|
 |
- Search
Abstract
Radiculopathy triggered by degenerative spinal disease is the most common cause of spinal surgery, and the number of affected elderly patients is increasing. Radiating pain that is extraspinal in origin may distract from the surgical decision on how to treat a neurological presentation in the lower extremities. A 54-year-old man with sciatica visited our outpatient clinic. He had undergone laminectomy and discectomy to treat spinal stenosis at another hospital, but his pain remained. Finally, he was diagnosed with a plexopathy caused by late recurrence of colorectal cancer, which compressed the lumbar plexus in the presacral area. This case report illustrates the potential for misdiagnosis of extraspinal plexopathy and the value of obtaining an accurate history. Although the symptoms are similar, spinal surgeons should consider both spinal and extraspinal origins of sciatica.
Nerve root compression caused by degenerative disc disease around the spinal column is a common cause of radiating pain to the lower extremities9). Radiating pain of extraspinal origin can be easily overlooked and may be difficult to discriminate from radiculopathy caused by spinal disease and plexopathy in the pelvic area, distracting from the neurological diagnosis of a lower extremity problem. Alertness to both disease entities may prevent unnecessary or incorrect spinal surgery. We herein describe a patient who underwent spinal surgery to treat sciatica but was finally diagnosed with late recurrence of colorectal cancer in the presacral area.
A 54-year-old man with sciatica in the left buttock and posterior aspect of the left leg visited our outpatient clinic. He rated his pain at 7 of 10 possible points on a numerical scale. He had undergone laminectomy and discectomy after diagnosis of lumbar stenosis at another hospital when the symptoms had developed 8 months prior. However, the symptoms did not improve.
Preoperative lumbar magnetic resonance imaging (MRI) revealed mild disc protrusion at L4/5 (Fig. 1). Lumbar MRI 2 weeks postoperatively revealed a well-decompressed thecal sac (Fig. 2). The motor power of the lower extremities was intact on neurological examination, but disabling pain was aggravating the left fourth lumbar to first sacral dermatome. The pain was constant and was not relieved by postural change. Because the sciatica did not improve and was even becoming aggravated, he underwent three additional lumbar MRI examinations at different hospitals. All MRI findings were similar.
Although he had a history of colon cancer surgery 7 years prior, he did not report this history to the spinal surgeon or medical personnel because he had been told that the colon cancer had completely remitted 5 years after the colorectal surgery. No palpable mass was evident in the abdominal or pelvic areas.
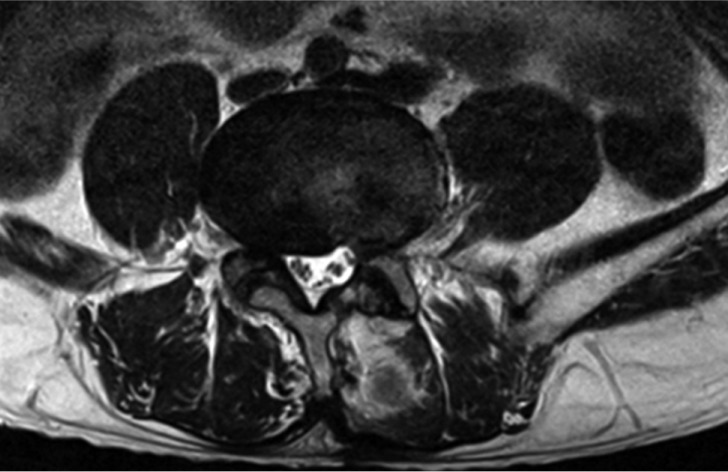
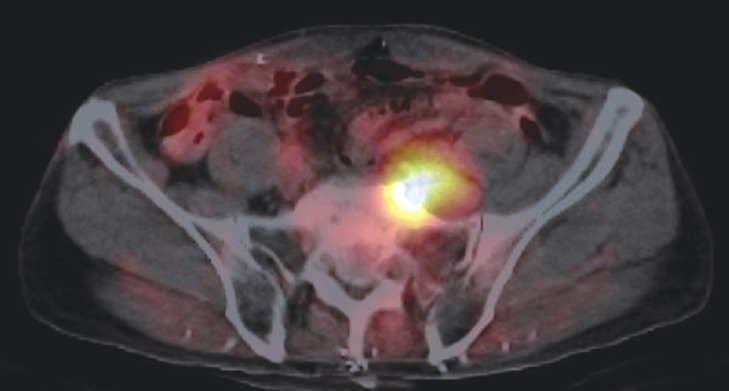
We performed enhanced pelvic MRI, which revealed a heterogeneous, well-enhanced mass compressing the lumbar plexus at the anterior aspect of the left sacrum. The lobulating mass was suspected to be a metastasis of colon cancer to the presacral lymph node (Fig. 3). An abdominal pelvic computed tomography scan also revealed a heterogeneously enhanced mass destroying the sacral bone of the left pelvic wall (Fig. 4). Colonoscopy revealed no evidence of cancer recurrence at the colonic anastomotic site; only benign polyps were apparent. 18F-Fluorodeoxyglucose positron emission tomography-computed tomography also revealed an enhanced mass (standardized uptake value, 2.1) with cortical invasion of the sacrum (Fig. 5). The carcinoembryonic antigen level was elevated at 16.44 ng/mL (reference range, 0.0-4.7 ng/mL).
Colorectal surgeon performed surgery via a midline transperitoneal approach. The recurrent mass was severely adhered to the lumbar plexus in the presacral area (Fig. 6). The mass was removed and adhesiolysis was performed around the plexuses. A metastatic lesion in the deep pelvic area could not be removed completely because of massive bleeding from the deep pelvic venous plexus. The sciatica improved markedly after surgery. Pathological examination revealed a metastatic adenocarcinoma. Immunostaining for CK20 and CDX2 was positive, and the K-ras mutation (codon 12 p.G12D) was present. The patient underwent chemotherapy and adjuvant radiation therapy under a final diagnosis of recurrent colon cancer at the presacral lymph node.
