Cervical Sagittal Alignment Parameters of Patients Admitted to Neurosurgery and Emergency Clinics in a State Hospital at Eastern Part of Turkey
Article information
Abstract
Objective
Cervical spine encompasses a bridge role between the head and the lower parts of the spine and therefore has unique properties. Our aim in this study was to evaluate the cervical sagittal alignment parameters in pediatric and adult non-surgical patients and to find any differences in respect of age, sex and admission type.
Methods
All patients who were admitted to emergency and neurosurgery clinics of Diyarbakir Bismil State Hospital due to cervical spine problems (trauma, radiculopathy, paraspinal pain) in 2014 were enrolled retrospectively into the study. Cervical anterior-posterior and lateral X-rays were obtained. Our exclusion criteria were cervical coronal deformity, multitrauma, Glasgow Coma Scale <15, traumatic disruption of the cervical spine, history of malignancy, spinal infection, metabolic or rheumatologic diseases.
Results
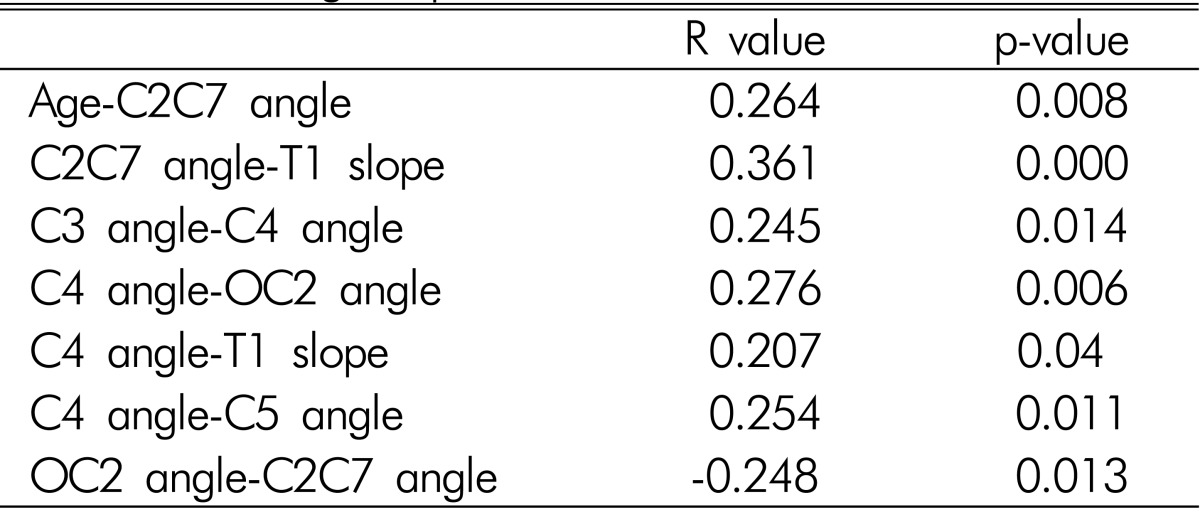
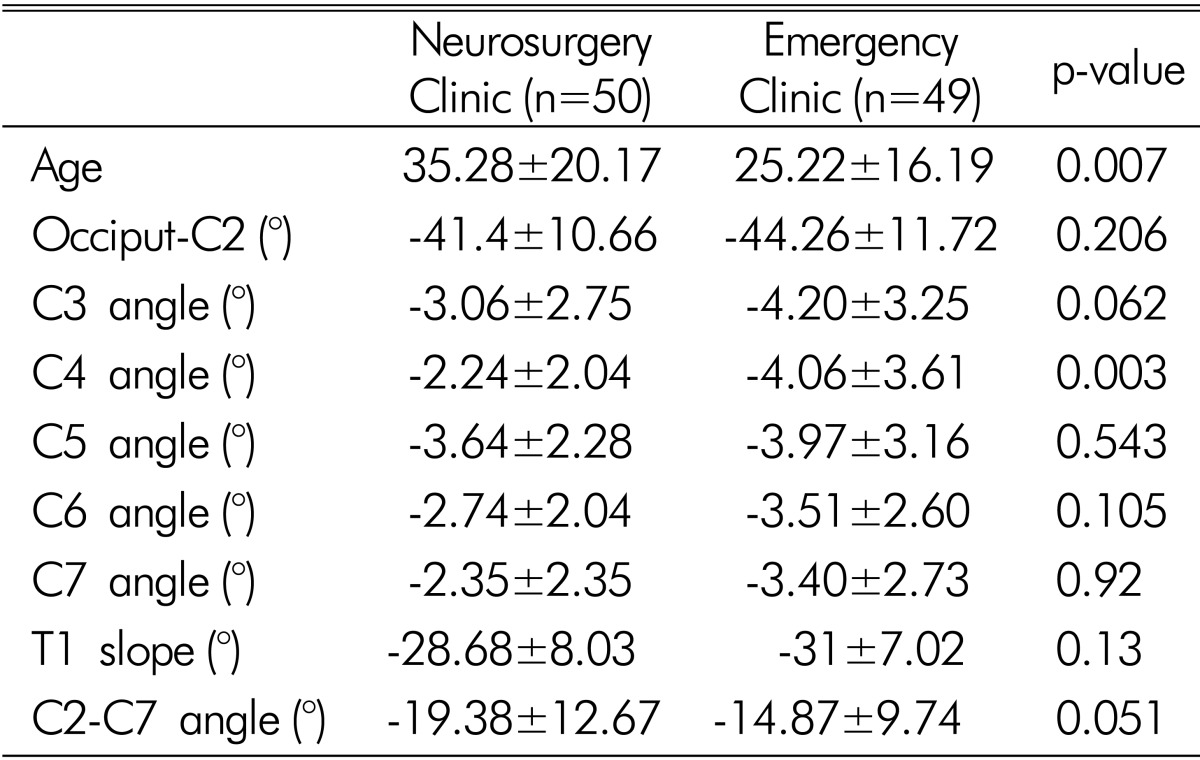
There were 44 female and 55 male patients (n=99) in the study. Thirty-five (35.35%) of the patients were younger than 18 years of age. Mean cervical spinal alignment parameters were as follows: -42.81±11.23° (OC2), -17.15±11.48° (C2-C7), -29.82±7.60° (T1 slope), -3.62±3.05° (C3), -3.14±3.05 (C4), -3.80±2.74° (C5), -3.12±2.36° (C6), -3.43±2.53° (C7). Positive correlations were observed between age-C2C7 angle, C2C7 angle-T1 slope, C3 angle-C4 angle, C4 angle-OC2 angle, C4 angle-T1 slope, C4 angle-C5 angle. The one only negative correlation was between OC2 angle-C2C7 angle.
Conclusion
In this regional study, it has been observed that global cervical lordosis increases as age increases. C4 vertebra is in the middle of this evaluation as it has many correlations with other cervical segments, which should be kept in mind when making surgical plans for this delicate spine region.
INTRODUCTION
Spinal alignment has been the area of interest with a more comprehensive understanding of the underlying mechanisms. Dubousset described the spinal balance in the economic range of gravity named as 'cone of economy'4). Since then, sagittal and coronal parameters of thoracolumbar spine with pelvic parameters have been thoroughly studied3911). Cervical spine encompasses a bridge role between the head and the lower parts of the spine and therefore has unique properties; however cervical spinal alignment has not been studied as much as thoracolumbar spinal alignment. The studies are scarce even in the pediatric population1).
Our aim in this study was to evaluate the cervical sagittal alignment parameters in pediatric and adult non-surgical patients and to find any differences in respect or age, sex and admission type. We analyzed cervical lateral X-rays of 99 patients that admitted to a state hospital's emergency and neurosurgery clinics at eastern part of Turkey.
