INTRODUCTION
The term spondylolisthesis describes a pathologic slippage of one vertebra against another. It is one of the spinal diseases requiring fusion surgery. Posterior fusion techniques including posterolateral fusion, posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF) and circumferential fusion have been performed to treat spondylolisthesis7). Bone fusion and screw fixation have been associated with a high fusion rate, especially in the treatment of low grade spondylolisthesis in which the segment of the spinal column to be fused is under a more compressive load. However, the high shear stress at the lumbar or lumbosacral junction in moderate to high grade spondylolisthesis alters this bio-mechanical advantage. Moreover, forceful slip reduction was reported to have an high rate of neural injury caused by distraction of nerve roots2,13,14,15). The correction degree of sagittal translation is still controversial focus on method and degree for symptomatic spondylolisthesis. So far, it has not been clear whether potential benefit or lack thereof is due to the translational or the angular reduction, and it is difficult to form a clear guideline for spondylolisthesis. Moreover, the use of minimally invasive mini-open PLIF using the percutaneous screw fixation system for moderate to severe spondylolisthesis has not been previously described. The current study describes the surgical technique and feasibility of the mini-open PLIF with percutaneous screw fixation for moderate to high grade spondylolisthesis to achieve spontaneous slip reduction minimizing neural injury.
MATERIALS AND METHODS
Between January 2007 and December 2010, 40 consecutive patients who underwent mini-open PLIF for Grade II spondylolisthesis or more were included in this study. The inclusion criteria were: (1) no previous surgery at the level of spondylolisthesis, (2) followed up for at least 12 months, and (3) no severe osteoporosis (the lowest T-score on dual energy X-ray absorptiometry bone mineral density >-3.0). The patients' age ranged between 29 and 68 years (average 59.4) and mean follow-up period was 24.1±13.5 months. The preoperative diagnosis was 22 cases of degenerative type and 18 cases of isthmic type, comprising 32 cases with Meyerding Grade II, 5 cases with Meyerding Grade III and three cases with Meyerding Grade IV. Spondylolisthesis was present at the L3-4 level in three patients, at the L4-5 level in 24 patients and at the L5-S1 level in 13 patients.
1. Surgical Technique
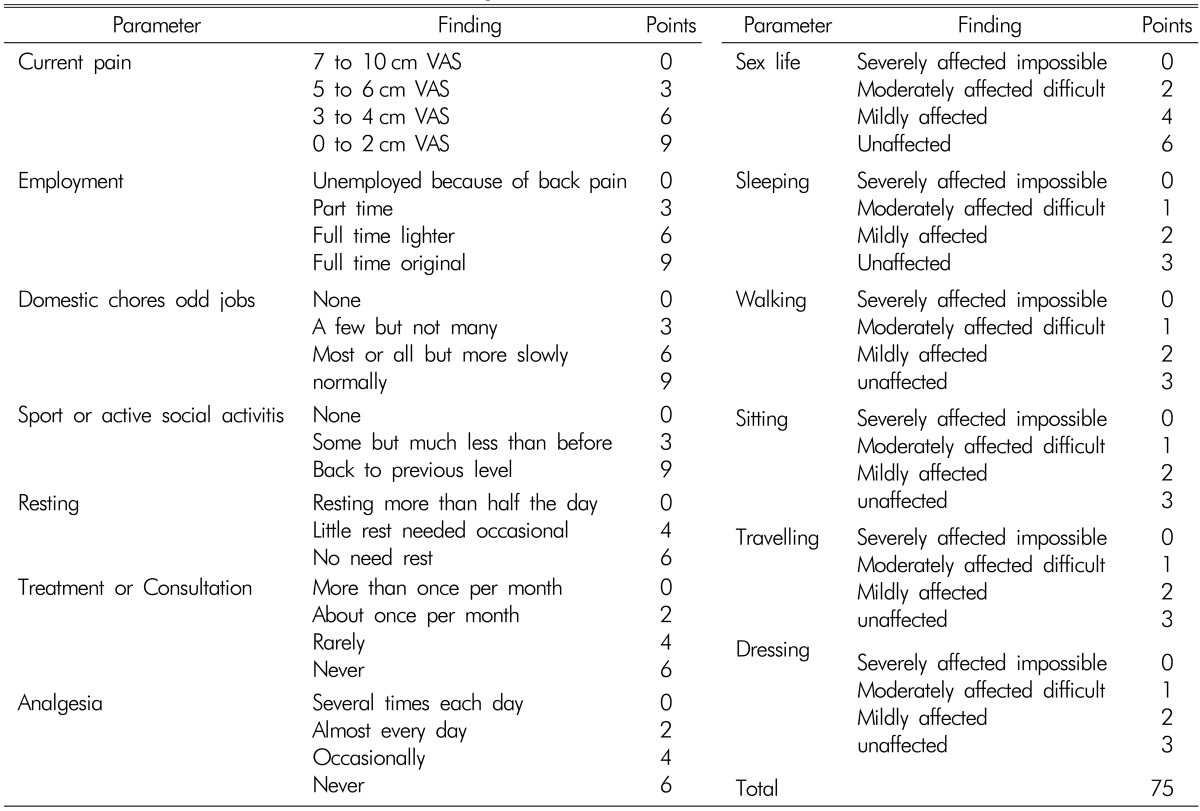