The lumbar plexus comprises T12-L5 and the sacral plexus of the S1-5 nerve roots. Radicular pain in the leg can be caused by various pelvic plexopathies. Demyelinating disease, a neoplasm, an inflammatory lesion, post-partum status, diabetes, osteoarthritis, and radiotherapy are reported extraspinal causes of plexopathy2,4,5,11,12).
It is difficult to clinically discriminate between radiculopathy caused by spinal disease and plexopathy from the pelvic area. Very similar cases were reported in 195510). Nineteen patients had malignant bone tumors in the lumbar spine or pelvis, and 10 had symptoms of degenerative disc disease. Laminectomy was performed unnecessarily in nine of these patients. The same errors continue to be made despite the fact that today's diagnostic tools are much more advanced. Indeed, several case reports on unnecessary spinal surgery seeking to treat radiating pain, which was ultimately identified as being of extraspinal origin, have been published recently7,13).
Radiculopathy caused by spinal disease may be intermittent or constant, and may worsen with increased intra-abdominal pressure (as when coughing). The pain may be relieved in the supine position, which decreases pressure on the herniated disc, and is aggravated by sitting, bending, or prolonged standing. Stretching the nerve reproduces pain in the sciatic distribution; this is the so-called "Lasegue sign"6). Numbness and muscular weakness may also develop in one leg.
Extraspinal radiculopathy can cause lower extremity pain, sensory disturbance, and weakness. Bickels et al.3) reported that a particular pain pattern was the single most common finding in patients with extraspinal tumors. In patients with neoplastic plexopathies, pain onset is usually insidious, prominent in one leg, and often the initial symptom of disease1). An early diagnosis is possible if the pain pattern is insidious in onset, constant, progressive, and unresponsive to changes in position. However, patients with spinal diseases complain of similar symptoms.
If a patient has underestimated lumbosacral plexopathy combined with asymptomatic radiological stenosis, the surgeon may make a wrong decision; lumbar spinal surgery is unnecessary.
It is difficult to accurately distinguish spinal from retroperitoneal or pelvic diseases using radiology alone; the imaging characteristics are nonspecific. Such clinical scenarios, coupled with imaging, should be contemplated by both the spinal surgeon and radiologist, who need to recognize that a non-spinal lesion is possible11).
In the present case, the principal reason for failure of an initial diagnosis of metastatic lymphadenopathy was that the cancer was of low signal intensity on T2-weighted images, inviting confusion with a part of the paravertebral muscle, particularly on sagittal images. Another reason is that the initial MRI protocol did not include contrast-enhanced MRI, which highlights a lesion. It is difficult to trace the lumbosacral plexus via two-dimensional MRI (the orientation of which is oblique). Some authors have attempted to trace the plexus using three-dimensional short-tau inversion recovery reconstructions in the coronal oblique plane through the plexus1).
Although we did not perform electrodiagnosis, this modality, coupled with nerve conduction studies and needle electromyography, can help localize and characterize the underlying cause of a neurological condition in the absence of any invasive procedure8). Such work distinguishes plexopathy from radiculopathy; both the amplitudes and conduction speeds differ. However, an electrophysiological study does not feature in routine evaluations prior to spinal surgery, which may be a serious error if a patient has symptoms that cannot be matched with radiological data.
Lumbosacral plexopathy is a severe clinical syndrome that is very likely to be underdiagnosed because of confusion with lumbosacral disc disease. This case report emphasizes the importance of obtaining an accurate history and careful performance of a neurological examination to differentially diagnose lumbar plexopathy from degenerative lumbar disease. A spinal surgeon should always consider an extraspinal origin of sciatica arising from the pelvis, particularly in a patient with symptoms that are not explained by imaging.
References
1. Ailianou A, Fitsiori A, Syrogiannopoulou A, Toso S, Viallon M, Merlini L, et al. Review of the principal extra spinal pathologies causing sciatica and new MRI approaches. Br J Radiol 2012 85:672-681. PMID: 22374280.



