Comparisons of Two-level Discectomy and Fusion with Cage Alone versus Single-level Corpectomy and Fusion with Plate in the Treatment of Cervical Degenerative Disc Disease
Article information
Abstract
Objective
To compare the radiologic parameters and clinical outcomes of two-level anterior cervical discectomy and fusion (ACDF) with cage alone versus single-level anterior cervical corpectomy and fusion (ACCF) with plate in the treatment of two-level contiguous cervical degenerative disc disease.
Methods
Of all 38 consecutive patients who were included in this study, 22 patients underwent on a two-level contiguous ACDF with cage alone (ACDF-CA group), 16 patients underwent a single-level ACCF with plate (ACCF-P group). We compared following parameters between these two groups; perioperative parameters (hospital stays, blood loss and operation duration), clinical parameters (Japanese Orthopedic Association scores and Odom's criteria) and radiologic parameters segmental height ratio (SHR), segmental lordotic angle (SLA), global lordotic angle (GLA) and fusion rate).
Results
The amount of operative blood loss in the ACCF-P group was higher than in the ACDF-CA group with statistical significance (p<0.05). Clinical outcomes and fusion rates were similar between groups. The postoperative SHRs in both groups were higher than that of preoperative period with statistical significance; however, these values significantly decreased at the last follow up period. The SLA increased during the immediate postoperative period, and then mild decreased. The values of GLA in both groups did show variable differences according to each time frame.
Conclusion
The results of ACDF-CA were comparable with ACCF-P with regard to clinical and radiologic outcomes in contiguous two-level cervical fusion. A two-level ACDF-CA as a treatment modality for two-level contiguous cervical disc disease may be a worthwhile method as an alternative to single-level ACCF-P.
INTRODUCTION
Cervical degenerative disc disease is a common cause of neck pain, radiculopathy or myelopathy. Many surgeons have recommended surgical decompression for the treatment of cervical spondylosis associated with medically intractable radiculopathy or myelopathy. Since the publication of a report by Smith and Robinson16), anterior cervical discectomy and fusion (ACDF) has been widely accepted as the golden standard for surgical treatment of cervical degenerative disc disease. However, its success rate declines in multi-level discectomies as the number of operated levels increases3). The optimal surgical treatment, therefore, still remains controversial for the patient with multi-level cervical spondylosis. They can be treated with either multi-level ACDF or anterior cervical corpectomy and fusion (ACCF). However, it is also not clear whether multi-level cervical spondylosis is the best treated with multi-level ACDF or single/multi-level ACCF.
Clinical results of the application of interbody cages to the multi-level ACDF in patients with cervical degenerative disc disease have been encouraging6,18,20). Further, ACDF with cage alone has been reported to have produced relatively good results3,8,9,11,19,21). However, controversy remains with regard to fusion rate, subsidence, pseudoarthrosis in association with ACDF with cage alone compared with plate augmentation in ACDF5). There have few studies on two-level contiguous ACDF reporting that the results of ACDF with cage alone would be comparable with ACDF with plate8,9,11,19). However, the National Health Insurance Corporation does not approve of two-level contiguous ACDF with cage alone on the ground of cost effectiveness and lack of evidences for positive clinical results. Therefore, many spine surgeons usually practice single-level ACDF with cage alone. However, ACCF with plate instrument is the usual choice of treatment of two-level contiguous cervical disc disease since ACDF with cage alone is not applicable in such cases.
There are few comparative studies of two-level contiguous ACDF and single-level ACCF with plate augmentaion13,14,22). However, there is no direct comparison between two-level ACDF with cage alone and single-level ACCF with plate instrument. The purpose of this study was to compare the perioperative, clinical and radiologic parameters between the two operation methods, two-level ACDF with cage alone and single-level ACCF with plate, in the treatment of two-level contiguous cervical degenerative disc disease.
MATERIALS AND METHODS
We retrospectively reviewed the records of 75 patients who underwent two-level contiguous anterior cervical fusion from September 2002 to August 2010. Among them, patients with less than 6 months of postoperative follow-up were excluded from this study. Other patients who had severe trauma, infectious or neoplastic cases, or underwent combined posterior or other procedures were also excluded. Only 38 patients who had cervical degenerative disc disease were included in this study. Subjects were divided into two groups. 22 patients underwent two-level contiguous ACDF with cage alone (ACDF-CA group) and 16 patients underwent single-level ACCF with plate instrumentation (ACCF-P group) for the treatment of cervical degenerative disc disease. Indication for surgery included intractable radiculopathy, myelopathy, or a combination of the two, due to nerve root or spinal cord compression. The cervical spondylosis and degenerative disease was diagnosed by means of cervical X-ray, computed tomography and magnetic resonance imaging.
