Cervical Spine Deformity Correction Techniques
Article information
Abstract
Cervical kyphotic deformity can be a debilitating condition with symptoms ranging from mechanical neck pain, radiculopathy, and myelopathy to impaired swallowing and horizontal gaze. Surgical correction of cervical kyphosis has the potential to halt progression of neurological and clinical deterioration and even restore function. There are various operative approaches and deformity correction techniques. Choosing the optimal strategy is predicated on a fundamental understanding of spine biomechanics. Preoperative characterization of cervical malalignment, assessment of deformity rigidity, and defining postoperative clinical and radiographic objectives are paramount to formulating a surgical plan that balances clinical benefit with morbidity. This review of cervical deformity treatment provides an overview of the biomechanics of cervical kyphosis, radiographic classification, algorithm-based management, surgical techniques, and current surgical outcome studies.
INTRODUCTION
The cervical spine functions to bear the axial load of the head, optimize forward gaze in an erect posture, maintain physiologic head and neck movement, and to support and protect vital neurovascular structures. Appropriate cervical spinal alignment is critical to these functions as they relate to nearly all aspects of activities of daily living. Conversely, cervical spinal deformity, most commonly kyphosis, can have a profoundly negative impact on an individual’s quality of life [1,2]. Cervical kyphosis can occur secondary to various underlying etiologies including: advanced degenerative disease, iatrogenic, trauma, neoplasm, infection, and systemic arthritides (e.g., rheumatoid arthritis, ankylosing spondylitis) [3,4]. The presentation of symptomatic cervical kyphosis typically includes neck pain; however, severe deformity resulting in spinal cord or nerve compression can lead to myelopathy and/or radiculopathy. With progressive cervical malalignment, additional impairments can occur including problems with horizontal gaze, cough, swallowing and respiration.
Mild cervical deformity in individuals with minimal or no neurologic compromise can often be managed conservatively. Severe deformity and those with significant neurologic deficits, ultimately, can only be corrected with surgical intervention. The goals of surgery in cervical deformity include neurologic decompression, restoration of alignment, stabilization and arthrodesis, and complication avoidance. This review discusses the biomechanical principles of cervical deformity, preoperative clinical and radiographic assessment, algorithms for operative decision-making, and current evidence regarding surgical outcomes.
CERVICAL SPINE BIOMECHANICS
The cervical spine is composed of 7 vertebrae that function to provide motion in 6 planes: flexion/extension, axial rotation, and lateral bending. Biomechanical studies determine that the cervical spine is capable of nearly 90° of flexion and lateral rotation, 70° of extension, and 20°–45° of lateral bending [5]. The overall sagittal alignment of the native cervical spine is that of lordosis. Cervical lordosis is secondary to the relative increased disc height anteriorly versus posteriorly. The coronal orientation of the subaxial cervical facet joints allows for greater sagittal plane motion, resistance against translation, and maintenance of forward gaze and head position with erect posture. Loss of cervical lordosis (i.e., kyphosis) most commonly occurs with progressive deterioration of anterior disc height (e.g., degenerative, iatrogenic) over multiple segments, but can also result from ventral wedge compression of the vertebrae (e.g., trauma, pathologic fracture). An impaired posterior tension band (e.g., postlaminectomy, facet compromise) contributes to further kyphosis due to inability to resist forward tilting and/or translation of the cervical spine.
