechanical comparison of stabilization techniques on Hangman's fracture and posterior C2-C3 screw and rod construction was found to be more effective on the stabilization of Hangman's fracture than anterior cervical plating and C2 pars screwing7). Pedicle screw fixation is a biomechanically stronger repair method and requires only a posterior approach1,19). In addition, pedicle screw instrumentation through a single stage posterior approach offered better biomechanical stability in 3 column spinal injury. However, pedicle screw placement is technically demanding because of large individual variations in the pedicle dimensions and course of the vertebral artery.
Both posterior C1-C3 and C2-C3 fixation can offer high fusion rate. However, posterior C1-C3 fixation immobilized intact C1-C2 segment and leaded serious limitation of neck motion and axial pain. This showed the differences in clinical outcomes between these two techniques. In C2-C3 group, the average VAS score for neck pain and NDI scores were much less than those in C1-C3 group right after the surgery and these differences continued until final follow-up. The differences of VAS score and NDI score between C2-C3 and C1-C3 groups at each follow-up period were statistically significant (p<0.001) by paired T-test. Even though other clinical situations, such as accompanying injury to soft tissue or other levels and severity of dislocation, these differences of VAS score and NDI score at final follow-up visit with the full recovery from the initial injury can show clinical significance. C2-C3 group showed better clinical and biomechanical results than C1-C3 group in terms of axial pain and disability of neck.
There was one case of screw loosening in C2-C3 group which needed revision surgery for screw repositioning. Although posterior C2-C3 fixation for unstable Hangman's fracture offers biomechanical stability without additional treatment, there are some prerequisite conditions for achievement of good clinical and radiological results. Complete reduction and close adhesion of fracture gap should be achieved before the insertion of C2 screw. And, we have to press down the screw during insertion of C2 pedicular screw not to make fracture gap wide. Even if complete reduction is not achieved before the insertion of pedicle screws, bicortical purchase of C2 pedicular screw, or posterior C1-C3 fixation, is recommended.
Even though posterior C2-C3 fixation for unstable Hangman's fracture may have better clinical outcomes compared with those of posterior C1-C3 fixation, clinical application should be carefully considered regarding severity of injury of C2 vertebra and instability to adjacent vertebrae.
CONCLUSION
A higher degree of immobilization and strong fixation may lead higher fusion rate of hangman's fracture. Even though higher and satisfactory fusion rate can be achieved in both posterior C2-C3 fixation and C1-C3 fixation groups, their clinical outcomes can be different because of pain and neck disability. Posterior C2-C3 fixation is a segmental fixation in patient with Hangman's fracture and may be feasible surgical treatment in proper indication compared with posterior C1-C3 fixation.