The choice of operation was dependent on the presence or absence of retrovertebral compression. Corpectomy was chosen if the compression was considered to be removed more easily using it, and it was also considered the patients with a large posterior osteophyte adjacent to end plate. Otherwise, ACDF was chosen. Surgical procedure was performed according to the standard anterior approach described by Smith and Robinson16). All the patients in the ACDF-CA groups underwent two-level contiguous ACDF without anterior plate. In all 22 patients in the ACDF-CA group, an optimal PEEK cage filled with allograft (12 patients) or autograft (10 patients) bone was used. In ACCF-P group, 13 patients were treated by inserting a mesh cage which was filled with autograft (10 patients) or allograft (3 patients) bone. Autologous iliac bone block was also used in 3 patients. A Philadelphia collar placed in all patients in both groups for 6-8 weeks postoperatively.
Radiological follow-up was performed during the preoperative period and 1 day and 3 months postoperatively, as well as during the last follow-up visit. Lateral X-rays were used to evaluate the cervical spinal curve and the height ratio of fused segments. Segmental height ratio (SHR) was measured by dividing the segmental height of fused segments by antero-posterior diameter of the mid-vertebral body (Fig. 1). Segmental lordotic angle (SLA) was measured using Cobb's angle between the upper endplate of the most cranial vertebral body and the lower endplate of the most caudal vertebral body of the fused segments (Fig. 2). Global lordotic angle (GLA) was measured using Cobb's angle between the inferior endplate of the C2 vertebral body and the inferior endplate of the C7 vertebral body (Fig.3).
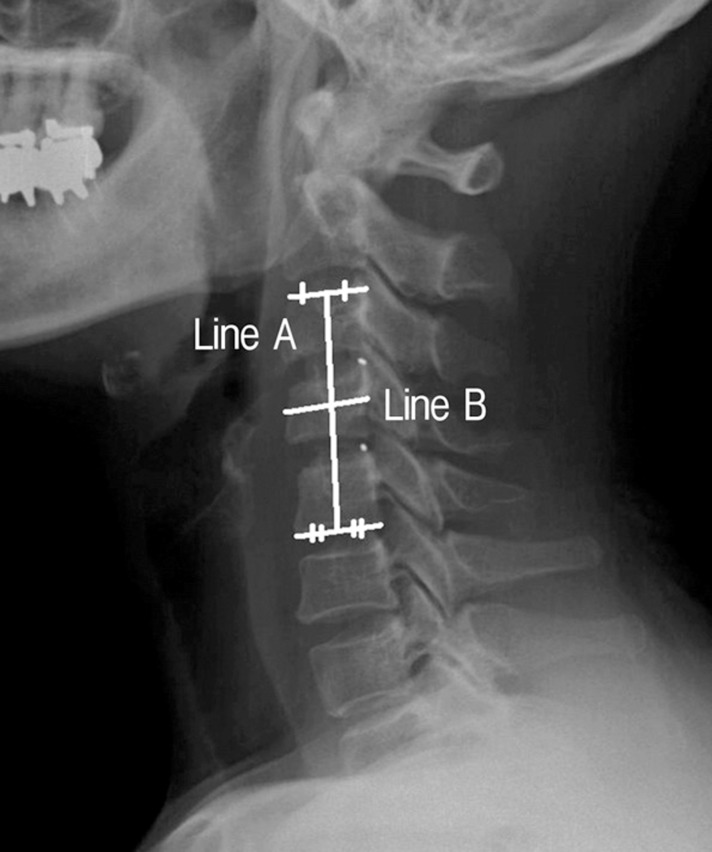
Lateral radiograph of cervical spine showing the segmental height ratio (SHR) measuring method. Segmental height ratio=segmental height (line A)/AP diameter of the mid vertebral body (line B).

Lateral radiograph of cervical spine showing the segmental lordotic angle (SLA) measuring method. There is a Cobb's angle between the upper endplate of the vertebral body and the lower endplate of vertebral body of the fused segment.