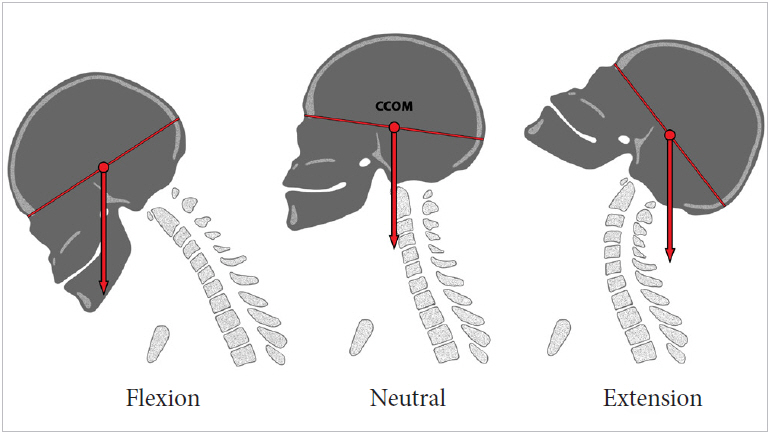
The cranial center of mass (CCOM) has been identified as the midpoint of the nasion-inion line from cadaver studies by Vital and Senegas [6]. This point is superior and anterior to the cervical vertebral column resulting in anterior axial loading. The posterior tension band ligaments and paraspinal muscles balance this force, yielding the lordotic curvature seen in a properly aligned cervical spine. The subaxial facet joints bear about 66% of the loading weight with the remaining 33% from the intervertebral disks of the anterior compartment [7]. In the presence of cervical kyphosis, the CCOM moves further anteriorly, increasing the bending moment, and requiring greater counterbalance from the posterior elements within the neck (Fig. 1). This is analogous to the instantaneous axis of rotation (IAR). In lordosis, the IAR is situated posteriorly in the vertebral body, thereby facilitating the posterior tension band to maintain appropriate alignment. Alternatively, in kyphosis, the IAR can move anterior to the vertebral column (typically at the level of the apex of the curve), which puts the posterior tension band at a relative biomechanical disadvantage for maintaining sagittal alignment. Over time with muscle fatigue, ligamentous loading laxity, and glacial disk degeneration, the CCOM/IAR can continue to shift anteriorly, compounding the degree of deformity.
CERVICAL RADIOGRAPHIC ASSESSMENT
There are multiple methods for characterizing the radiographic alignment of the cervical spine. Historically, the Toyama method is a simple description of overall alignment as lordotic, straight, sigmoid or kyphotic. On lateral X-ray, a straight line is drawn from the midpoint of C2 to C7. The number of intervening vertebrae that lie anterior versus posterior to this line, and their relative distance from the line is measured. The modified Cobb method is the angle subtended by lines perpendicular to the C2 and C7 inferior endplates, with a positive angle indicating lordosis.
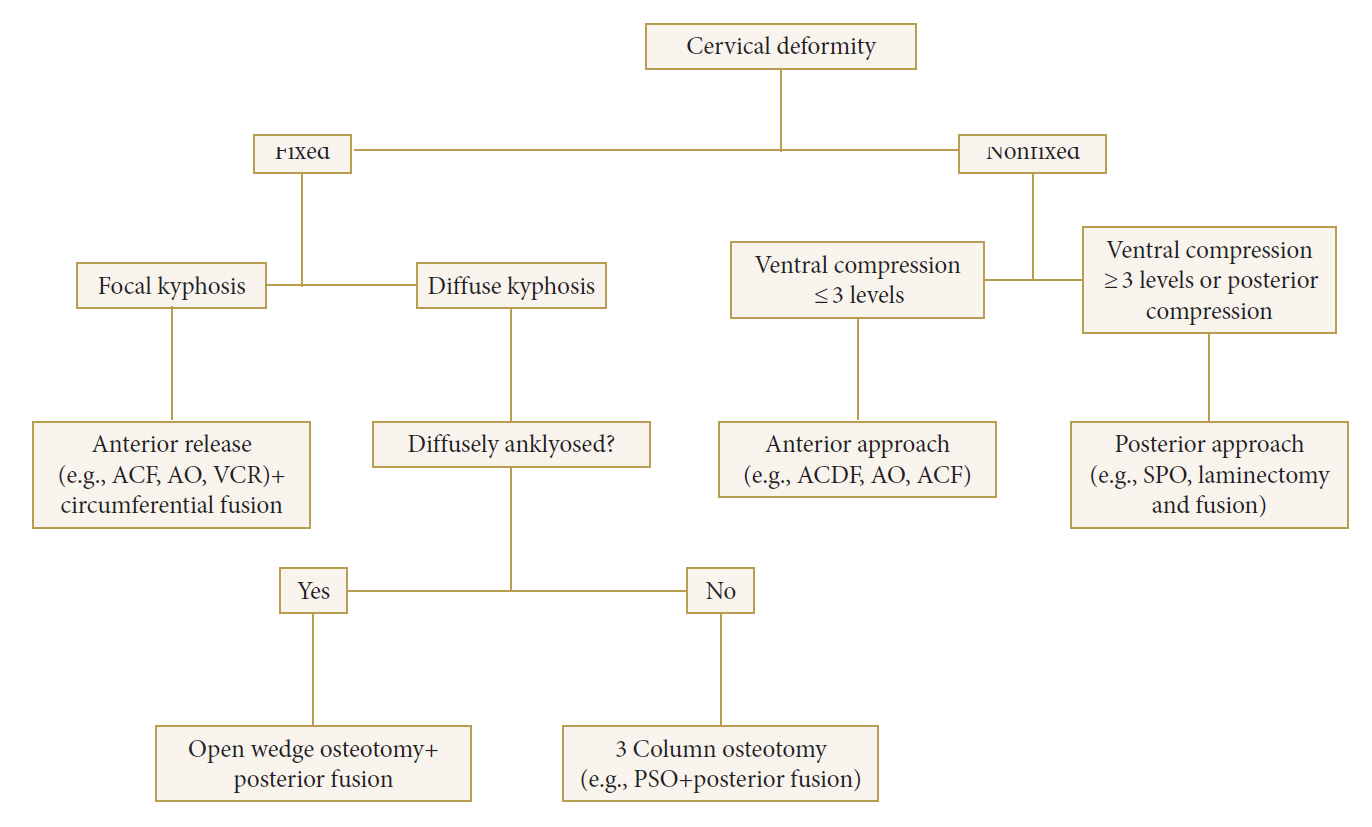
More recently, several radiographic parameters have been developed to better characterize cervical alignment, sagittal balance, and relative position of the head-cervical-upper thoracic axis. The C2–7 sagittal vertical axis (SVA) describes general cervical sagittal balance. C2–7 SVA is measured by the distance between a C2 vertical plumb line (midvertebral body) and a horizontally oriented line from the posterior superior C7 endplate (Fig. 2). Positive cervical sagittal imbalance with a C2–7 SVA >40 mm correlates with increased disability [2]. Worsening disability with increased C2–7 SVA may be related to the increased moment arm of the cervical spine leading to greater strain on the posterior cervical musculature and consequent impaired posture, functional range of motion, and pain [2].
