Feasibility of Full Endoscopic Spine Surgery in Patients Over the Age of 70 Years With Degenerative Lumbar Spine Disease
Article information
Abstract
Background/Aims
Degenerative spine disease, encompassing disc prolapse and stenosis, is a common ailment in old age. This prospective study was undertaken to evaluate the role of endoscopic spine surgery in elderly patients (above 70 years of age) with clinical and radiological follow-up.
Methods
In this study, a retrospective analysis was conducted of 53 patients with lumbar disc prolapse or spinal stenosis who were treated with percutaneous endoscopic discectomy or decompression from November 2015 to June 2017. Clinical follow-up was done at 1 week, 3 months, and 1 year, and at yearly intervals thereafter. The outcomes were assessed using the modified Macnab criteria, a visual analogue scale, and the Oswestry Disability Index.
Results
Of the 53 patients, 21 were men and 32 were women. Their mean age was 76±4 years. The mean follow-up period was 17 months. Percutaneous endoscopic discectomy was performed in 24 patients and endoscopic decompression in 24 patients, while 5 patients underwent combined surgery. An excellent outcome in terms of the MacNab criteria was observed in 9 patients (16.98%), a good outcome in 38 patients (71.7%), and a poor outcome in 6 patients (11.3%). Of the 6 patients with a poor outcome, 5 (9.4%, 5 of 53) developed recurrent disc prolapse, and 1 developed hematoma with motor weakness. All 6 of these cases required revision surgery.
Conclusion
Managing degenerative spine disease in elderly patients with multiple comorbidities is a challenging task. Percutaneous endoscopic spine surgery is pivotal for addressing this concern. The authors have shown that optimal results can be achieved with various types of disc prolapse and stenosis with favorable long-term outcomes.
INTRODUCTION
Lumbar degenerative spine disease affects the majority of the population in all societies with variable outcomes in old age. The multiple comorbidities that exist have an important bearing on the outcome of prolonged spine surgery [1-3]. At this age, the physical incapacities and comorbid illness make any intervention in the form of surgery a challenging task. The rate of complication after spine surgery may be as high as 35% [1]. The overall quality of life frequently gets hampered after open spine surgery [4,5], and with increasing longevity nowadays it is all the more a matter of concern.
There have been numerous reports on the benefit of endoscopic spine surgery for lumbar disc prolapse and spinal stenosis. Not only is the surgery performed with a small incision that helps early recovery, but overall hospital stay is significantly shorter and quality of life is improved [6-9]. So far, there has been no mention of the role of endoscopic spine surgery in old age patients, especially above 70 years of age. We undertook this prospective study on patients above 70 years of age who presented with various problems pertaining to spine and were offered surgical interventions in form of percutaneous endoscopic spine surgery (PESS). The clinical and radiological follow up along with the quality of life was assessed in all the patients. Endoscopic spine surgery has a definite role in old age patients by helping to improve quality of life with a minimal disability.
MATERIALS AND METHODS
The study is based on retrospective analysis of 53 patients with lumbar degenerative spine disease, over 70 years of age that were managed at Nanoori Hospital from November 2015 to June 2017. This study was approved by the Institutional Review Board of Nanoori Hospital (approval number: 2018-006). Xray imaging, computed tomography (CT), and magnetic resonance imaging (MRI) were done in all cases to confirm the diagnosis and to rule out other pathologies. The findings demonstrated on the CT and MRI scans were correlated with the neurologic examination. After proper diagnosis patients underwent surgery by endoscopic route-percutaneous endoscopic transforaminal lumbar discectomy (PETLD), percutaneous endoscopic interlaminar lumbar discectomy (PEILD), percutaneous endoscopic transforaminal lumbar foraminotomy (PETLF), and percutaneous endoscopic stenosis lumbar decompression (PESLD). We used local anesthesia for transforaminal procedures, epidural anesthesia for interlaminar procedures. When antithrombotic drugs are discontinued in the days before a surgical procedure, the risk for perioperative bleeding may decrease, whereas the risk of thromboembolic events rises. Therefore, we usually individualize this protocol for each patient after consulting with our cardiologist and anesthetist. In general, we stop aspirin for 5 days and clopidogrel for 7 days before surgery in patients without major risk factors like stent thrombosis.
