INTRODUCTION
Infectious spondylitis is defined as an infection by a specific organism of one or more components of the spine, namely the vertebra, intervertebral discs, paraspinal soft tissues, and epidural space16). Infectious spondylitis represents 2-4% of all cases of osteomyelitis. Males are affected more frequently than females (ratio of 2 to 1), usually in the fifth to sixth decades, but it may appear at any age17). Although infection can be caused by pyogenic, granulomatous, autoimmune, idiopathic, and iatrogenic conditions, pyogenic spondylitis is the most common spinal infection, and tuberculosis continues to be a major problem in developing countries and is resurgent in Western world with the onset of human immunodeficiency virus (HIV)13).
The clinical differentiation of pyogenic and tuberculous spondylitis is important because the medications used to manage these infections are notably different. Early diagnosis and prompt treatment are essential to prevent permanent neurologic deficit and spinal deformity5,11). However, it is difficult to differentiate tuberculous spondylitis from pyogenic spondylitis clinically and radiolgically3,16). Magnetic resonance (MR) imaging has been useful in the detection of spinal disorders, and its high sensitivity in detecting early changes has been valuable12). The purpose of our study was to evaluate the MR imaging feature differentiating tuberculous spondylitis from pyogenic spondylitis.
MATERIAL AND METHOD
1. Patient population
MR images of the spines of 41 patients with infectious spondylitis at our institution over 8-years of period were retrospectively reviewed. After the medical record review, 18 patients with infective spondylitis were excluded because their results on the marrow biopsy and culture were negative. All 17 cases of pyogenic spondylitis and 6 cases of tuberculous spondylitis were confirmed by biopsy and culture. The patient comprised 17 with pyogenic spondylitis (10 male, 7 female) and 6 with tuberculous spondylitis (3 male, 3 female). The mean age of the patient with pyogenic spondylitis and tuberculous spondylitis was 63.6 years (range 51-78 years) and 49.2 years (range 29-74 years), respectively. The mean interval from presentation to MR imaging was 7 weeks (range 1-14 weeks) in patients with pyogenic spondylitis and 26 weeks (range 1 week - 24 months) in patients with tuberculous spondylitis.
2. MR imaging
