Comparative Study on the Period of Absolute Bed Rest of Vertebral Compression Fracture
Article information
Abstract
Objective
As a conservative treatment of compression fractures, absolute bed rest (ABR) for a certain period has been recommended, but no guideline on the period has yet been established. Considering that a long ABR period may adversely affect patients, the difference in prognosis according to the ABR period was investigated in this study.
Methods
A prospective study was conducted who were diagnosed with compression fracture. Groups A and B were put on ABR (one week for group A and two weeks for group B). X-ray images at baseline, 1, 2, 4, and 8 weeks were obtained from both groups, for assessment purposes.
Results
The compression rates of both groups were no significant difference at baseline, 1, 2, 4, and 8 weeks. The conditions of 25.9% and 21.2% of the subjects deteriorated in groups A and B, showing no significant difference. Between the groups of age and bone mineral densities (BMD), no significant difference was observed in the incidence of deterioration. In terms of complications development including constipation and other Gastrointestinal problems, voiding difficulty, etc., group A reported 57.4%, and group B, 84.8%, showing a significant difference (p-value=0.001).
Conclusion
No significant difference in the conservative period was observed between the groups. Group B, however, reported a higher complications development rate than group A. Therefore, a short ABR period may be helpful in the early stage of conservative treatment.
INTRODUCTION
Compression fractures are usually caused by osteoporosis, severe trauma, infection, and neoplasm1,10,16,19). They often lead to back pain and spine deformities such as kyphosis, kyphoscoliosis and loss of vertebral height, which cause deteriorations in the management of daily life activities and in quality of life1,4,7,11,12,18). For the conservative treatment of compression fracture, short bed rests and the use of orthoses have been suggested6,9,17,18,23). Though absolute bed rest (ABR) has been recommended and implemented, no guidelines on its optimal period has been suggested8,13,17,18). The complications of ABR have been reported to include muscle weakness, systemic inflammation, atelectasis, metabolic change, microvascular dysfunction, thromboembolic disease, joint contracture, and skin ulcer3,5,21,23). Considering that bed rest may cause inconvenience and various complications, differences in the prognosis according to the ABR period were investigated in this study.
MATERIALS AND METHODS
Materials
A prospective study was conducted that targeted 232 patients who were hospitalized in the Department of Neurosurgery and who were diagnosed with compression fracture from January 2010 to September 2012. Group A was put on ABR for one week, and Group B, for two weeks. Among the patients in the two groups, those whose follow-up were interrupted, whose fractures were caused by tumors, and who underwent early-stage surgical treatments were excluded from this study. The total of 120 patients who were finally selected for this study, 54 Group A patients were put on one-week ABR, and 66 Group B patients, on two-week ABR.
Methods
The groups were compared according to their ABR periods, which were one week for Group A and two weeks for Group B. The two groups were selected randomly. In each group, the subjects' ages, gender, lengths of hospital day, bone mineral density (BMD) and fracture level, visual analog scale (VAS) scores and compression rate in each ABR period were investigated. The compression rate was calculated as follows: 100-[b/(a+c/2)]×100, wherein "a" and "c" represent the normal vertebral bodies that were one level higher and lower than the compression-fractured vertebral body, respectively, and "b" represents the height of the compression-fractured vertebral body24). The courses of the groups were monitored at the baseline, and after one, two, four and eight weeks through X-ray images to assess the development of complications during the ABR period. The compression fracture was deemed to have deteriorated if the compression rate increased by at least 10%. The deteriorations in the compression fractures of each group during each ABR period were compared according to gender, age, and BMD. The rates of development of complications in the ABR period groups were also compared. The ABR-caused complications included constipation, nausea and voiding difficulty, and they arose only after the compression fracture occurred.
Statistical analysis was performed using SPSS statistic software ver. 19.0.0 (SPSS Inc, Chicago, IL). Chi-square test, Fisher's exact test, Independent Samples T-test were used. A P-value of less than 0.05 was considered statistically significant.