The exclusion criteria were the presence of segmental instability and spondylolisthesis more than grade 1. A written informed consent was obtained from all the patients. PETLD and PETLF surgery were performed under local anesthesia, while epidural anesthesia was administered for PESLD and PEILD. PETLD and PETLF were performed for lumbar disc L1–2 to L4–5, PEILD for L5–S1 disc, PETLF for foraminal disc, and PESLD for stenosis.
Considering thin and fragile epidural blood vessels and dura, decompression was performed with additional care. We tried to minimize the duration of surgery and all surgeries performed by our senior spine surgeon with 10 years of experience and have performed 3,000 endoscopic spine surgeries. MRI was done in all the patients on the day following surgical intervention.
Outcome was measured by visual analogue scale (VAS) leg pain score, Oswestry Disability Index (ODI), and the MacNab criteria. These were measured in the preoperative period and at follow up visit (1 week and 3 months and at last follow-up). The significance level was considered at 0.05. Statistical software used for the study was IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA).
RESULTS
PESS performed in 53 patients. Of 53 patients 21 were men and 32 were women. The mean age of the patients enrolled in the study was 76 years (range, 70–88 years) and male/female ratio was 2:1.3 (Table 1). The mean follow-up of enrolled patients was 17 months (range, 8–29 months). Percutaneous endoscopic discectomy by transforaminal or interlaminar route was performed in 24 patients, endoscopic decompression in 24 patients while 5 patients underwent combined discectomy and decompression surgery. Total 62 levels were treated with 29 patients at L4–5 (46.8 %) level, 15 at L3–4 (4.2%), 11 at L5–S1 (17.7%), 6 at L2–3 (9.7%) and 1 at L1–2 (1.6%). Nine patients had undergone surgery at 2 levels (16.9%) whereas the remaining patients had undergone surgery at single level.
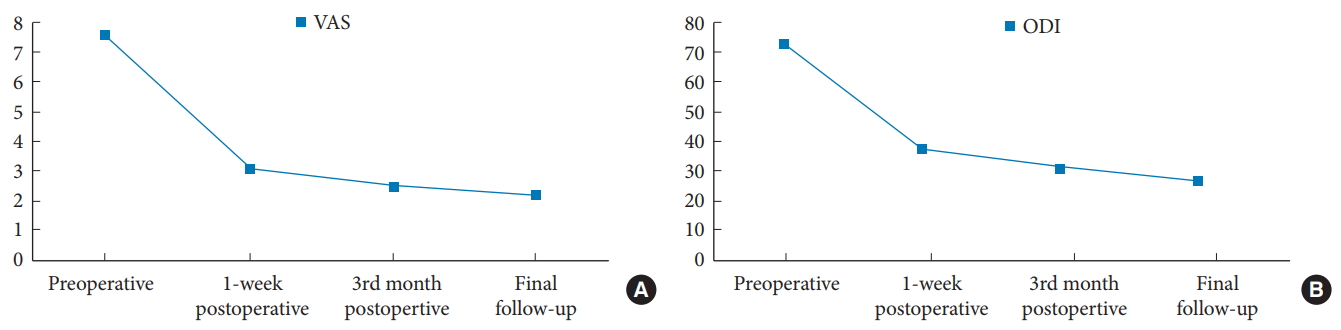
The preoperative VASleg score on the affected side was 7.6±1.1 (range, 6–10) and the postoperative VASleg score improved to 3.1±0.9 (range, 2–6). The improvement was significant at p<0.0001 (Table 2). Significant improvement was maintained at the third month and at final follow-up with VASleg scores of 2.5±0.9 (range, 1–5; p<0.0001) and 2.2±0.9 (range, 1–5; p<0.0001), respectively (Fig. 1A). ODI scores change from 73.4±7.4 (range, 48–86) preoperatively to 37.5±7.9 (range, 25–68) postoperatively (p<0.0001). Significant improvement was maintained at the third month postoperatively and at final follow-up with ODI scores of 31.4±8.2 (range, 22–56; p<0.0001) and 26.8±6.2 (range, 16–44; p<0.0001), respectively (Fig. 1B). An excellent outcome on MacNab criteria was noted in 9 patients (16.98%, 9 of 53), a good outcome in 38 patients (71.7%, 38 of 53), poor results in 6 patients (11.3%, 6 of 53). Average duration of surgery was 48±12 minutes (range, 35–90 minutes).