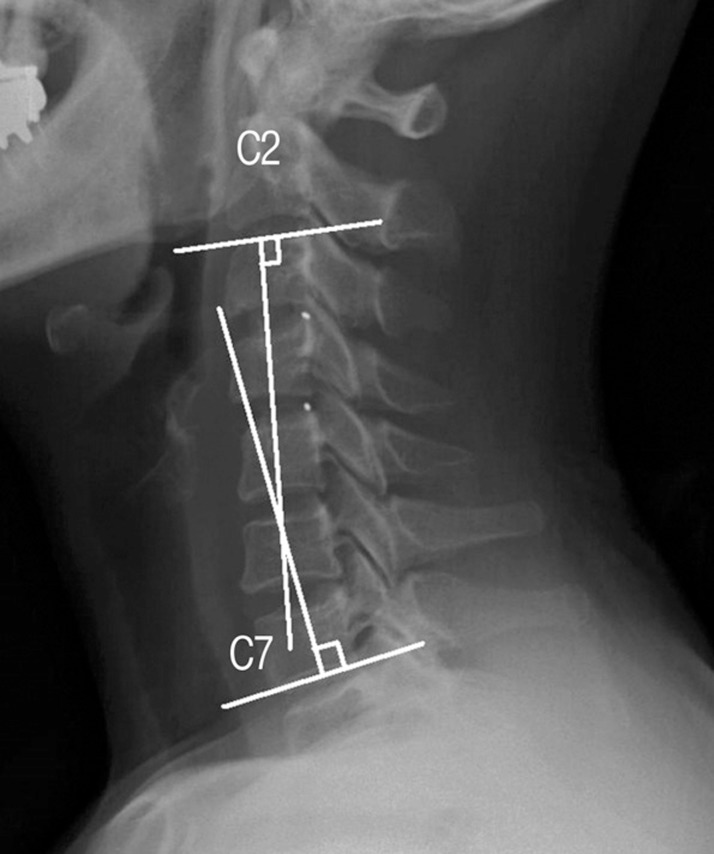
Lateral radiograph of cervical spine showing the global lordotic angle (GLA) measuring method. There is a Cobb's angle between the lower endplate of the C2 vertebral body and the lower endplate of C7 vertebral body.
Subsidence was defined as a graft material subsided more than 3mm into the adjacent vertebral endplate on lateral plain radiographs. Fusion was defined as the absence of motion on flexion/extension radiographs and the absence of any dark halo around graft bone or cages, or presence of bridging bone anterior or posterior to cages or bone graft. Clinical follow-up was performed consisting of standard neurosurgical examinations and evaluations using Japanese Orthopedic Association (JOA) score and Odom's criteria.
We compared following parameters between the two groups; perioperative parameters (hospital stays, blood loss and operation duration), clinical parameters (JOA scores and Odom's criteria) and radiologic parameters (SHR, SLA, GLA and fusion rate). Data were recorded and statistical analysis performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). Data were presented as mean±standard deviation. Since the number of specimens was limited and the data could not be assumed to be normally distributed, Mann-Whitney rank sum and Chi-Square test were used to analyze the differences in perioperative parameters and clinical outcomes between groups. For radiologic parameters, comparison between two groups was performed using Mann-Whitney test. Comparison between the results for each time frame within each group was performed using Wilcoxon signed ranks test because the number of specimens was small; however, comparison between the results for each time frame of total specimens for each parameter was performed using paired t-test because there was sufficient number of specimens which were normally distributed. Significance of difference was determined when the probability level p<0.05.
RESULTS
ACDF-CA group consisted of 12 males and 10 females with mean age 56.5±16.5 years. Among them, 13 patients had radiculopathy and 9 patients had myelopathy. Duration of the follow up period was 27.5±12.3 months. ACCF group consisted of 11 males and 5 females with mean age 57.1±15.0 years. Among them, 5 patients had radiculopathy and 11 patients had myelopathy. Mean follow-up period was 22.7±9.7 months. Demographic information of the patients and their locations of treated levels are shown in Table 1.