MR imaging was performed on 1.5-T imager (Intera, Philips Medical Systems), using a surface coil or spine coil. Axial and sagittal T1-weighted MR images and fast spin-echo or turbo spin-echo T2-weighted images were obtained. In addition, axial, sagittal and coronal fat-suppressed T1-weighted images were obtained after IV infusion of 0.1mmol/kg of dimeglumine gadopentetate. Typical MR parameters were as follows: field of view, 140-280mm for axial plane, 300mm for sagittal plane and 344 mm for sagittal plane; number of excitations, 2; slice thickness, 4 mm and intersection gap, 4mm.
RESULTS
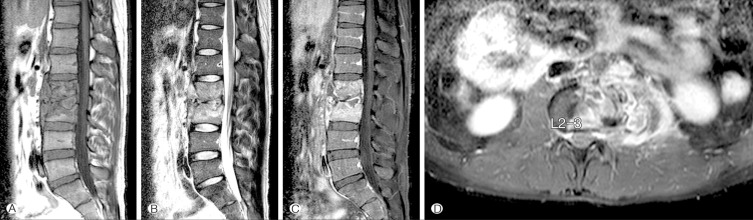
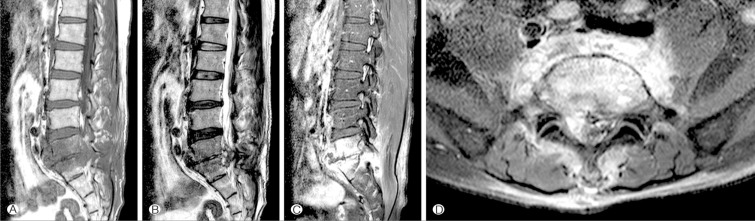
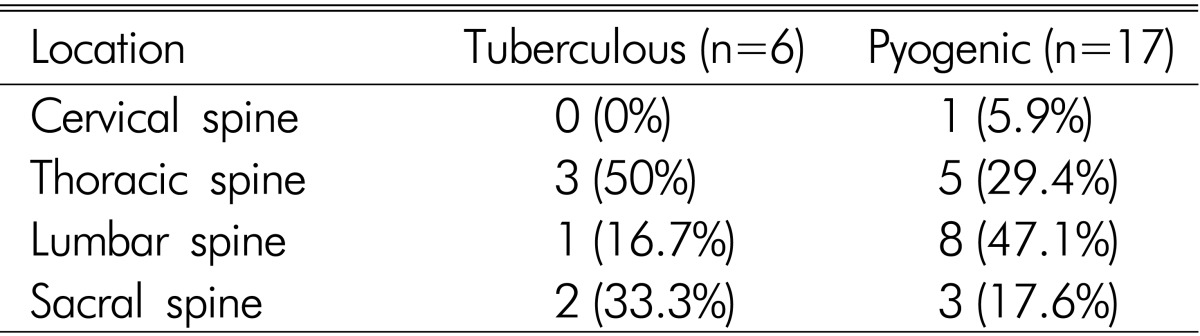
The tuberculous spondylitis (Fig. 1) group consisted of 3 males (50%) and 3 females (50%). Whereas, the pyogenic spondylitis (Fig. 2) group consisted of 10 males (58.8%) and 7 females (41.2%). The location that each spondylitis is involved is summarized in Table 1. Thoracic spine was the most common site of tuberculous spondylitis involvement.
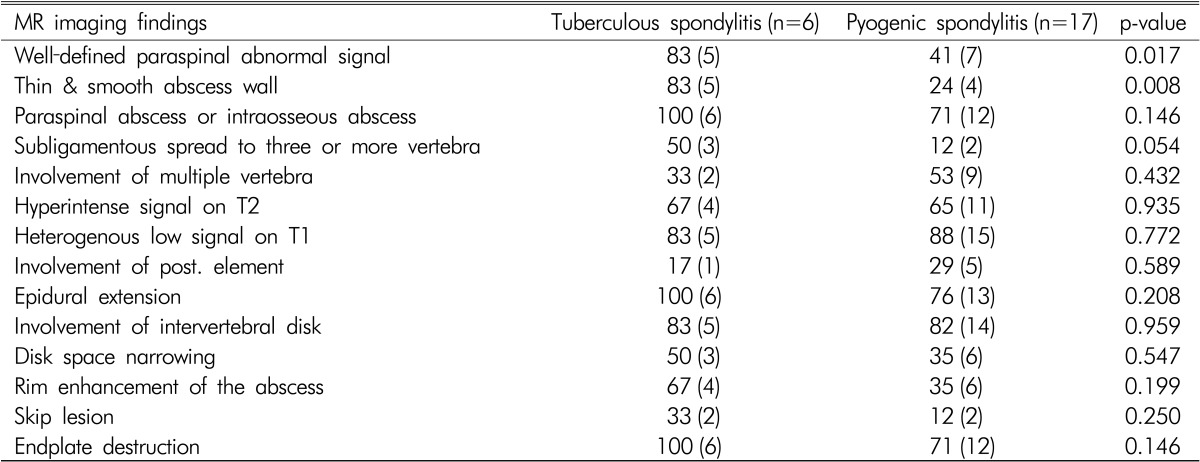
The mean affected verterbra number was 2.67 (range 2-4) in tuberculous spondylitis and 2.88 (range 2-4) in pyogenic spondylitis. The results of the imaging findings for tuberculous spondylitis and pyogenic spondylits are summarized in Table 2.
The incidence of the following MR imaging findings was singnificantly higher in patients with tuberculous spondylitis than in those with pyogenic spondylitis (p<0.05): a well defined paraspinal abnormal signal (83% in tuberculous vs 41% in pyogenic) and a thin and smooth abscess wall (83% vs 24%). There were no significant differences in the following MR imaging findings : paraspinal abscess or intraosseous abscess (100% in tuberculous vs 71% in pyogenic, p=0.146), subligamentous spread to three or more vertebra (50% vs 12%, p=0.054), involvement of multiple vertebra (33% vs 53%, p=0.432), hyperintense signal on T2-weighted images (67% vs 65%, p=0.935), heterogenous low signal on T1-weighted images (83% vs 88%, p=0.772), involvement of posterior element (17% vs 29%, p=0.589), epidural extension (100% vs 76%, p=0.208), involvement of intervertebral disk (83% vs 82%, p=0.959), disk space narrowing (50% vs 35%, p=0.547), rim enhancement of the abscess (67% vs 35%, p=0.199), skip lesion (33% vs 12%, p=0.250), and endplate destruction (100% vs 71%, p=0.146).