Out of these 6 patients with poor results, 5 patients (9.4%, 5 of 53) developed recurrent disc prolapse, one patient (without history of any antithrombotic drug) developed hematoma with motor weakness which required open irrigation. Out of the 5 patients with recurrent disc prolapse: 1 case converted to PESLD with a discectomy, 2 cases revision PETLD and 2 cases converted to TLIF. There was no injury to facet joint during index surgery in all these 5 patients and index surgery was discectomy, which less likely cause’s facet injury both in transforaminal and interlaminar approach in our technique [6-9]. The 2 patients in whom we performed fusion surgery had grade I spondylolisthesis before index surgery, which got aggravated in follow-up period.
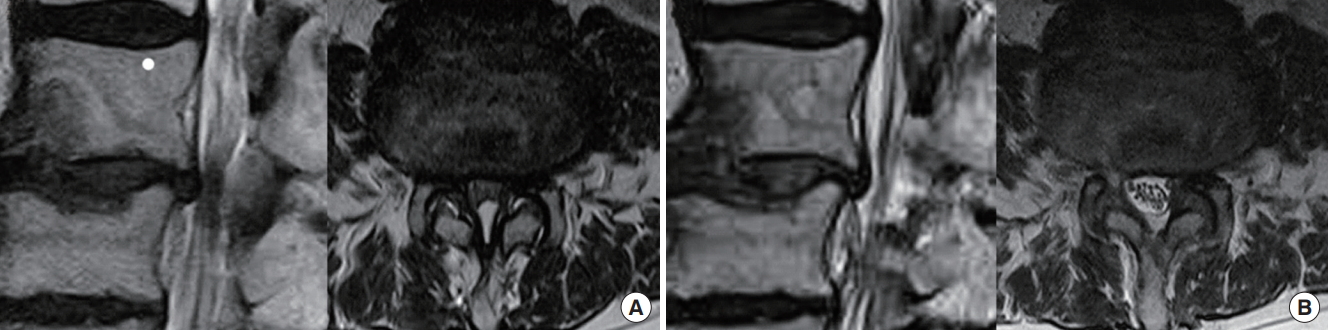
Postoperative MRI showed adequate decompression of the pathologic segment in 46 patients (86.8%) with these endoscopic procedures (Figs. 2-5).