1. Perioperative parameters
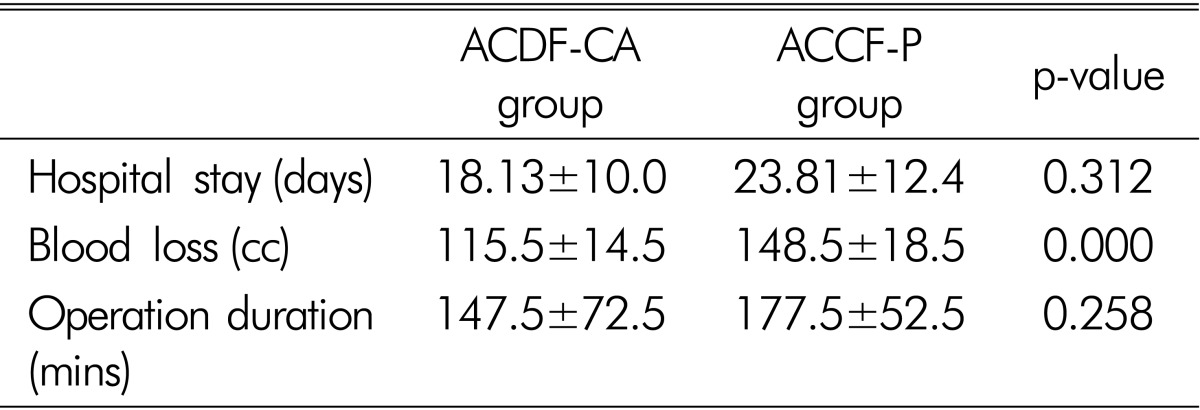
Duration of hospital stay was 18.13±10.0 days for patients in ACDF-CA group and 23.81±12.4 days for patients in ACCF-P group with no statistically significant intergroup difference. Mean blood losses during operation were estimated to be about 115.5±14.5 cc for ACDF-CA group and 148.5±12.4 cc for ACCF-P group. The amount of blood loss in the ACCF-P group was higher than that of the ACDF-CA group during operation with statistical significance (p<0.05). The mean duration of operation was 147.5±72.5minutes for ACDF-CA group and 177.5±52.5minutes for ACCF-P group. The patients in ACCF-P group seemed to have required longer times for operation than that those in ACDF-CA group, with no statistically significant difference, however (Table 2).
2. Clinical parameters
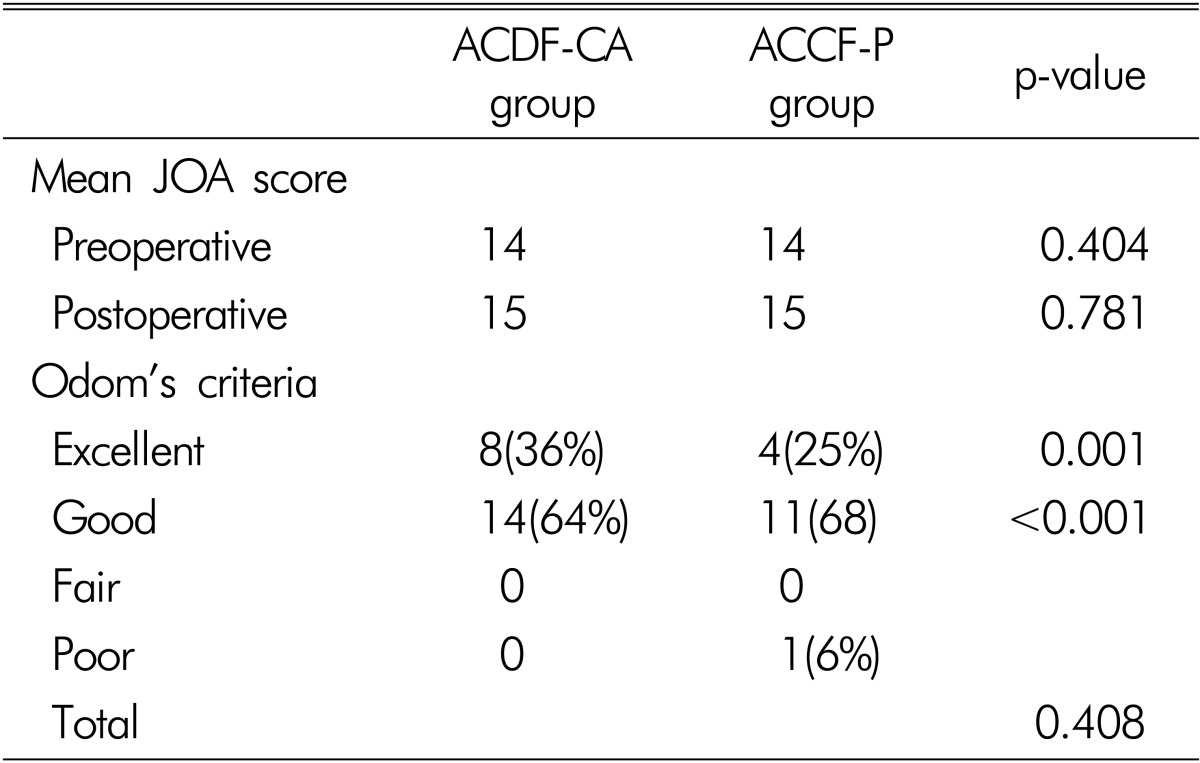
For all patients in two groups, mean JOA score was 14 points preoperative and 15 points postoperative with no statistically significant difference. Postoperative outcome was shown to be higher by one point in both groups (Table 3). Evaluation of Odom's criteria revealed that all patients except one in both groups clinically improved. However, worsening occurred in one patient who underwent ACCF-P procedure. There also was no statistically significant difference between groups.