MATERIALS AND METHODS
All patients who were admitted to emergency and neurosurgery clinics of Diyarbakir Bismil State Hospital due to cervical spine problems (trauma, radiculopathy, paraspinal pain) in 2014 were enrolled retrospectively into the study. The study protocol was compatible with 1964 Declaration of Helsinki. Cervical anterior-posterior (A-P) and lateral X-rays (head to T2) were obtained while the patients stood in a relaxed position and hands were flexed over clavicles in adults and teenagers. The cervical x-ray of the younger ones was obtained with the assistance of one of the parents. The patients were asked to look straightforward during the procedure. Cervical A-P films were evaluated only for presence of coronal deformity (Cobb >10°). Our exclusion criteria were cervical coronal deformity, multitrauma, Glasgow Coma Scale <15, traumatic disruption of the cervical spine, history of malignancy, spinal infection, metabolic or rheumatologic diseases. Pediatric age limit was selected as 18 years. After exclusion criteria, 99 patients were found to be suitable for the study.
Lateral cervical spinal x-rays were assessed in respect of occipito-C2 angle (OC2) (between MacGregor line and inferior end-plate of C2 vertebral corpus), C2-C7 angle (between inferior end-plates of C2 and C7), T1 slope (between horizontal line and upper end-plate of T1 vertebral corpus), and segmental vertebral angles from C2 to C7(between upper and lower end-plates of each corresponding vertebral corpus) (Fig. 1). For accuracy of the data, all measurements were done by one of the authors (S.C.K.) on a software program(Surgimap, Nemaris Inc, New York, USA).

Cervical sagittal alignment parameters: (A) Occiputo-C2 angle, (B) C2-C7 angle (cervical lordosis), (C) C4 segmental angle, (D) T1 slope.
