Comparison of Inpatient and Outpatient Preoperative Factors and Postoperative Outcomes in 2-Level Cervical Disc Arthroplasty
Article information
Abstract
Objective
The purpose of this study was to evaluate factors associated with inpatient admission following 2-level cervical disc arthroplasty (CDA). A secondary aim was to compare outcomes between those treated on an inpatient versus outpatient basis.
Methods
Using data from the American College of Surgeons National Surgical Quality Improvement Program database, multivariate logistic regression analysis was used to assess the independent effect of each variable on inpatient or outpatient selection for surgery. Statistical significance was defined by p-values <0.05. The factors considered were age, sex, body mass index (BMI), smoking status, American Society of Anesthesiologists physical status classification, and comorbidities including hypertension, diabetes, history of dyspnea or chronic obstructive pulmonary disease, previous cardiac intervention or surgery, steroid usage, and history of bleeding. In addition, whether the operation was performed by an orthopedic or neurosurgical specialist was analyzed.
Results
The number of 2-level CDA procedures increased from 6 cases reported in 2014 to 142 in 2016, although a statistically significant increase in the number of outpatient cases performed was not seen (p=0.2). The factors found to be significantly associated with inpatient status following surgery were BMI (p=0.019) and diabetes mellitus requiring insulin (p=0.043). There were no significant differences in complication and readmission rates between the inpatient and outpatient groups.
Conclusion
Patients undergoing inpatient 2-level CDA had significantly higher rates of obesity and diabetes requiring insulin than did patients undergoing the same procedure in the outpatient setting. With no difference in complication or readmission rates, 2-level CDA may be considered safe in the outpatient setting in appropriately selected patients.
INTRODUCTION
The overall rates of cervical spine surgeries in general as well as those performed on an outpatient basis have increased significantly in recent years [1-4]. Despite well documented increases in the rates of medical comorbidities in patients undergoing cervical procedures, there has been a simultaneous decrease in complication rates [1-3], potentially allowing for more of these procedures to be performed in an ambulatory setting. However, given the increases in comorbidities as well as the nature of cervical procedures, routine inpatient admission following surgery is still common.
Cervical disc arthroplasty (CDA) is an operation which has been gaining popularity largely due to widely reported good clinical outcomes and low complication rates. There now exists a strong body of literature, including multiple meta-analyses, which demonstrates both safety and efficacy of the procedure [5-12]. In addition, the preservation of motion provided by arthroplasty has been shown to reduce the incidence of adjacent segment disease [13], increasing its attractiveness as a surgical option in an appropriately selected patient.
With the continued push to decrease costs, the spectrum of procedures performed on an outpatient basis has widened, now often including multilevel cervical fusions and arthroplasties. While the outcomes of 2-level CDA are comparable to single level procedures [14], less is known specifically regarding which factors allow for outpatient 2-level surgery to be performed. The purpose of this study therefore was to evaluate which factors were associated with inpatient admission following 2-level CDA. A secondary aim was to compare outcomes between those patients treated on an inpatient versus outpatient basis.
MATERIALS AND METHODS
1. Electronic Database
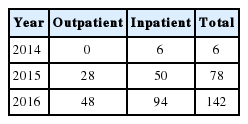
For this study, the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database was queried from 2014 through 2016 (Table 1). The ACS NSQIP database is a prospectively collected database that contains preoperative, intraoperative and 30-day follow-up data on major surgical procedures from several hundred hospitals in the United States. A trained surgical clinical reviewer is responsible for data collection at each site, and patients are followed via mail, telephone calls and medical chart reviews. Data are entered online in a Health Insurance Portability and Accountability Act-compliant, secure, web-based platform that can be accessed 24 hours a day [15]. The NSQIP has been reported to have a high success rate in recording outcomes and an interrater reliability of agreement on reported outcomes of greater than 95% [16]. Because the NSQIP is a national anonymized database, this study was deemed exempt from review by the local Institutional Review Board.
Patients older than 18 years of age who underwent 2-level CDA were included from the database. Patients were selected on the basis of having a current procedural terminology (CPT) code for a single level arthroplasty (22856) as well as the code for an additional disc arthroplasty (22858). It was not deemed necessary to exclude revision surgeries as they are commonly performed on an outpatient basis as well.