Artist rendering demonstrating radiographic parameters used to define cervical sagittal alignment parameters. Cervical sagittal vertical alignment demonstrated as the distance between the C7 postero-superior endplate and a plumb line from the C2 centroid. T1 slope denoted as the angle between the extension of the T1 superior endplate and the horizontal reference line through the midpoint of the T1 superior endplate. Thoracic inlet angle represented as the angle between the extension of the T1 superior endplate line connected to the sternum and a reference line orthogonal to the midpoint of the T1 superior endplate. Neck tilt denoted as the angle between the line parallel to the T1 superior endplate and the vertical reference line.
Chin-brow vertical angle (CBVA) is a measure of horizontal gaze, defined as the angle subtended by a line from an individual’s chin-to-brow and the vertical axis (Fig. 3). This value is typically measured either from clinical photograph or long cassette radiographs including the skull, with the patient extending their hips and knees while the neck remains in a neutral upright position [8]. Lafage et al. [9] in a retrospective radiographic series of 303 patients showed a CBVA ranging from -4.7° to 17.7° corresponded to worse function on Oswestry Disability Index.

Chin-brow vertical angle denoted as the angle subtended between the vertical axis and a line connecting the chin-to-brow.
Spino-pelvic parameters such as pelvic incidence, sacral slope and pelvic tilt have been effective in characterizing thoracolumbar sagittal balance. Corollary parameters in the cervical spine have been introduced with the thoracic inlet angle (TIA), T1 slope (T1S), and neck tilt as measures of cervical sagittal balance (Fig. 2) [10]. TIA is the angle formed by a line from the sternum to the midpoint of the T1 upper endplate and a line perpendicular to that endplate. The T1S is the angle subtended by the T1 superior endplate and a horizontal line crossing the T1 superior endplate midpoint. Neck tilt is calculated by the angle formed between a line connecting the T1 superior endplate midpoint to the sternum and the vertical axis.
These measurements have been incorporated in a recently described cervical deformity classification system [11]. The classification system includes a deformity curve descriptor plus 5 modifiers. The deformity curve descriptor is determined by the location of the curve apex: C (cervical in sagittal plane), CT (cervicothoracic junction in sagittal plane), T (thoracic in sagittal plane), S (primary coronal curve), and CVJ (deformity located at craniovertebral junction). The 5 modifiers include the C2–7 SVA, CBVA, T1S – cervical lordosis (analogous to pelvic incidence - lumbar lordosis), myelopathy modifier, and SRS-Schwab classification for thoracolumbar deformity. Normal values for the above modifiers are T1S – cervical lordosis <15°, C2–7 SVA <40 mm, CBVA between -10° and +20°.