2. Benny BV, Nagpal AS, Singh P, Smuck M. Vascular causes of radiculopathy: a literature review. Spine J 2011 11:73-85. PMID: 21168101.


3. Bickels J, Kahanovitz N, Rubert CK, Henshaw RM, Moss DP, Meller I, et al. Extraspinal bone and soft-tissue tumors as a cause of sciatica. Clinical diagnosis and recommendations: analysis of 32 cases. Spine (Phila Pa 1976) 1999 24:1611-1616. PMID: 10457583.


4. Cho YJ, Kim SB, Chin DK, Seo EK, Kim SJ. Spinal Cord Tumors which were Misdiagnosed as Degenerative Spine Disease. Korean J Spine 2004 1:94-99.
5. Choi I, Im SB, Kim BT, Shin WH. Radiculopathy Caused by Internal Iliac Artery Pseudoaneurysm Managed with Endovascular Embolization. J Korean Neurosurg Soc 2007 42:484-486. PMID: 19096595.



6. Jaeckle KA, Young DF, Foley KM. The natural history of lumbosacral plexopathy in cancer. Neurology 1985 35:8-15. PMID: 2981417.


7. Jung DY, Cho KT, Lee SC. Atypical Guillain-Barr? Syndrome Misdiagnosed as Lumbar Spinal Stenosis. J Korean Neurosurg Soc 2013 53:245-248. PMID: 23826482.



8. Laughlin RS, Dyck PJ. Electrodiagnostic Testing in Lumbosacral Plexopathies. Phys Med Rehabil Clin N Am 2013 24:93-105. PMID: 23177033.


9. Melikoglu MA, Kocabas H, Sezer I, Akdag A, Gilgil E, Butun B. Internal iliac artery pseudoaneurysm: an unusual cause of sciatica and lumbosacral plexopathy. Am J Phys Med Rehabil 2008 87:681-683. PMID: 18388559.


10. Odell RT, Key J. Lumbar disk syndrome caused by malignant tumors of bone. J Am Med Assoc 1955 157:213-216. PMID: 13211338.