RESULTS
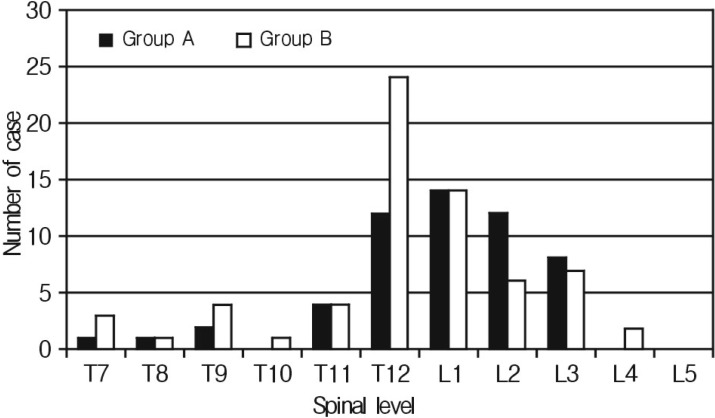
Group A had a mean age of 69.7±12.9 years, a mean BMD of -3.5±1.3, 15 male and 39 female patients, and a mean length of hospital day of 14.2±7.3 day, On the other hand Group B had a mean age of 66.1±14.4 years, a mean BMD of -3.5±1.3, 18 male and 48 female patients, and a mean length of hospital day of 25.9±9.5 days (Table 1). The most common vertebral bodies with compression fracture were from T12 to L2 in both groups (Fig. 1). The compression rate of Group A at the baseline, and one, two, four, and eight weeks was 21.1±10.7, 22.3±10.1, 22.7±10.9, 27.0±11.1, and 28.6±9.4, respectively, and those of Group B was 21.9±13.6, 23.4±13.1, 23.9±13.3, 27.8±14.2, and 29.3±15.2 (Table 2). In both Groups A and B, 14 subjects reported deterioration (25.9% and 21.2%, respectively) (p-value=0.544). In Group A, eight subjects underwent median branch block due to persistent pain; as did 13 subjects in Group B, which figures show a significant difference between the groups (p-value=0.484). The blocking was performed 11.5±4.5 days after the admission in Group A and 16.3±11.0 days after the admission in Group B (p-value=0.171). Thirty-one complications developed in Group A and 56 - much more-in Group B (p-value=0.001) (Table 3). The VAS score of Group A at the baseline and after one, two, four and eight weeks was 6.3±0.9, 2.6±1.0, 2.3±0.8, 2.1±0.9 and 2.2±1.4, respectively, and of Group B, 6.3±1.3, 2.7±0.8, 2.3±0.8, 2.2±0.9 and 2.3±1.1 (Table 4).
Three male subjects reported deteriorations in Group A and the same number in Group B (p-value=1.0), and 11 females each in Groups A and B (p-value=0.602).
Among the subjects aged 75 years or older, 10 in Group A and slightly fewer, seven, in Group B had deteriorated conditions (p-value=0.216); and among the subjects aged less than 75 years, four in Group A and seven in Group B (p-value = 0.752). No significant differences in the ages and the ABR periods of the two groups were observed. Three subjects reported -3.0 or higher BMD deterioration in Group A, and two in Group B (p-value=0.656). In Group A, 11 subjects reported deteriorations with -3.1 or less BMD; and in Group B, 12 subjects (p-value=0.762). The difference between the groups in the rates of their compression fracture deterioration according to their ABR period and BMD was not statistically significant (Table 5).
A total of 87 subjects reported the development of complications: 31 in Group A and 56 in Group B. Thus, there were more complications in the longer ABR group (p-value=0.001). The most common complication was gastrointestinal (GI) problems such as constipation, heartburn and nausea, followed by voiding difficulty (Table 6).
DISCUSSION
Percutaneous vertebroplasty and balloon kyphoplasty have been studied as surgical treatments for compression fractures2,14,15). However, many compression fracture patients with mild kyphosis still choose conservative treatments due to such treatments' favorable results and for economical or psychological reasons20). Nevertheless, no clear protocol for conservative treatments for compression fractures with acute pain has been established yet17,18).
The treatment goals for compression fracture include pain relief, vertebral stability, rehabilitation and osteoporosis improvement17,26). The acute pain that accompanies compression fracture is relieved over a 6- to 12-week period25,27). During this period, bed rest and the use of analgesics and orthoses are suggested as a conservative treatments6,9,17,18,23). In particular, bed rest can reduce the risk of bone resorption and secondary fracture25). It has been widely advised, but there are still no guidelines on its optimal period8,13,17,18). In previous studies, long- or short-term bed rest periods have been cited, without a specific suggestion on the period6,9,17,18,23). Three-day bed rest was done in a study28), and another study did not recommend bed rest as a conservative treatment2). In yet another study, longer bed rest was recommended in the cases with severe pain requiring gradual mobilization17), and for older patients26). Eventually, however, these studies did not clearly suggest a bed rest period. To examine the appropriate periods of bed rest that are expressed as short-term and long-term in the previously mentioned researches, in this study, the group of patients who were put on one-week ABR was compared with the group of patients who were put on two-week ABR.