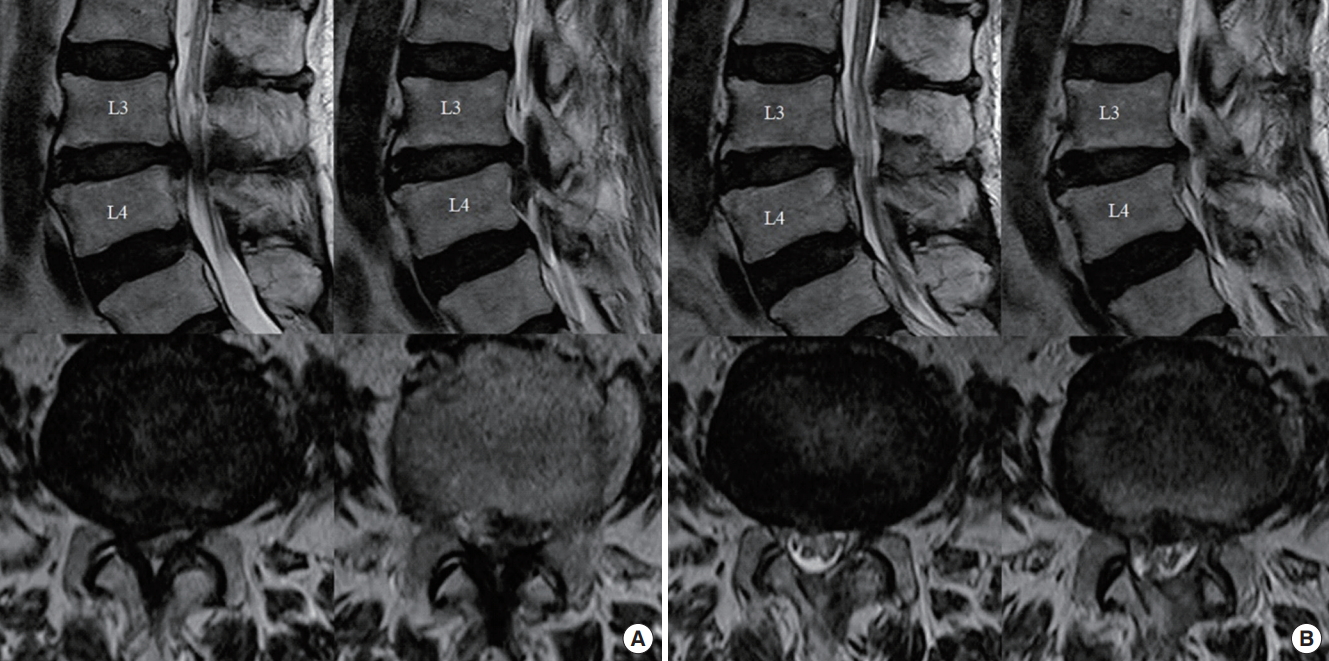
(A) Preoperative magnetic resonance imaging (MRI) of a case with severe lumbar canal stenosis with inferior migration of disc fragment at L3–4 level. (B) Postoperative MRI showing complete removal of inferiorly migrated herniated disc with bilateral decompression without violation of facet joints or muscle damage after percutaneous endoscopic stenosis lumbar decompression.
(A) Preoperative magnetic resonance imaging (MRI) of a case with severe lumbar canal stenosis at L4–5 level. (B) Postoperative MRI showing complete bilateral decompression without violation of facet joints or muscle damage after percutaneous endoscopic stenosis lumbar decompression.
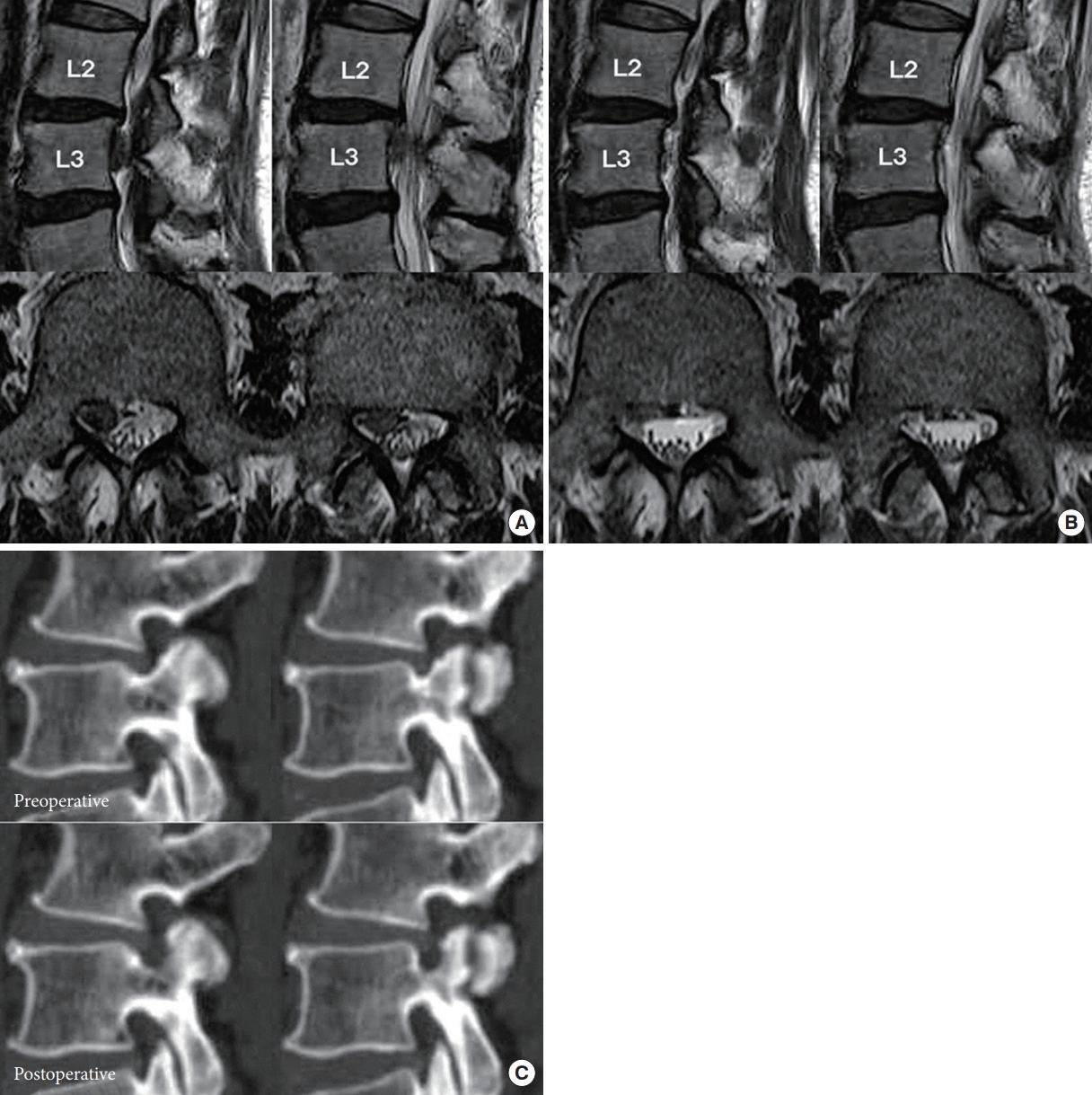
(A) Preoperative magnetic resonance imaging (MRI) showing high-grade inferior migration of disc at L2–3 level. (B) Postoperative MRI showing complete removal of high grade inferiorly migrated herniated disc at L2–3 level. (C) Preoperative and postoperative computed tomography images of suprapedicular circumferential drilling to approach inferior migrated disc fragment.

(A) Preoperative magnetic resonance imaging (MRI) showing inferior migration of disc at L3–4 level and postoperative MRI showing complete removal of inferiorly migrated herniated disc at L3–4 level. (B) Recurrence after 2 years: Preoperative MRI showing inferior migration of disc at L3–4 level and postoperative MRI showing complete removal of inferiorly migrated herniated disc at L3–4 level.
DISCUSSION
The fields of spine surgery have experienced rapid growth over the past decade, yet little research has focused on the issues related to older age. Perioperative complications are frequently encountered in elderly patients owing to comorbid cardiovascular and renal disease, poor nutritional status and immobility. Concerns regarding perioperative complications may be allayed by decreasing the invasiveness with which the spine is approached. Smith and Fessler [10] have mentioned without exaggeration about the paradigm change in spine surgery accompanying the evolution of Minimally Invasive Spine Surgery techniques. Ideal surgical approach to the spine is the one, which causes minimal approach related disruption of normal spinal anatomy and function.