Dichotomous and continuous variables were evaluated with chi-square and student's t-test, respectively. Correlation study was done with Pearson's correlation. All statistical analyses were conducted with SPSS 22.0 (Statistical Package for the Social Sciences, IBM, New York, USA). An alpha value of <0.05 was accepted as significance of difference.
RESULTS
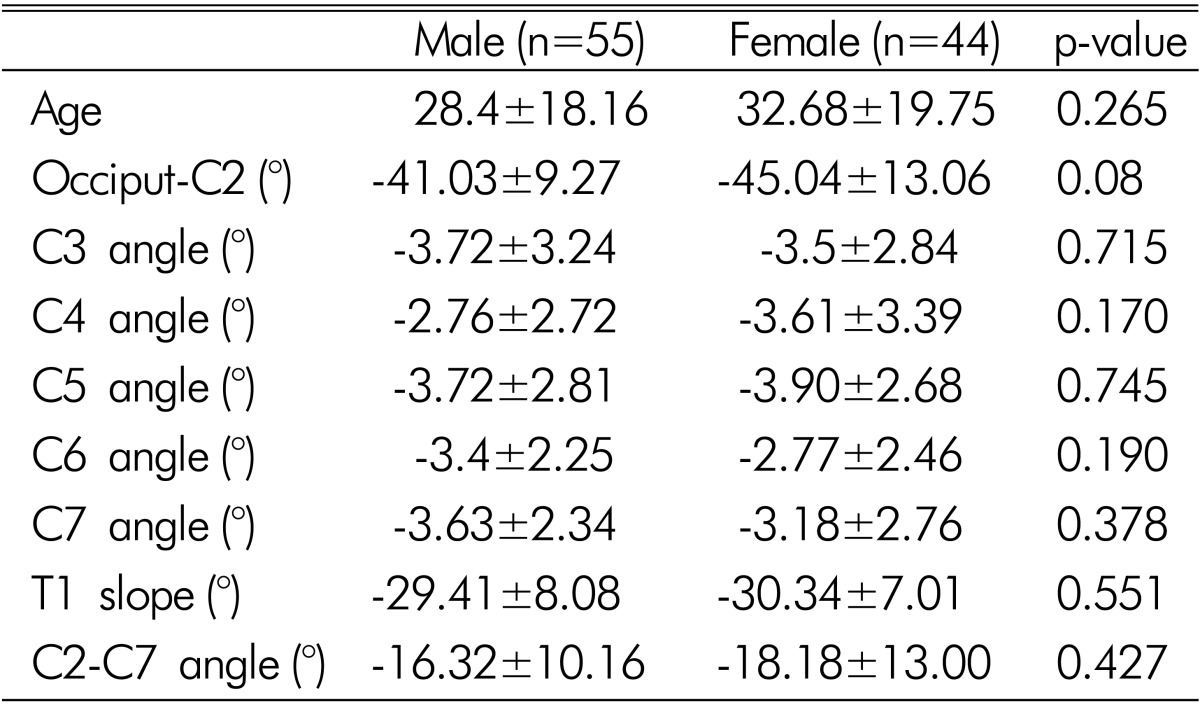
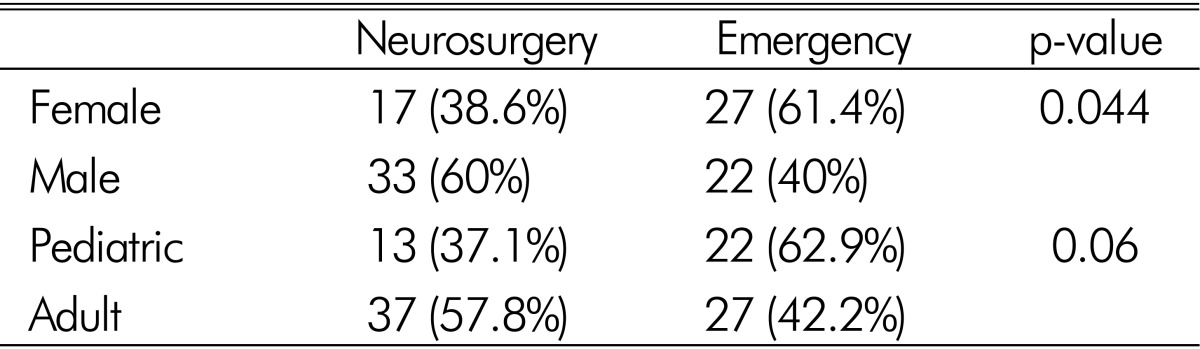
There were 44 female and 55 male patients in the study. Mean age of the cohort was 30.30±18.90 years. Thirty-five (35.35%) of the patients were younger than 18 years of age. Mean cervical sagittal alignment parameters were as follows: -42.81±11.23° (OC2), -17.15±11.48° (C2-C7), -29.82±7.60° (T1 slope), -3.62±3.05° (C3), -3.14±3.05 (C4), -3.80±2.74° (C5), -3.12±2.36° (C6), -3.43±2.53° (C7). Patients were compared according to clinical admission type, gender and their pediatric or adult status (Table 1,2,3). Statistical difference was present in age (p=0.007) and C4 angle (p=0.003) between patients admitted to emergency clinic and patients admitted to neurosurgery clinic. All other cervical sagittal alignment parameters were similar between the groups. More female patients were admitted to emergency department (61.4% vs. 40.0%, p=0.044) (Table 4).
Comparison of cervical sagittal alignment parameters according to patients' admission to neurosurgery or emergency clinic
Positive correlations were observed between age-C2C7 angle (R=0.264, p=0.008), C2C7 angle-T1 slope (R=0.361, p=0.000), C3 angle-C4 angle (R=0.245, p=0.014), C4 angle-OC2 angle (R=0.276, p=0.006), C4 angle-T1 slope (R=0.207, p=0.04), C4 angle-C5 angle (R=0.254, p=0.011). The one only negative correlation was between OC2 angle-C2C7 angle (R=-0.248, p=0.013) (Table 5).