2. Extracted Data
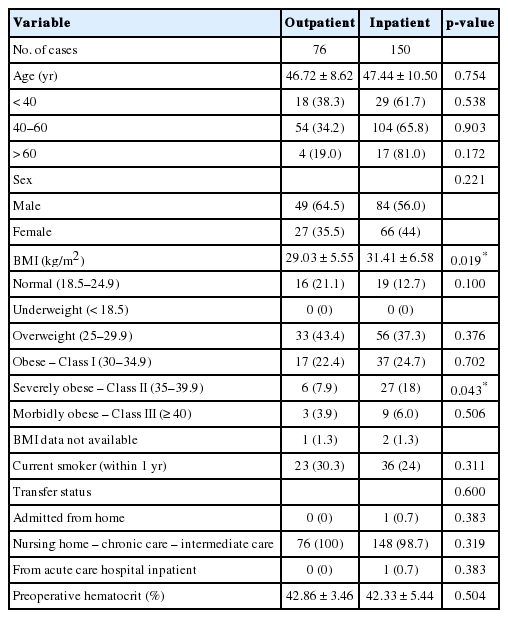
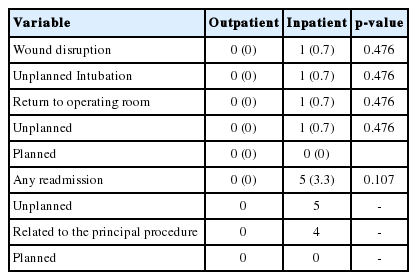
Patient data included inpatient versus outpatient performance of surgery, patient age at the time of surgery, sex, body mass index (BMI), height and weight, smoking status, American Society of Anesthesiologists (ASA) physical status classification, and selected comorbidities including hypertension requiring medication, diabetes, history of dyspnea or chronic obstructive pulmonary disease (COPD), previous cardiac intervention or surgery, steroid usage and history of a bleeding disorder (Tables 2, 3). In addition, whether the surgery was performed by an orthopedic or neurosurgical specialist was analyzed as well. Shortterm outcomes data included readmission, complications which occurred during the initial hospitalization, length of stay (LOS) and discharge disposition (Table 4).
All analyses were performed using the IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA). Comparisons between groups were performed using Student t-tests for continuous variables and chi-square or Fisher exact tests for frequencies. Multivariate logistic regression analysis was used to assess the independent effect of each variable on inpatient or outpatient selection for surgery. Statistical significance was defined with a p-value set at <0.05.
RESULTS
A total of 226 cases, 76 performed on an outpatient basis and 150 performed on an inpatient basis were included in this study. The number of 2-level CDA procedures increased from 6 cases reported in 2014 to 142 in 2016, although a statistically significant increase in the number of outpatient cases performed was not shown (p=0.2).
The 2 factors which were found to be significantly associated with inpatient status following surgery were BMI and diabetes mellitus requiring insulin. Inpatients had a higher BMI (p=0.019) at 31.41±6.58 kg/m2 (range, 19.65–64.17 kg/m2) compared to outpatients at 29.03±5.55 kg/m2 (range, 19.34–46.44 kg/m2). Inpatients were also more likely to obese, at 49.3% vs. 34.7% of outpatients (p=0.037), and more likely to have a history of diabetes requiring treatment with insulin, at a rate of 5.3% compared to 0% for outpatients (p=0.043).
Sex (p=0.221), smoking status, (p=0.311), hypertension (p=0.356), history of COPD (p=0.623), reported dyspnea (p=0.223), steroid use (p=0.223), disseminated cancer (p=0.476), history of a bleeding disorder (p=0.223) and preoperative hematocrit (p=0.504) were not associated with either inpatient or outpatient treatment. Differences based on age were not found to be statistically different, and while patients 60 or older were less likely to be treated as outpatients (19% vs. 33.6%, overall), this value did not reach significance (p=0.172). Likewise, patients under 40 were not more likely to be treated as outpatients (p=0.538).
ASA physical status classification (p=0.699) and wound classification (p=0.159) were not significantly different between the inpatient and outpatient groups.
One hundred fifty-four (68 % of the reported cases) were performed by a neurosurgeon, with 70.1% of those being inpatient, and 72 (32% of the reported cases) were performed by orthopedic surgeons, with 58.3% of those being inpatient. However, whether the surgery was performed by a neurosurgeon or orthopedic surgeon did not affect performance of surgery on an inpatient or outpatient basis (p=0.80).
The total operative time (in minutes) was statistically significant between the 2 groups (p=0.017), with the outpatient group having a mean operative time of 131.34±43.56 minutes (range, 56–252 minutes) and the inpatient group, 147.65±56.41 minutes (range, 49–314 minutes).
The postoperative LOS for the outpatient group was 0.84±0.49 days (range, 0–2 days), while that for the inpatient group was 1.41±0.83 days (range, 0–4 days) (p<0.0001).
There were no significant differences in complication (Table 5) and readmission rates (between the inpatient and outpatient groups, with there being 1 wound disruption (p=0.476), 1 unplanned intubation (p=0.476), 1 unplanned return to the operating room (p=0.476), and 5 unplanned readmissions (p=0.107) in the inpatient group and none in the outpatient group (Tables 6, 7).
No patients had superficial surgical site infection (SSI), deep SSI, organ space SSI, pneumonia, pulmonary embolism, failure to wean off the ventilator for >48 hours, progressive renal insufficiency, acute renal failure, urinary tract infection, cerebrovascular accident/stroke with neurological deficit, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, bleeding requiring transfusion, deep vein thrombosis/thrombophlebitis, sepsis or septic shock.
