Understanding the normal craniovertebral junction (CVJ) alignment and segmental motion in human is paramount to better understand CVJ deformity and to decide on a more appropriate surgical strategy according to the pathologies of CVJ.
During fetal development, the spine assumes the shape of the letter “C,” with the curved side facing toward the back, while the open side faces the front of the fetus. This C-shaped curve is the primary curve of the spine and is well-suited to the cramped confines of the womb. Newborn infants retain this primary curve and, with growth and maturity, develop secondary curves, first in the neck and later in the lower back. Of the 2 secondary spinal curves, the cervical curve in the neck region develops first. This curve develops in the opposite direction from the primary spinal curvature and allows the infant to have visual access to his surroundings [1,2]. This secondary cervical curvature is also found in quadrupedal animals as well as in humans. However, there is a significant difference between humans and animals with respect to this curvature: the upper cervical alignment compared to the cranium. It is because the location of the human foramen magnum is quite different from any other kind of animals.
In humans, the foramen magnum is anteriorly positioned and is inferiorly oriented (opening directly downward). Contrastingly, in apes, the foramen magnum is more posteriorly positioned, the foramen magnum in apes is more vertically oriented (opening backwards and downwards, rather than directly downwards) [3-5].
Positional difference of the foramen magnum causes a difference of CVJ alignment between humans and other quadrupeds with respect to the C0–1 segment.
When humans are at rest in standing position, the C0–1 articulation is held rather flexibly, whereas the C1–2 joints are held slightly in an extended position. This is because the human cervical spine is located inferior to the foramen magnum, and these characteristics ensure an energy-saving balance of the head and neck when at rest, allowing humans to maintain horizontal vision effectively without significant effort of the neck extensor muscle. However, quadrupeds with posteriorly positioned foramina magna require well-developed nuchal musculature and ligaments to bear the weight of the head to maintain horizontal gaze. Therefore, the demands on the neck musculature differ between humans and quadrupedal mammals (Fig. 1).
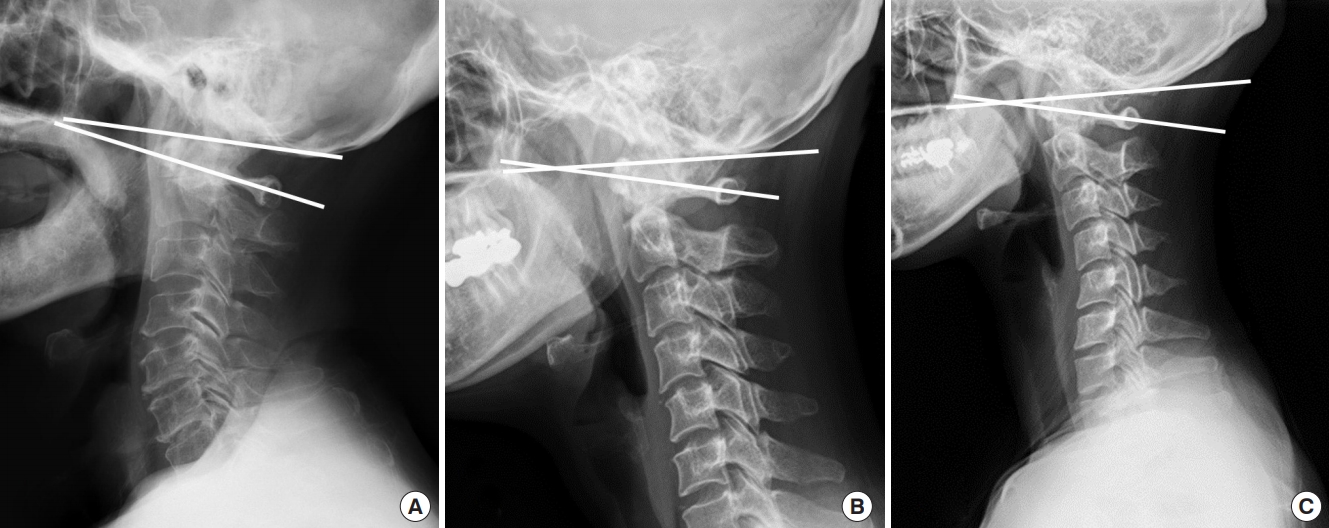
Radiographically, the C1 slope is backwardly slanted and kyphotic angulation of the C0–1 segment allows some degree of freedom for neck extension as the space between the occiput and C1 posterior arch allows for upper cervical extension (Fig. 2).
Although asymptomatic population may have different types of cervical alignment, such as “straight” or “kyphotic” cervical spines ranging from 7% to 40% (Fig. 2), it has been well accepted that a large percentage (about 75%–80%) of cervical lordosis is localized to the C1–2 segment, only a small percentage (15%) of cervical lordosis exists in the lower cervical levels and the C0-1 segment is kyphotic [6,7].