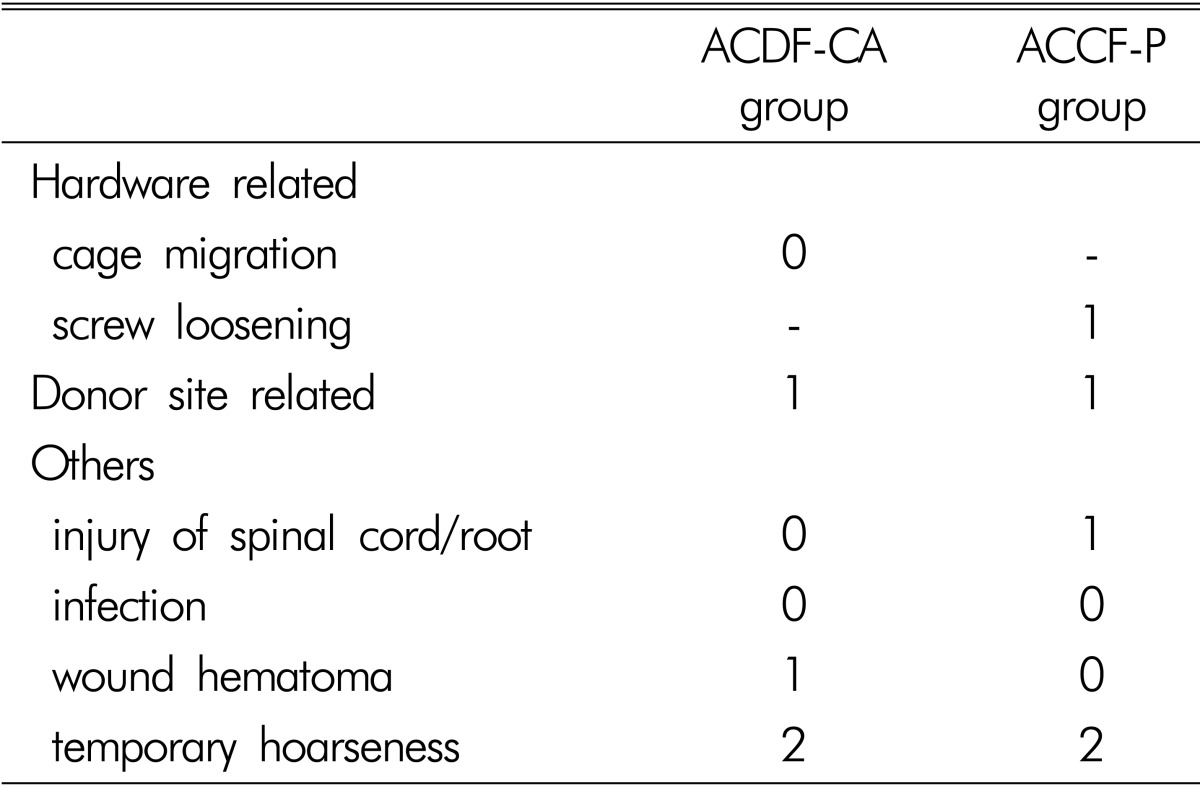
Postoperative complications were observed transient hoarseness in the each 2 cases of both groups, hardware related complications were developed a case of screw loosening in ACCF-P, they were not in the ACDF-CA group (Table 4).