DISCUSSION
The incidence of typical acute vertebral osteomyelitis has decreased because of the more wide spread use of antibiotics. However, tuberculous spondylitis is still a frequent cause of infectious spondylitis in endemic regions and is increasing in prevalence because of the resurgence of tuberculosis during the past decades, especially in patients who are immunocom-promised3,13,15,16).
The clinical differentiation of pyogenic and tuberculous spondylitis is important because the medications are definitely different6). However, differentiation between tuberculous and pyogenic spondylitis is difficult clinically and radiographically12). MR imaging has been reported to be useful in the early detection of spondylitis1,3,9,20). There have been several reports about the differences on MR imaging findings between tuberculous spondylitis and pyogenic spondylitis. We also studied on the differences on MR imaging findings. We demonstrated that the two MR imaging findings, a well defined paraspinal abnormal signal (83% in tuberculous vs 41% in pyogenic) and a thin and smooth abscess wall (83% vs 24%) are reliable suggesting tuberculous spondylitis in our study. Our study is corresponding to Jung et al.12) The smoother margin of the paraspinal abnormal signal and a thinner and smoother abscess wall are due to the relative late phase and chronic course of tuberculous spondylitis12). The minimal inflammation of tuberculous abscess also might be the reason to the thin and smooth appearance of abscess wall12). Rim enhancement of abscess on MR imaging suggested the tuberculous spondylitis by other reports1,3,15,16,21). However, rim enhancement (67% in tuberculous vs 35% in pyogenic) in our study had no stastically singnificant difference (p=0.199). This finding is supported by Jung et al. 12).
Lack of proteolytic enzymes in Mycobacterium as compared with pyogenic agents of infection has been proposed as the cause of the relative preservation of the intervertebral disks3,8,18). However, the results of our study showed disk space narrowing in 50% of patients with tuberculous spondylitis and 35% of those with pyogenic spondylitis. This difference is not statistically significant (p=0.547). We assume that the disk space narrowing might be attributable to other factors such as a lumbar disk degeneration10).
Subligamentous spread to three or more vertebral levels in tuberculous spondylitis is frequent9,21). Infection may extend from an anterior lesion of the vertebral body beneath the anterior longitudinal ligament to the anterior parts of neighboring intervertebral disk and vertebral bodies10). However, in our study, subligamentous spread was observed in 50% of patients with tuberculous spondylitis as compared with 12% of those with pyogenic spondylitis. There was no statistically difference (p=0.054). These discrepancies might be due to the small number of patients in our study. Involvement of the posterior element has been reported in tuberculous spondylitis and very uncommonly in pyogenic spondylitis3,15,18). Our study findings were not corresponding to these previous report, 17% in tuberculous vs 29% in pyogenic spondylitis, especially statistically no difference (p=0.589).
Chang et al.6) reported distinguishing the tuberculous spondylitis and pyogenic spondylitis was difficult by using only T2-weighted images. Like Chang et al.6), Our study findings are no differences between the two groups in T2 signal intensity. There are several limitations associated with this study reported here. The sample size was small. Especially, the number of the patients with tuberculous spondylitis was six, because tuberculosis has been reduced in developed countries in the past 30 years, as a consequence of a precocious diagnosis and mostly with anti-bacillary therapeutics2). Tuberculosis of spine also accounts for 1% of all tuberculosis infection21). Also rates for isolating the causative organism are less than 50% in tuberculous spondylitis and 60-80% for pyogenic spondylitis4,7,14). Morever, histopathologic evaluation of biopsy material does not always provide a specific diagnosis19,21).