In the study conducted by Peter Vorlat et al.28) on the recovery predictor after the conservative treatment of compression fracture, all the patients were recommended to go on bed rest for a maximum of three days. The researchers investigated the correlations between different factors, such as the age, gender, BMI, social status, educational attainment, occupation, smoking, insurance, underlying diseases, back pain, association with injuries, fracture type, disc damage level, and sagittal index of injuries, and the prognosis of conservative treatments. Among these factors, smoking and insurance were said to have affected the prognosis, but the influence of the bed rest period on the results was not stated. The mean VAS score in such study were 1.2 (SD 2) before the injury, 7.1 (SD 2.5) a day after the injury, and 3.8 (SD 3) 12 months after the injury. The chronic pain that lasted beyond 12 months was believed to have been caused by the short and insufficient ABR. In comparison, the bed rest periods in this study were one and two weeks, and their effects on the pain relief, length of hospital day, and development of complications were compared. With sufficient bed rest, the mean VAS scores in Group A improved from 6.3±0.9 at the baseline to 2.2±1.4 eight weeks after the injury; and in Group B, they similarly improved from 6.3±1.3 (p-value=0.986) to 2.3±1.1 (p-value=0.553).
In terms of the compression rate of the groups, no statistically significant difference was observed in the X-ray images at the baseline and after one, two, four and eight weeks. In both groups, there were more female patients than male patients, as in most relevant studies13,14,21,27). The most common vertebral bodies where compression fractures developed were from T12 to L2 in both groups (Fig. 1). The difference in the numbers of T12 and L2 in the two groups might have been due to the patient group classification error. Other studies reported results similar to those of this study2,13,21,27), because the thoracolumbar segment is the site between the stiff thoracic vertebral column and the comparatively flexible lumbar vertebral body1).
During the hospital stay, block was conducted for eight subjects (14%) in Group A and 13 subjects (19.7%) in Group B due to persistent pain (p-value=0.484). The mean lengths of time before the block implementation were 11.5±4.5 days in Group A and almost the same, 16.3±11.0 days, in Group B (p-value=0.171). In the study on gray ramus communicans nerve block in compression fracture patients conducted by Tae et al.25), 30 (88.2%) of the 34 patients experienced continuous relief. Although the GRC blocking significantly relieved the pain felt by the compression fracture patients, it did not reinforce the strength of the fractured vertebral body. Nevertheless, the procedure was effective for the control of the persistent pain that could remain after early bed rest, and was helpful for the early ambulation of the patients.
For the complications of bed rest, muscle weakness, systemic inflammation, atelectasis, metabolic change, microvascular dysfunction, thromboembolic diseases, joint contracture, and skin ulcer were described3,5,21,23). To treat these complications, physiotherapy, passive stretching, neuromuscular electrical stimulation (NMES) and early ambulation were recommended3). In particular, severe hyperkyphosis in compression fracture reduces the space between the rib and the iliac crest, induces flank pain and compresses respiration22). Early rehabilitation can correct kyphosis to reduce the pain and to improve the patient's mobility and quality of life17,18). In addition, rehabilitation can prevent additional injuries, reinforce the axial muscle strength of the spine and help re-align the spine17,18).
In this study, no serious complications were observed during the short one- and two-week bed rest periods. The most common complications in Group A included GI problems such as constipation and diarrhea, followed by voiding difficulty and dizziness; and in Group B, constipation, followed by other GI problems, cough and voiding difficulty. Moreover, the incidences of constipation (p-value=0.005), GI problems (p-value=0.003) and cough (p-value=0.008) significantly increased with a longer bed rest. Most of the complications were controlled with medications, and most of the symptoms disappeared through ambulation and rehabilitation.
However, in this study, the groups of patients were divided randomly, so the comparison of the two groups according to the degree of their compression fracture was insufficient. When treating patients, it is unreasonable to apply one-week ABR unconditionally and uniformly to the group of patients with a serious compression rate, and more detailed studies on this are needed.
CONCLUSION
In this study, no statistically significant difference in the incidence of clinical deterioration was observed between the one- and two-week absolute best rest (ABR) groups. No significant differences were observed either in the results of the bed rest periods in terms of age and bone density. By contrast, the incidences of complications and discomfort increased in the longer-ABR-period group. In conclusion, the short term bed rest period is recommended in compression fracture patients to reduce the treatment period and inconvenience of the patients.