This classification system requires full-length standing postero-anterior (PA) and lateral spine radiographs that include the cervical spine and femoral heads, standing PA and lateral cervical spine radiographs, modified Japanese Orthopedic Association score questionnaire, and a clinical photograph or radiograph that includes the skull for measurement of CBVA. Both intra- and interobserver reliability were reasonably established for the system and each modifier was selected by its correlation with measure of health-related quality of life (HRQoL) [12-16].
ALGORITHM FOR SELECTION OF SURGICAL APPROACH
Cervical deformity correction requires meticulous preoperative planning with careful attention to biomechanical principles, pathologic processes contributing to kyphosis, and individual patient factors that may impact surgical effectiveness versus morbidity. Comprehensive preoperative imaging including dynamic flexion-extension X-ray, magnetic resonance imaging (MRI), and computed tomography should be obtained to assess curve location, severity, and overall rigidity, as well as, need for neural decompression and accessibility for spinal stabilization. The decision with regards to anterior, posterior, or combined approach, number of instrumented levels, and the osteotomy type and location is informed by both imaging characteristics and patient clinical and neurologic status. Ultimately, judicious patient selection and communicating appropriate expectations for postoperative outcome are paramount for effective patient-physician shared decision-making.
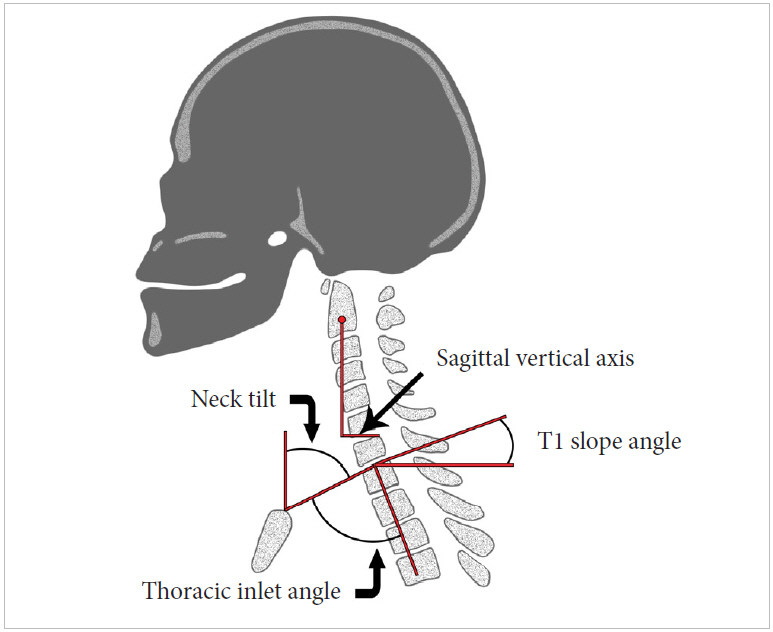
Steinmetz et al. [4] in 2007 proposed an algorithm for cervical deformity correction based primarily on overall spinal rigidity. The first step is to define the deformity as either “fixed” or “flexible” based on flexion-extension X-rays and/or responsiveness to cervical traction. A “flexible” deformity is recommended for posterior correction and fusion alone. Alternatively, a “rigid” deformity is then assessed for presence of facet ankylosis. A rigid deformity with facet ankylosis, regardless of anterior or posterior cord compression, requires a combined anterior and posterior release of the intervertebral disc(s) and ankylosed facets (respectively) for correction with subsequent stabilization and fusion. If facet ankylosis is not present, an anterior only approach for correction, decompression as needed, and stabilization can be performed. This algorithm provides a straightforward method for determining the optimal strategy for correction of regional cervical alignment (i.e., kyphosis). The algorithm, however, does not account for positive cervical sagittal imbalance (i.e., positive C2–7 SVA) particularly in the setting of upper thoracic hyper-kyphosis (i.e., increased T1S). Surgical decisionmaking for these complex cervicothoracic deformities may require more extensive osteotomy techniques and involvement of the upper thoracic levels. Fig. 4 represents the algorithm used by the senior author.
SURGICAL TECHNIQUES FOR CERVICAL DEFORMITY CORRECTION
Techniques for cervical deformity correction include traditional procedures such as anterior cervical discectomy and fusion (ACDF), anterior corpectomy, and posterior laminectomy and fusion, as well as, more advanced Smith-Petersen/Ponte, opening wedge, and cervical pedicle subtraction osteotomies. These various techniques can be utilized solely or often in combination depending on the location and severity of the deformity, and to address neural compression and need for spinal fixation.