3. Radiologic parameters
A summary of radiologic outcomes is shown in Fig. 4 and Table 5. SHR increased during immediate postoperative period in both groups. However, it progressively decreased during follow up period. Preoperative, immediate postoperative and last follow-up SHR was 2.64±0.57, 2.81±0.52 and 2.77±0.72, respectively, in ACDF-CA group and 2.79±0.35, 3.06±0.67 and 2.74±0.33, respectively, in ACCF-P group. Immediate postoperative SHR was higher than that of preoperative time (p=0.001 for the ACDF-CA, 0.020 for the ACCF-P group) with statistical significance. However, it decreased significantly at the last follow-up period (p=0.028 for ACDF-CA group, 0.026 for ACCF-P group). SHR decreased more in ACCF-P group than in ACDF-CA group. But it did not show statistically significant difference between the two groups. Comparing with immediate postoperative period, more than 3mm subsidence occurred in 7 segments (16%) of total 44 segments of ACDF-CA group, in 2 segments (13%) of 16 segments of ACCF-P group. Among them, there was no case with clinical worsening.
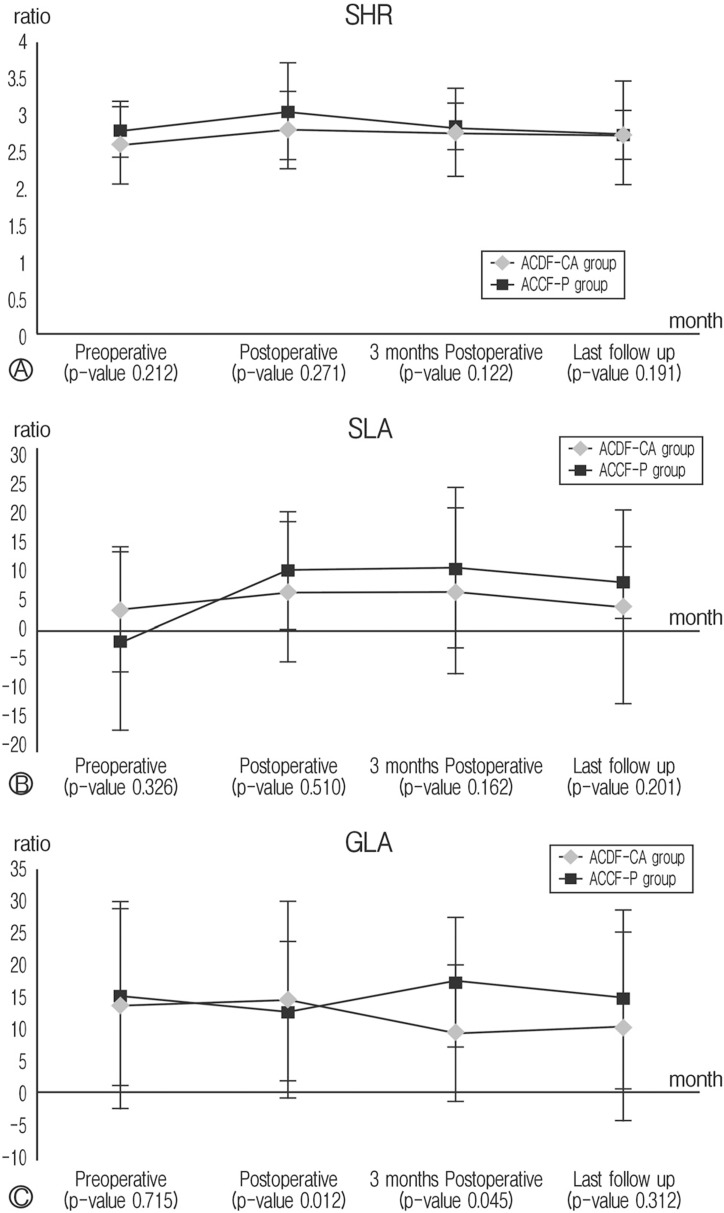
Line graphs showing comparisons of radiologic parameters between two groups. There are segmental height ratio (A), segmental lordotic angle (B) and global lordotic angle (C). Data are represented as mean±standard deviation. The p-values were derived from comparison between groups using Wilcoxon signed ranks test.
