INTRODUCTION
Calcifying psuedoneoplasm(CPN) involving the neural axis is very rare, with spinal involvement being even less frequent. About 20 cases of spinal CPN have been reported since the first description in 197816). The symptoms of spinal CPN vary from asymptomatic lesion to isolated pain, radiculopathy, or myelopathy. Lesions display, varied findings on imaging that can lead to erroneous malignant and inflammatory differential diagnoses. The pathogenesis of this non-neoplastic lesion is not obvious. Most cases are treated by surgical resection with good outcomes.
We present three cases of epidural CPN and review imaging and pathologic characteristics, surgical management, and outcomes. We also discuss the pathogenesis of epidural CPN.
CASE REPORT
Case 1
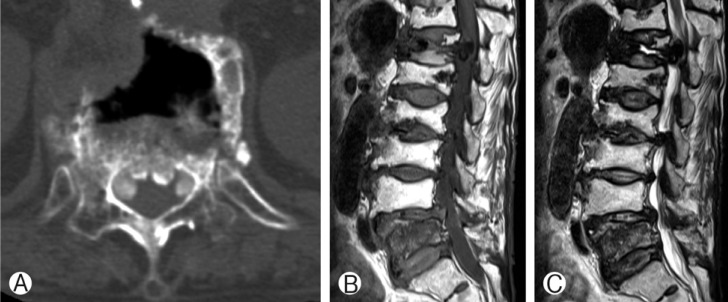
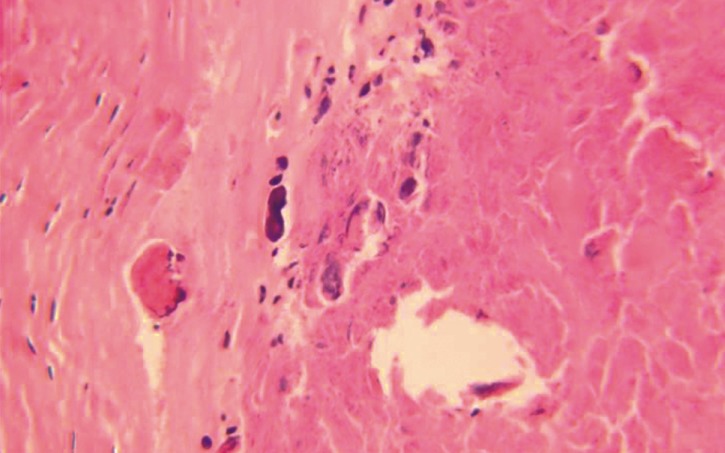
A 77-year-old woman presented with more than a two-year history of low back pain and pain in both legs, especially the left leg. Pain had become more aggravated following a minor trauma 20 days previously. She had a history for operation of vertebroplasty at the L1 body due to osteoporotic compression fracture 8 years ago. Computed tomography (CT) scans of the thoracolumbar spine showed three nodular high density lesions or structures in both anterolateral epidural space at the T12 body (Fig. 1A). Magnetic resonance imaging (MRI) showed three nodular dark T1 and T2 signal intensity lesions in the anterolateral epidural space at T12 body with thecal sac compression (Fig. 1B, C). After laminectomy of T12, gross total resections of masses were done. The masses were firm and adherent to the dura mater. Histologically, epitheloid cells in a granuloma-like pattern, fibrocellular stroma with spindled fibroblastic cells, and calcified materials were found. These pathology findings confirmed a CPN(Fig. 2). Postoperatively, back pain and radicular pain were resolved. Follow-up CT scan 5 months after surgical resection confirmed no recurrence; at that time, symptoms continued to be almost completely relieved.
Case 2
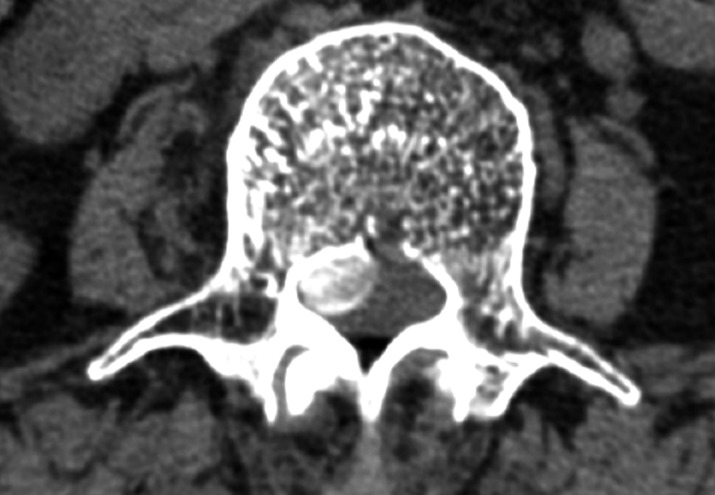
A 67-year-old female patient presented with a two-month history of radiculopathy on the L3 dermatome of the right leg. She had undergone posterior cement-augmented pedicle screw fixation from T12 to L2 for burst fracture of L1 before 4 years. CT scans of the thoracolumbar spine showed a prominent central to right side calcified epidural mass measuring 10.4├Ś7.5mm, with a distinct increased density at the body of L2 and L3 (Fig. 3). Laminectomy of L2 and L3 and total removal of the epidural mass were done. After mass resection, extension of previous posterior fixation to L3 level was done. Pathology finding indicated CPN. Symptoms were resolved after surgical resection.