All patients underwent mini-open PLIF in the prone position. Following a midline skin incision, an expandable tubular retractor of appropriate length (X-tube, Medtronic Sofamor Danek, Memphis TN., USA) was inserted at each level. Decompressive surgery consisted of transfacet laminectomy and foraminotomy bilaterally. Complete removal of the scar tissue around the pars interarticularis led to the sufficient liberation of the nerve root under the slipped pedicle, achieving posterior release as well. The disc inferior to the slipped vertebrae was thoroughly resected, lateral to both pedicles, in which course, the disc space was gradually distracted and released with sequential disc shavers, removing of the anterior annulus as much as possible that was even in conjunction with anterior longitudinal ligament (ALL) to accomplish exhaustive anterior release, followed by insertion of cages bilaterally. During the maneuver, due to circumferential release, it could be found that the slipped vertebrae tended to obtain partial spontaneous reduction. Secondly, percutaneous pedicle screws with a vertical axis and detachable extender (Apollon system®, Solco medical, South Korea) were inserted without additional skin incision. After dissection of the subdermal plane, the percutaneous screws were inserted following retraction of the skin. Furthermore, with the compressing the screws into each other to create a lumbar lordosis, additional reduction could be achieved without any application of compulsive force. Imaging and clinical findings including involved level, slip percentage, lumbar lordotic angle, focal segmental angle, clinical outcomes, and complications were analyzed. Clinical outcomes were measured using a self assessment 10-point visual analog scale (VAS) and low back outcome score (LBOS) normalized to 75 (Table 1).
2. Radiological Measurement
The slippage was measured from standing lateral radiographs and calculated as the quotient of sagittal displacement expressed in percent. Lumbar lordotic angle was defined by Cobb's method, using the intersection of lines at the level of the superior plateau of L1 and the inferior plateau of L5. Focal segmental angle was defined as the focal angle of superior line of spondylolisthetic level and inferior line of adjacent lower level.
RESULTS
All patients were followed for at least 12 months and the mean follow-up period was 24.1 months. At a minimum of 12 months follow-up, all cases appeared to have solid fusions as judged by the presence of a trabecular bony bridge or less than 5° on dynamic flexion and extension views.
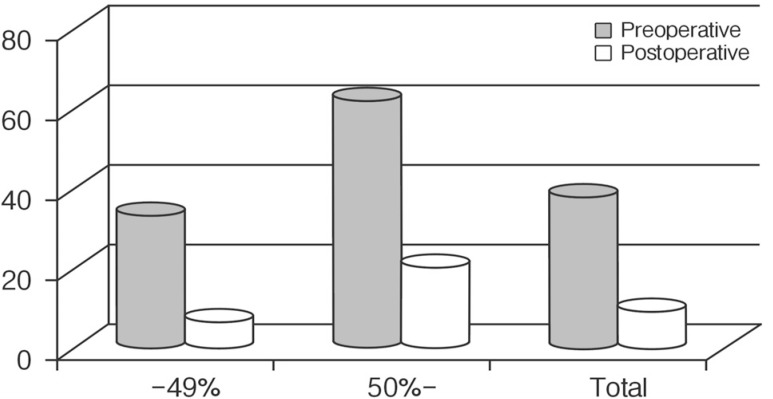
1. Degree of Slippage Reduction
Preoperative slippage averaged 38.0±12.6%. At the latest follow-up, mean slippage improved significantly to 9.3±7.8% (p<0.001) (Fig. 1).
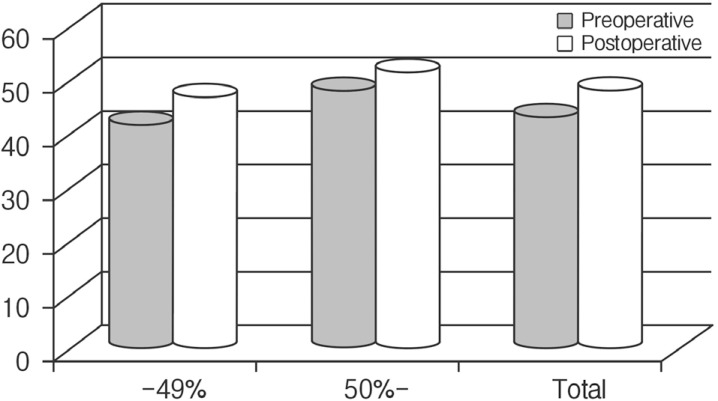
2. Degree of Lumbar Lordotic Angle
Lumbar lordosis, measured from the upper endplate of L1 to the inferior endplate of L5, was 43.0±13.8° before surgery. In spite of no statistical significance, mean lordosis was changed to 48.2±10.3° at last follow-up (p>0.05) (Fig. 2).