11. Planner AC, Donaghy M, Moore NR. Causes of lumbosacral plexopathy. Clin Radiol 2006 61:987-995. PMID: 17097418.


13. van Zyl AA. Misdiagnosis of hip pain could lead to unnecessary spinal surgery. SA Orthop J 2010 9:54-57.
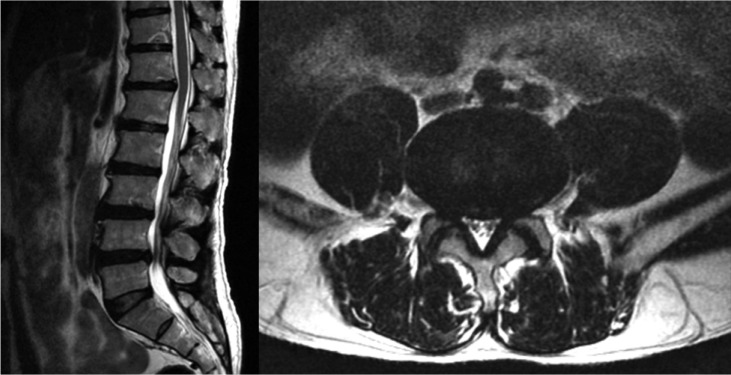
Fig.┬Ā3
Pelvic magnetic resonance image shows a well-enhanced heterogeneous mass (arrow) compressing the lumbar plexus.
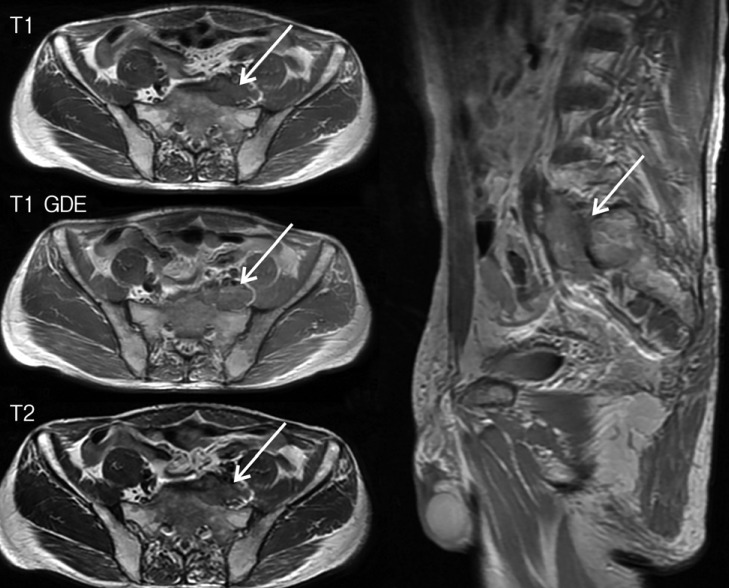
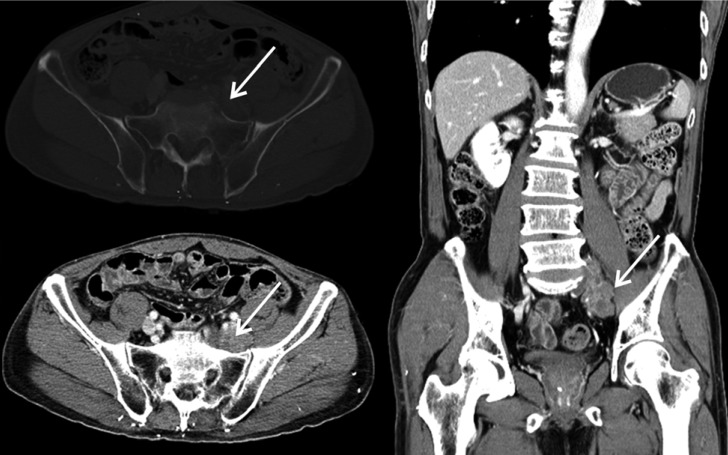
Fig.┬Ā4
Computed tomography scan shows a heterogeneously enhanced mass (arrow) destroying the sacral bone of the left pelvic wall.