Case 3
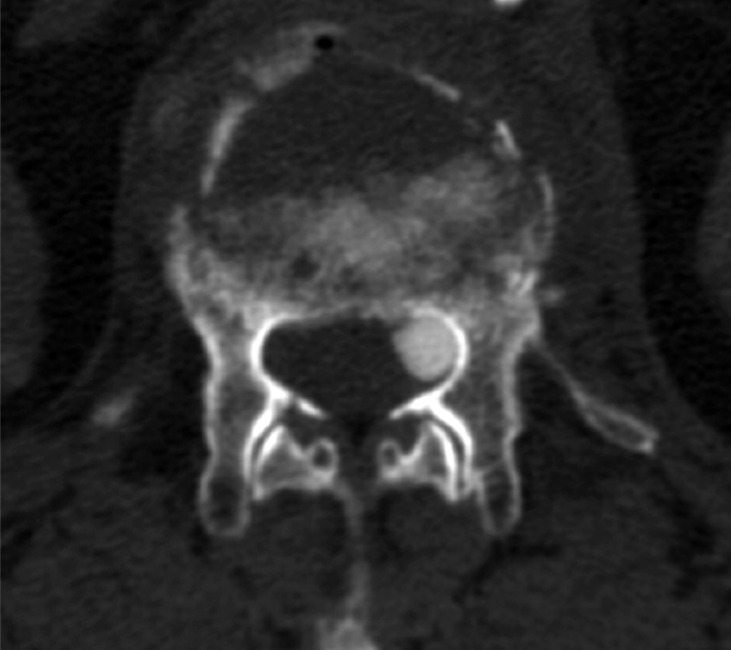
A 78-year-old woman presented with a two-month history of low back pain after a slip. She had already been diagnosed as an osteoporotic compression fracture of L1 and had been treated conservatively. The pain had become worse over time. CT scan of the lumbar spine revealed a lobulated, calcified mass measuring 7├Ś8.5 mm, with a well-defined margin along the left anterolateral side of the spinal canal at the L1 body level (Fig. 4). Left hemilaminectomy of L1 and epidural mass excision was done. Post-operatively, pain was resolved.
DISCUSSION
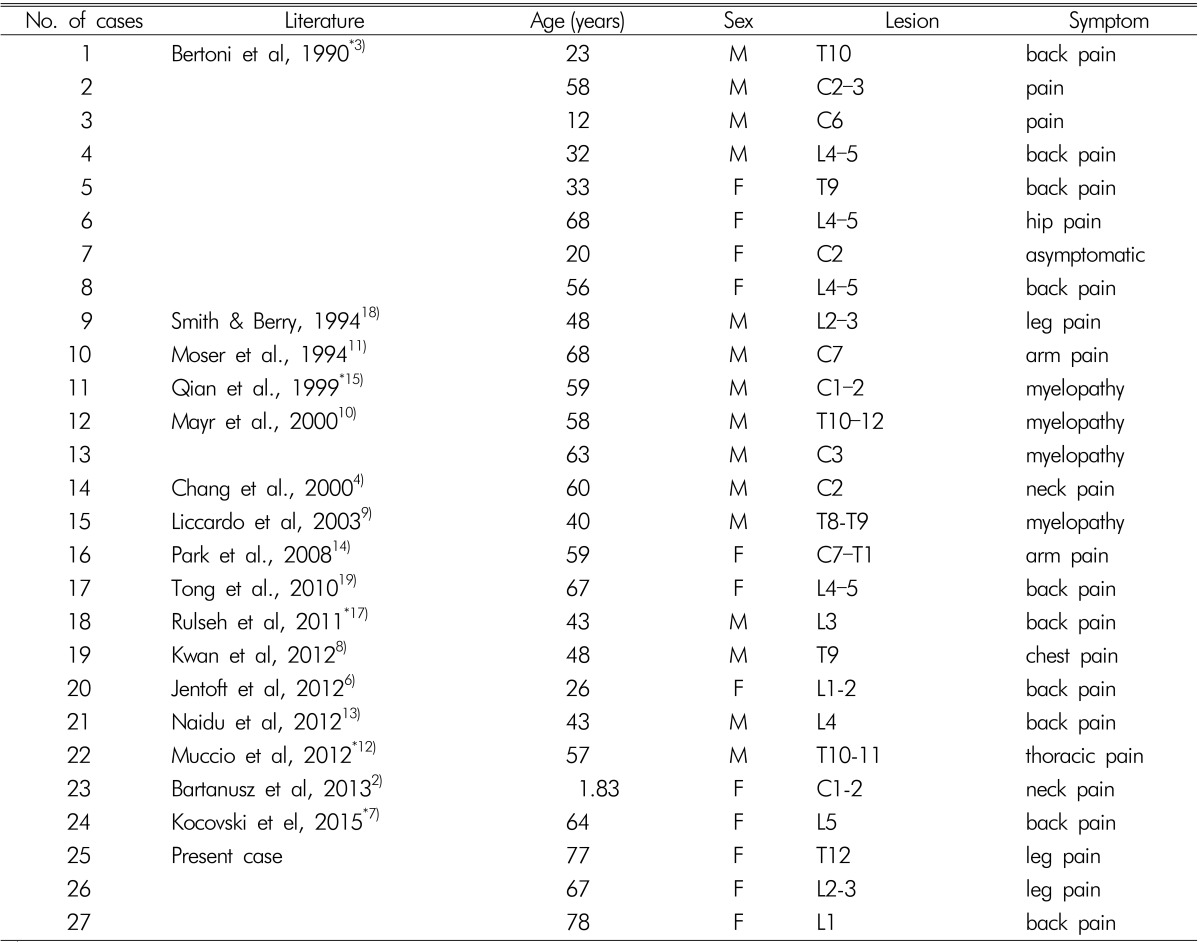
CPN or fibro-osseous lesions of the spine have been documented and reported in the literature in 27 cases, including these present three cases (Table 1)2,3,4,5,7,8,9,10,11,12,13,14,15,17,18,19). The age of the affected individuals has varied widely, from a 22-month-old girl to a 78-year-old woman. Half of cases occurred in middleage adults, with male patients predominating. No CPN has been described in the spinal intramedullary area.
Nine (33%) of the 27 cases were cervical lesions and six (22%) were located in the thoracic level. Lesions occurred in the lumbar spine in 12 (44%) patients, with symptoms varying from axial back pain to radiculopathy.
Pathologic findings have revealed five histological features1): (1) chondromyxoid matrix in a nodular pattern, (2) palisading spindle to epithelioid cells, (3) fibrous stroma, (4) calcification, osseous metaplasia, or scattered psammoma bodies, and (5) foreign body type reaction with giant cell. These components vary markedly from patient to patient; the present three cases displayed some of these features.
The most common symptom of CPN is isolated pain. Radiculopathy due to compression of the nerve root is also common. For cervical lesions, myelopathy is the more frequent symptom. However, an asymptomatic incidental mass has been reported3).