3. Degree of Focal Segmental Angle
Degree of focal segmental angle, measured from the upper endplate of slipped vertebra to lower endplate of adjacent vertebra, was 10.1±8.5° before surgery. At the latest follow-up, the focal segmental angle was 15.9±6.0°, which improved significantly (p<0.01) (Fig. 3).
4. Clinical Outcome
There was no case required a blood transfusion. The mean LBOS prior to surgery was 32.5, which improved to 53.1 at the last follow-up (p=0.037). From a preoperative average of 7.5, the VAS score was decreased significantly to 3.0 at 7 days postoperatively and 2.9 at the final follow-up (p=0.015).
5. Complications
There was no case to be converted into conventional open surgery due to technical difficulty. Complications included one case of medial penetration of pedicle border, which needed screw re-insertion and two cases with a superficial wound infection. However, there was no pseudoarthrosis. All patients had a solid bony fusion at the last follow-up, without any dislocation compared to the immediate postoperative radiographs. Two patients with Grade III spondylolisthesis showed a signs of a transient root lesion after surgery (1 case of transient and mild motor weakness and 1 case of radiating pain and sensory change), which resolved completely. However, there were no permanent neurological sequelae as a result of miniopen PLIF (Fig. 4 and 5).
DISCUSSION
Spondylolisthesis is a relatively common disease with an incidence approximately 5% of the population requiring fusion surgery4). Low-grade spondylolisthesis may be managed by conservative treatment in some cases, but in moderate to high grade spondylolisthesis, nonoperative methods are not able to prevent the progressive back and radiating pain, increasing slip and deformity or cauda equina symptoms. Decompression was introduced as the treatment for spondylolisthesis that induces radiating pain by Gill in 1955, and subsequently various surgical techniques have been performed1). Symptomatic spondylolisthesis usually require surgical intervention, the goals of which include the stabilization of the motion segment, decompression of neural elements, reconstitution of disc space height, and restoration of sagittal plane translational and rotational alignment. Among them, PLIF is a widely performed procedure and it has been associated with the improvement of the fusion rate while restoring disc height and maintaining vertebral alignment for spondylolisthesis. Moreover, recently, mini-open PLIF using percutaneous screw fixation system can provide many potential benefits compared to conventional PLIF5). For the treatment of symptomatic spondylolisthesis, however, the role of compulsory translational reduction and instrumentation is controversial. Some proponents state that the reduction itself will improve the rate of fusion and improve spinopelvic balance3). The theoretical advantages of slip reduction include improved spine biomechanics, better nerve root decompression, and chance to obtain fusion because it provides an increased surface area of the fusion bed and the fusion is no longer under the influence of tension and anterior shear forces. Another advantage of slip reduction is the correction of the sagittal deformity to improve posture. Re-aligning the spine and achieving sagittal balance are important in the long run by preventing premature adjacent level disc degeneration12). On the contrary, a forceful and mandatory instrumented slip reduction can certainly lead to reduction even by 100%, which will increase the risk of permanent complications. The major disadvantage of complete slip reduction is the increased risk of neural injury caused by excessive distraction of nerve roots11). The various hypothetical cause of neurologic injury include direct pressure on the nerve root during reduction, impingement of the nerve roots on the iliolumbar ligaments, extradural tension on the nerve roots, and disc material extruded into the canal6,8). Moreover, for the treatment of high-grade spondylolisthesis, the risk of neural injury caused by forceful reduction and pseudarthrosis is much higher9,10). To overcome these disadvantages, spontaneous partial reduction techniques have evolved. Pan et al.12) reported that circumferential release, including scar resection for posterior release complete disc removal and distraction with rupture of annulus conjunct with anterior longitudinal ligament for anterior release in the treatment of low-grade isthmic spondylolisthesis. Significant slip reduction for the group was achieved and the fusion rate approached 100% with no definite neurological complications. They insisted that spondylolisthesis has a certain trend toward spontaneous reduction intraoperatively, including the reduction of translational and rotational deformity, which can provide good outcomes. The technique described here also meets these requirements. Reduction of the slippage was achieved by a combination of two principles. First, circumferential release was applied. Resection of the scar around the pars interarticularis would lead to liberation of the nerve roots, which could help to achieve posterior release. The disc was totally resected with removing the anterior annulus as much as possible even in conjunction with ALL, and the disc space was gradually distracted with sequential disc shavers to fully restore the disc space height, accomplishing anterior release. Second, with the insertion of cages to maintain the height, the following influence of percutaneous pedicle fixation on the spinal alignment by compressive force, additional reduction could be achieved without any application of powerful posterior translational force. As a result, no forceful tension acts on the pedicle screw system, obviously decreasing the anterior shear forces. All the surgical procedures in this study were performed by a single surgeon to eliminate the variable effects of different surgeon on surgical outcome. However, larger-scale, multicenter studies involving more surgeons are necessary to validate our results.