DISCUSSION
Cervical spine is unique in respect of its wide range of motion capability and carrying the head over it. Cervical sagittal alignment is important not only for stability of motion in the 'cone of economy', but also preventing cervical spinal cord myelopathy2). It was demonstrated that spinal cord intramedullary pressure increased with increased amount of kyphosis514). The effect of changes is not limited to only morphological cord changes, but also influences quality of life of the patients significantly2). Morphometric radiographical studies dedicated to cervical sagittal alignment are rare in the literature.
There are several measurement methods that could be conducted to assess cervical sagittal alignment. Although Harrison posterior tangent method is superior over Cobb method in measuring cervical lordosis, it has been shown that good intra- and inter-rater reliability of Cobb method and its clinical use are easier than Harrison method81315). Cervical lordosis measurement with C1-C7 or C2-C7 has been performed and has been found that they have been overestimating and underestimating cervical lordosis, respectively2). We preferred C2-C7 sagittal Cobb angle to measure cervical lordosis of the patients. We also used occiput to C2 angle to involve all cervical spinal segments into consideration. In our final analysis, OC2 angle was found to be significantly negatively correlated with global cervical lordosis (C2-C7 angle). This makes sense as global cervical lordosis increases, OC2 angle decreases to keep the head in horizontal plane. Cervical lordosis angle of our cohort was 17.15±11.48° which is comparable to age-paired studies in the literature6). Increased age was found to be correlated with increased cervical lordosis, which is also comparable to current literature67). This could be explained in part by compensatory alignment changes in cervical spine due to whole spine degenerative process12). However, it may not be valid for segmental measurements. When we compared cervical parameters of the patients admitted to neurosurgery and emergency clinics, we saw that all cervical parameters except global cervical lordosis (C2-C7) were higher in patients admitted to emergency clinic even though they were younger than the patients admitted to neurosurgery clinic. Global cervical lordosis was still higher in patients admitted to neurosurgery clinic. Segmental vertebral angles (C3 to C7) were higher in our study. This can be due to the differences in the study protocols. As a shortcoming of this study, patients who applied with cervical trauma and/or cervical pain signs and symptoms to our clinics were enrolled into the study. Even though severe cases and obvious pathologies were excluded from the study protocol, we compared our results with the asymptomatic case-series presented in the literature.
We observed that many correlations in the cervical sagittal alignment were involving C4 vertebral corpus (with OC2, C3, C5, T1 slope). This may depict the importance of C4 vertebral corpus position in the cervical spine, which should be considered in surgical treatment planning of patients. There was a significant difference in C4 segmental angle between patients admitted to neurosurgery and emergency clinics. To make a more comprehensible statement, prospective studies with large cohorts of samples representing general population are in need.
T1 slope has gained increased awareness among spine surgeons, recently. Studies about this angle are still limited in the literature. It was found that T1 slope has a significant correlation with cervical alignment and cervical lordosis210). We also observed a positive correlation of T1 slope with both global cervical lordosis and C4 segmental angle.
All spine segments are related with each other and when one of them changes, the others are affected in a contiguous way: increased pelvic incidence leads to increased lumbar lordosis, increased lumbar lordosis leads to increased thoracic kyphosis, increased thoracic kyphosis leads to increased cervical lordosis2). Our study protocol included only cervical A-P and lateral X-rays, which were obtained for clinical evaluation of the relevant patients. So, we could not compare our results in cervical spine with other spinopelvic parameters. However, it is obvious that for a good restoration of cervical alignment in surgical patients, a whole 3-ft spine films from head to upper femoral shaft should be evaluated.
CONCLUSION
In this regional study, it has been observed that global cervical lordosis increases as age increases. C4 vertebra is in the middle of this evaluation as it has many correlations with other cervical segments, which should be kept in mind when making surgical plans for this delicate spine region. To make a more comprehensible statement about asymptomatic general population, more prospective morphometric studies should be made.
ACKNOWLEDGEMENT
Murat Şakir Ekşi, M.D. was supported by a grant from Tubitak (The Scientific and Technological Research Council of Turkey), Grant number: 1059B191400255.