SLA increased during the immediate postoperative period compared with preoperative period. But it did not show statistically significant difference between groups and between each time frame within the same group except the total comparison between preoperative and immediate postoperative periods. There were also no statistically significant differences between groups and between each time frame within the same group. GLA in ACDF-CA group was significantly larger than that in ACCF-P group during immediate postoperative period (p=0.012). However, GLA in ACCF-P group was significantly larger than that in ACDF-CA group in 3 months postoperative. Other values of GLA did not show statistical significant differences between groups and between each time frame within the same group.
All patients included in the two groups of this study showed fusion except one in simple X-ray. A case of ACDF-CA group was suspected psuedoarthrosis. However, she is clinically stable; our observation is still ongoing more than 1 year.
DISCUSSION
Surgical treatment of multi-level cervical spondylosis is a challenging process. The optimal surgical treatment for the patient with multi-level cervical spondylosis still remains controversial. The choice of surgical treatment could be either multi-level ACDF or ACCF. It is also not clear which of multi-level ACDF or single/multi-level ACCF is better surgical treatment for multi-level cervical spondylosis. Compared with multi-level ACDF, ACCF has resulted in high fusion rates because there are only two fusion surfaces4,10). ACCF is also associated with early hardware failure15). To overcome these problems, various methods and instruments for anterior cervical spine fusion have been developed. Recently, the use of anterior cervical plate with or without cage in ACCF and ACDF procedures has become popular and been regarded as a standard practice.
In multi-level ACDF, augmentation with plate fixation may seem preferable due to higher fusion and lower reoperation rates and better clinical outcomes3,23). In spite of these benefits, plate-related complications including screw pullout, screw breakage, injury of laryngeal nerve, injury of esophagus, prolonged dysphagia, injury of cord or root and wound infection occurred at varied rates from 2.2 to 24%2,3). Additionally, operation using plate fixation usually takes longer9,19). The clinical results of the applications of interbody cages in multi-level ACDF have been encouraging6,18,20). Furthermore, ACDF with cage alone has been reported with relatively good results3,8,9,11,19,21). However, controversy over ACDF with cage alone remains with regard to its fusion rate, subsidence and pseudoarthrosis compared with plate augmentation in ACDF5). There have been few studies reporting that the results of ACDF with cage alone would be comparable with those of ACDF with plate in two-level contiguous ACDF8,9,11,19). Lee et al.9) reported that the use of two-level stand alone cages in ACDF yielded excellent fusion rate and clinical outcomes in spite of subsidence. Joo et al.8) suggested that routine use of plate and screw in two-level ACDF may not be beneficial.
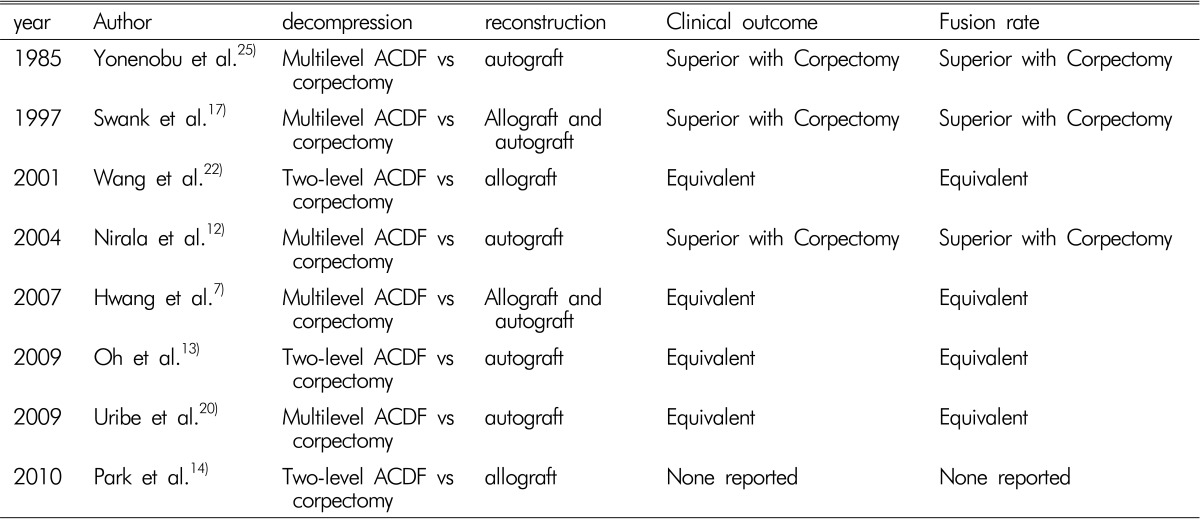
To the best of our knowledge, there have been a few studies comparing single/multi-level ACCF and ACDF in terms of clinical results and fusion rates (Table 6)7,9,13,14,17,20,22,25). In early reported series12,17,23,25), ACCF showed superior results compared with ACDF except in one report. Interestingly, Wang et al.22) reported that the addition of cervical plates in either two-level disectomies or single-level corpectomy yielded similar clinical results and fusion and complication rates. It may be because comparison was made only between single-level ACCF and two-level ACDF and because anterior plate augmentation was used. However, in recent reported series7,13,20), these two procedures yielded similar results in terms of fusion rate and clinical outcomes. We suggest that their observations be used as valuable references in using and developing instruments such as plate or cage in ACCF and ACDF procedures.