DISCUSSION
In this study it was determined that BMI, specifically BMI which is at or above the obese level and diabetes mellitus requiring treatment with insulin were preoperative variables which were significantly associated with inpatient 2-level CDA. While it was not possible to determine whether these were planned inpatient stays or if they were unanticipated admissions following scheduled outpatient surgery, the findings do highlight certain factors which are important to consider in the preoperative setting. Given the potential for postoperative complications including airway compromise from postoperative hematoma or soft tissue swelling, patient safety is of primary concern. While we cannot conclude that obesity or diabetes are directly related to patient safety, it remains important to identify all factors which may affect ability to perform surgeries safely in the outpatient setting. Likewise, while other factors such as age, BMI, presence of bleeding disorders or ASA physical status classification are frequently involved in preoperative planning, they may not significantly impact whether or not 2-level surgery may be performed in the outpatient setting.
In addition, the absence of a significant difference in shortterm complications and readmissions between the inpatient and outpatient groups shows that multilevel cervical disc replacement performed on an outpatient basis is indeed safe.
The ability to provide safe and effective outpatient surgery is of particular importance, as there are significant reductions in cost when patients are able to be discharged home the same day. In a study from 2010, Wohns [17] found that the cost of an inpatient 1-level CDA was nearly 6 times higher than the same procedure performed in the outpatient setting, without a difference in complication rates. Similarly, multiple studies of both CDA and anterior cervical discectomy and fusion (ACDF) indicate that single and multilevel procedures can be safely performed in the outpatient setting without increases in complications [10,18-21]. Granted the 2 procedures are different, the patient populations and many technical aspects of the operations are similar, with reasonable conclusions to be drawn from both.
Specifically regarding CDA, it is likely that its widespread popularity will continue to grow, furthering the importance of being able to safely perform the procedure in the outpatient setting. For many years, ACDF has been the mainstay of treatment for symptomatic cervical disease, however more recently studies have demonstrated superior outcomes for CDA. There have been may published studies, including multiple meta-analyses of direct comparisons between the 2 procedures that have shown that CDA appears to result in better function, lower reoperation rates, lower complication rates, better improvements in neurological success, greater motion preservation, lower rates of adjacent segment disease, shorter lengths of stay, and without differences in health state utility values [5-9,11-13,22-24]. In light of these findings, it is clear that CDA will remain a common and prevalent procedure, further highlighting the substantial reductions in costs able to be achieved with a better understanding of how to plan for outpatient surgery.
This study is not without limitations. First, the nature of retrospectively reviewed database studies does not allow for the elimination of bias. The lack of randomization of patients itself creates bias, as does the variability of many factors involving the settings in which the surgeries took place. In addition, it is not possible to account for surgeon experience and preference during planning of the surgeries or for hospital or surgery center policies. Similarly, differences in preoperative diagnoses can account for differences between groups. Since in this study patients were selected on the basis of CPT code, it is unclear whether certain preoperative diagnoses would have affected one or more outcomes or the inpatient versus outpatient nature of the procedure. Likewise, it is beyond the scope of the study to determine whether patients were selected for outpatient operations based on certain diagnoses but rather than to report on which diagnoses were associated with either inpatient or outpatient performance of surgery. Finally, there was some overlap between the lengths of stay in both groups, indicating that not all patients with planned outpatient procedures were discharged on the day of surgery, however it was not possible to determine specific causes of inpatient admission in these individual cases. Despite these limitations though, the large number of variables reported by the NSQIP database and its high reporting accuracy allow for a wide variety of patient and operative factors to be studied for a given procedure oftentimes identifying previously unknown findings.
CONCLUSION
There was no difference in the complications rates between the 2 groups, thus showing that outpatient multilevel CDA is as safe as and more cost-effective than an inpatient procedure, therefore, it may be possible to more effectively plan for outpatient surgery and improve cost effectiveness. Larger prospective studies are warranted to better delineate which factors would allow for outpatient performance of surgery, and which factors may necessitate inpatient admission.
Notes
Dr. Sheeraz Qureshi is currently receiving Consulting Fees from Zimmer-Biomet, Stryker Spine, Globus Medical, Inc.; Shareholder Interest in Avaz Surgical, Vital 5; Royalties from RTI, Zimmer-Biomet, Stryker Spine. Dr. Todd Albert is currently receiving Grant/Research Support from PCORI, ISSG, NIH; Royalties from Zimmer Biomet, DePuy Synthes, Nuvasive, JP Medical Publishers, Saunders/Mosby-Elseveir, Thieme; Consulting Fees from Facet Link, DePuy, Biomet, Nuvasive, Gentis (Medical Advisory Board); Stock/Investment Interests from Vital 5, Bonovo Orthopedics Inc., Biomerix, InVivo Therapeutics, Spinicity, Crosstrees Medical, Paradigm Spine LLC, Invuity, Gentis, ASIP, PMIG, Pioneer. The other authors have indicated they have no financial relationships relevant to this article to disclose.