Decision taking for operative intervention in old age spine disease is a formidable task. As the age increases so does the comorbidity [2,3]. Fragility, defined as increasing vulnerability due to stressors in old age, increases exponentially with age [11]. While major complications as wound infection, neurological deficit, renal shutdown, pneumonia and stroke may be seen in one out of five patients in old age, the frequency of minor complications as delirium, urinary tract infections, postoperative dysesthesia may be seen in upto 72% of patients [12,13]. Endoscopic spine surgery has come as a boom to cater the need of this precious patient population. While numerous studies have demonstrated the benefits of endoscopic spine surgery as compared to microlumbar discectomy or open surgery [6-9], we could not find any study notably mentioning the role of endoscopic spine surgery in old age.
The multiple comorbid illnesses of old age, as cardiorespiratory diseases, renal insufficiency, diabetes, and immunocompromised state together make up the administration of general anesthesia an arduous task [14-17]. Moreover the prolonged duration in traditional open spine surgery itself becomes a risk factor for adverse outcome [18]. Blood transfusion is frequently needed in open spine surgery as the patient has a low reserve, and then transfusion has its own complications. While laminectomy alone carries risk of increasing subtle insufficiency [19,20] that already exists, posterior fixation in patients at 70 to 80 years of age is even not well tolerated. Moreover, the degenerative changes exist at more than one level at old age and so arises the need to address the spine disease in a minimally invasive way.
Advantages of full endoscopic spine surgeries are less soft tissue dissection, less blood loss, reduced hospital admission days, early functional recovery and enhancement in the quality of life [21]. With the increase in human longevity, the development of effective treatment for degenerative diseases is inevitable, and future endoscopic spine surgery will play a very important role in maintaining health of this ‘super-aged’ population.
The multiple level affection of disc disease in old age and coexistence of stenosis and disc disease merits special mention. Frequently, both are symptomatic and need intervention. PESS seems to be the treatment of choice in such patients. We managed 5 patients in our study who needed intervention for both, the disc disease and stenosis. As can be seen in the results, the recovery is immediate and long-standing. Our study has shown that multiple options exist in percutaneous endoscopy spine surgery to address different diseases of spine in old age. Different endoscopic routes in our patients effectively managed the wide gamut of disc prolapse as central, paracentral, foraminal and superior and inferior migration. Stenosis in old age causes incapacitation and worsens the quality of life. Excellent postoperative results with long-term follow-up for endoscopic decompression establishes the latter as the need of hour. The improvement in VAS score for leg pain and ODI was phenomenal and was maintained on long-term follow-up. On MacNab criteria, 88.6% of patients had good to excellent outcome. The recurrence rate in our study on 53 patients was 9.4%, this is well within the range of 5%–18% rate of recurrence reported previously. While multiple pathological factors contribute to early and late recurrence in disc disease, little is known about recurrence at this old age. We believe, with ever-improving surgical techniques and availability of modern instruments, the recurrence rates will improve in the coming years.
While the overall number of patients in this study is limited, the authors believe this is a landmark article that knuckles down to unfold the complex panorama of spine disease in age above 70 years. It embarks upon the potential of endoscopic spine surgery to combat disc prolapse and stenosis in old age patients.
CONCLUSION
Providing long-term optimum results in lumbar degenerative spine disease is a daunting task, especially in old age patients beyond 70 years. In spite of the recurrence as most common complication, PESS is pivotal to address old age degenerative spine disease without exposing patient to more extensive open surgery. The authors have shown that optimum results can be achieved in various types of disc prolapse and stenosis with the favorable long-term outcome.
Notes
The authors have nothing to disclose.
Acknowledgements
We would like to acknowledge scientific team members Ms. Jae Eun Park and Mr. Kyeong-rae Kim for providing assistance in acquiring full-text articles and managing digital works.