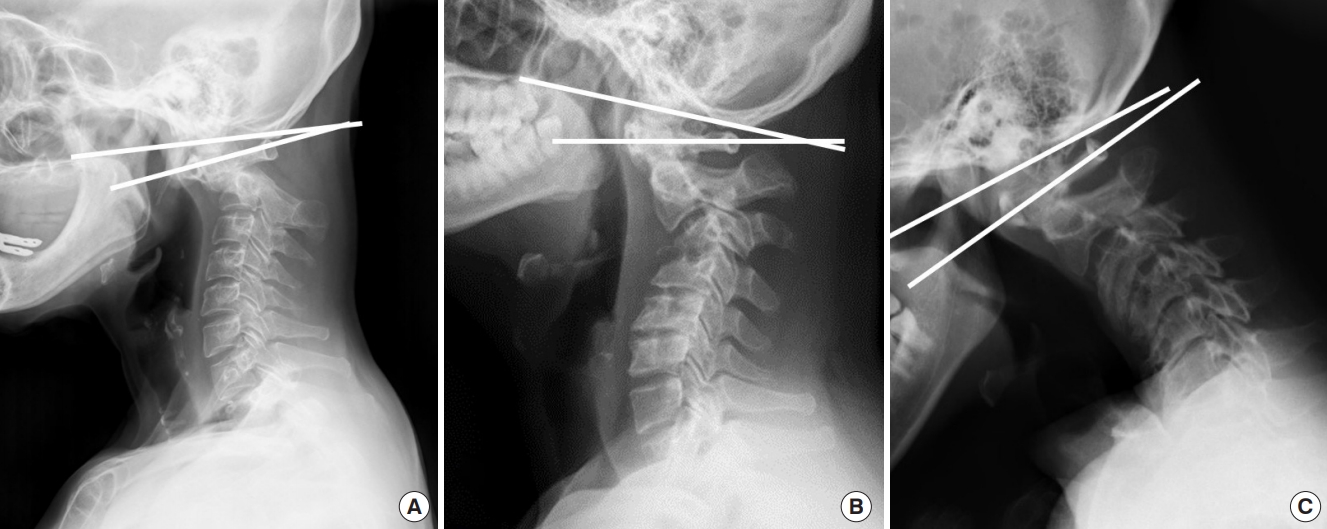
When patients have kyphotic deformity in the cervical spine or thoracolumbar spine, C0–1 segment can hold up the head to compensate for distal kyphosis, maintaining the sagittal balance and horizontal gaze (Fig. 3). Therefore, a normal kyphotic angulation of C0–1 segment could be referred to as a “tertiary curvature” to characterize human CVJ alignment, to differentiate between upper cervical spine alignment and primary/secondary curvature of the human spine as well as differentiate between the cervical spine curvature of humans and that of quadrupeds including apes.
The loss of subaxial lordosis has been reported in CVJ fixation in which excessive hyperlordosis is created at the C0–2 segment. Moreover, craniometrics studies revealed that an excessive CVJ kyphosis can cause subaxial compensatory lordosis [8,9].
The anatomy of the cervicothoracic junction (CTJ) has been shown to be as the main determining factor for cervical lordosis [10]. However, the angle of CVJ has also been shown to significantly be related to the angle of subaxial cervical spine [11]. These findings suggest that reciprocal interaction may likely affect not only global balance, but also regional balance.
Another interesting finding is that neck flexion and extension movement are initiated primarily by motions between the head and C1 [12,13]. As the head approaches full flexion and extension, contributions from the upper cervical segments decreases, whereas contribution from the lower cervical segments increases [14].
In addition, our previous studies showed that C0–1 segment is dominant segment for compensatory motion to prevent postoperative dysphagia caused by upper cervical fixation and the C0–1 segmental motion with or without occipital fixation is associated with subaxial kyphotic change after upper cervical fixation [15-17].
So, it is important not to include occipital fixation as much as possible not only to preserve C0–1 segmental motion to prevent postoperative dysphagia but also to avoid abnormal kyphotic alignment of the subaxial cervical spine after surgery.
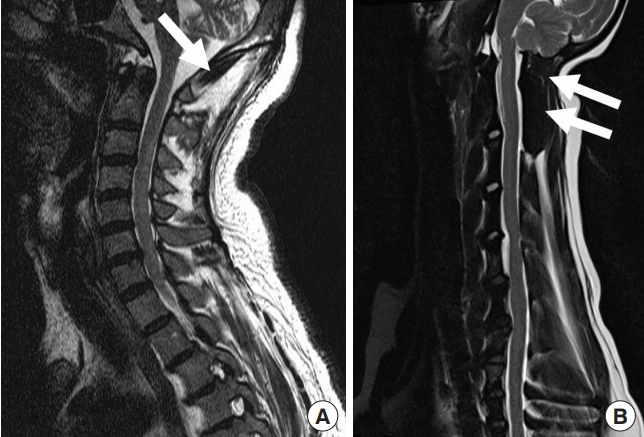
CVJ malalignment is a rare and challenging pathology that can result in progressive deformity, myelopathy, severe neck pain, and functional disability, such as difficulty swallowing. The most common causes of CVJ deformity include rheumatoid arthritis, trauma, neoplasm, infection, and congenital bony malformation. This deformity may alter the quality of life because of the neck pain, disabling headache, dysphagia, and myelopathy.
Surgical management of CVJ pathology could be complex for various reasons; given the sensitive relationships involved in the surrounding neurovascular structures and intricate biomechanical issues, access to this region is relatively difficult and there are many risks involved [16,18-23].
Recently, there have been tremendous advances in CVJ surgery. However, understanding normal alignment, segmental motion, compensatory reaction and anatomical variation around CVJ is critical not only to decide optimal surgical option but also to prevent complications and improve surgical outcomes.