The radiologic manifestations of spinal CPN vary, although many cases feature hypointensity signal on T1- and T2-weighted MRI. Contrast enhancement on T1-weighted images has revealed no enhancement in some cases, with other cases displaying peripheral rim enhancement. Heterogeneous enhancement and internal linear enhancement have also been reported. Dense calcification is a characteristic of CT scans. Differential diagnosis for a calcified mass on the spinal cord include calcified disc material20) or synovial cyst, psammomatous meningioma, epidural abscess, chronic hematoma, and infectious mass (e.g. tuberculoma).
The pathogenesis of CPN is still unclear. Garen et al.5) postulated that the process may be an erroneous membranous bone formation with osseous metaplasia. Bertoni et al.3) presumed that the cause of mass formation was unexpected expression of tumoural calcification in periarticular soft tissue. CPN is regarded as a being associated with degenerative joint disease. However, this view cannot explain cases of adolescents in whom joint degeneration was absent. Some cases occurred after trauma or surgery1,17), bolstering the view that pathogenesis is associated with a reactive and metaplastic response to injury. In our three cases, CPN also presented after compression fracture trauma or following surgery. So, there may indeed be a relationship between CPN and tissue injury. The presence of granulomatous inflammation surrounding nodules of calcification substantiates this theory.
Most cases of spinal CPN have been treated with surgical management. Surgical total or subtotal resection of CPN has a good prognosis. Almost all patients experienced improvement of symptoms and very low rates of recurrence. Kwan et al.8) reported thoracic CPN in a 48-year-old man, which resolved symptomatically and on imaging after treatment with oral indomethacin 25mg 3 times daily. The lesion was seen to decrease in size on CT and MRI after 8 weeks of treatment and to completely resolve by 16 weeks of treatment.
CONCLUSION
Calcifying pseudoneoplasm of the spine is a very rare and benign entity. It causes variable nonspecific symptoms from pain to myelopathy. A dense calcified mass on extradural space post-trauma or following surgery should prompt consideration of CPN. Surgical excision of the lesion provides excellent prognosis, with the chance of recurrence being low.