Hwang et al.7) reported that the absence of donor site complications and construct failures as well as shorter hospital stay would render the multi-level ACDF with cage and plate fixation preferable to ACCF with strut graft and plate fixation. Oh et al.13) reported that, although these two surgical procedures were found to be similar to each other in terms of clinical outcomes, two-level ACDF was found to be superior to single-level ACCF in terms of operation duration, amount of bleeding, preserved segmental height and postoperative cervical lordosis. Uribe et al.20) postulated that ACCF resulted in a higher rate of early hardware failure and psudoarthroses than ACDF, and thus in the absence of pathology requiring removal of vertebral body, ACDF could result in lower morbidity. Park et al.14) observed that graft subsidence and the loss of cervical lordosis appeared to occur mainly during the first 6 weeks after the surgery in both procedures. ACCF continued to subside at the posterior portion of caudal end plateeven after 6 weeks. However, the results of our study are some what different from others. They used a plate augmentation either in ACDF or ACCF. Surgical procedures in our study, however, were performed without plate in ACDF or with plate in ACCF. According to our retrospective review, in two-level contiguous cervical fusion, ACDF-CA was comparable with ACCF-P with regard to clinical and radiologic results with no significant difference. However, significant differences were observed between these two groups in terms of blood loss. Judging from the result of SHR, subsidence progressed after the surgery with statistically significant difference between the two groups. Segmental height decreased more in ACCF-P group than in ACDF-CA group without statistically significant difference. SLA is mildly reduced in similar pattern as SHR, postoperatively. Despite decreases in segmental height and segmental lordosis, they did not affect global cervical lordosis. These results support the observation that graft subsidence is not correlated with sagittal alignment and clinical outcome1,14), and that global cervical lordosis is correlated with clinical outcomes24). Our results, variable values of GLA according to time frame, represent that global cervical lordosis is correlated with clinical outcomes. All patients of both groups showed fusion except one in simple X-ray. These results are relatively higher than others. We are thinking about possibility of that our fusion rates are likely to have been overestimated because of inclusion criteria of this study. They are that the patients with less than 6 months of postoperative follow-up and underwent combined posterior procedures were excluded from this study. Indeed, three cases with posterior combined procedures, 2 early hardware failures and 1 early collapse were excluded from this study.
There are some limitations in this study. Short follow-up period and a small number of subjects did not allow thorough evaluation. Being a retrospective study, it was not performed as a randomized, controlled trial study. Therefore, long term follow-up and a prospective randomized study including a large subject population are required in the future.
CONCLUSION
Our results suggest that there are no clear benefits of ACCF-P over ACDF-CA in terms of clinical and radiologic outcomes in two-level contiguous cervical fusion. However, two-level ACDF-CA was found to be superior to ACCF-P in terms of the amount of bleeding. Therefore, we conclude that two-level ACDF-CA may be a worthwhile method and may be used as an alternative to single-level ACCF-P, in the absence of retrovertebral compression, as a treatment modality for two-level contiguous cervical disc disease.