1. Anterior Cervical Discectomy and Fusion
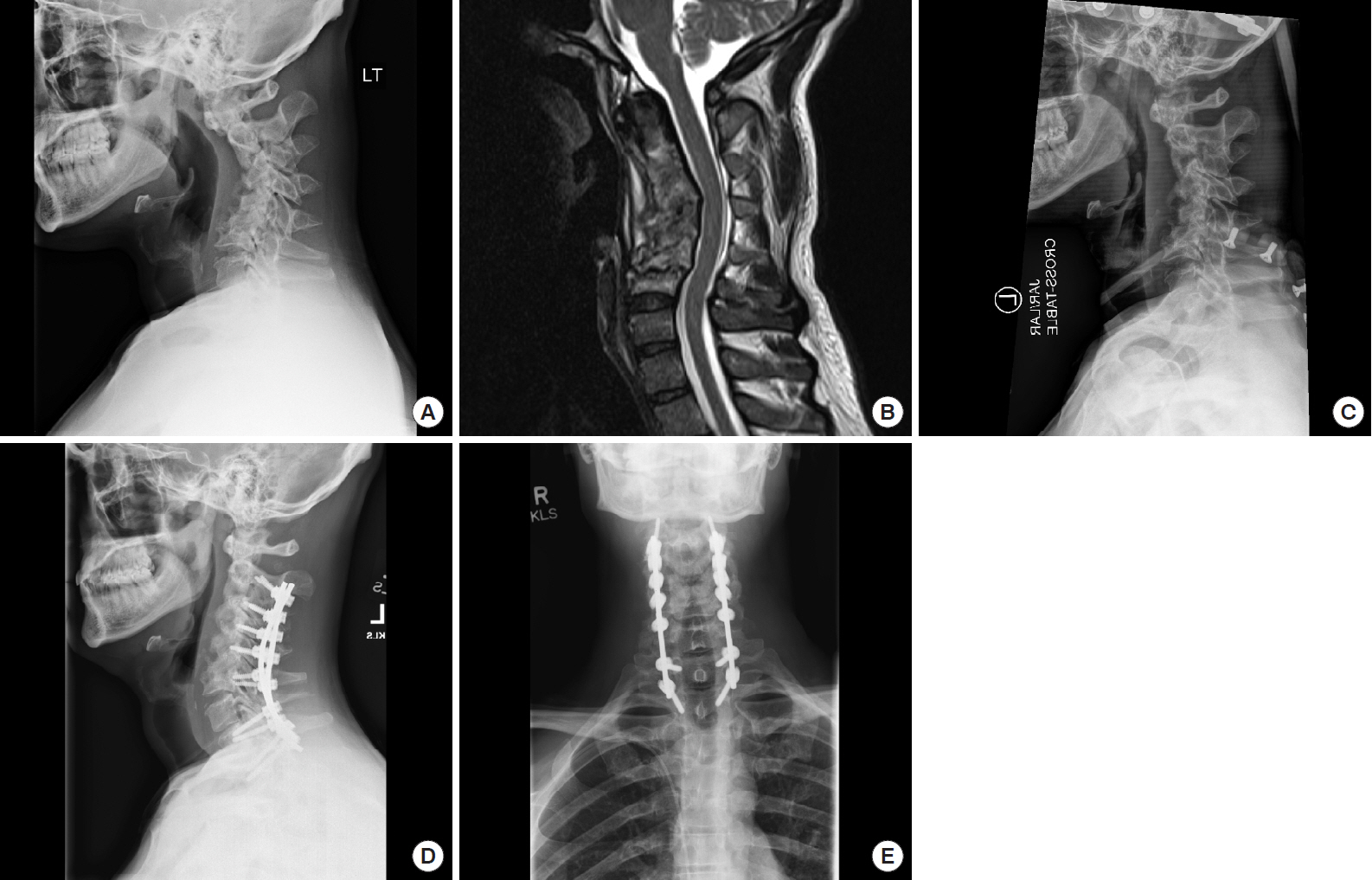
ACDF is a common neurosurgical procedure performed for routine degenerative conditions. Familiarity with this approach among surgeons makes it a relatively facile and effective strategy for correction of sagittal malalignment, particularly when incorporating multiple levels across the apex of a kyphosis (Fig. 5). Employment of this technique for deformity correction, however, requires mobility through the disc space and facet joint. It is not appropriate, therefore, in the setting of ankylosis or after prior surgical fusion.

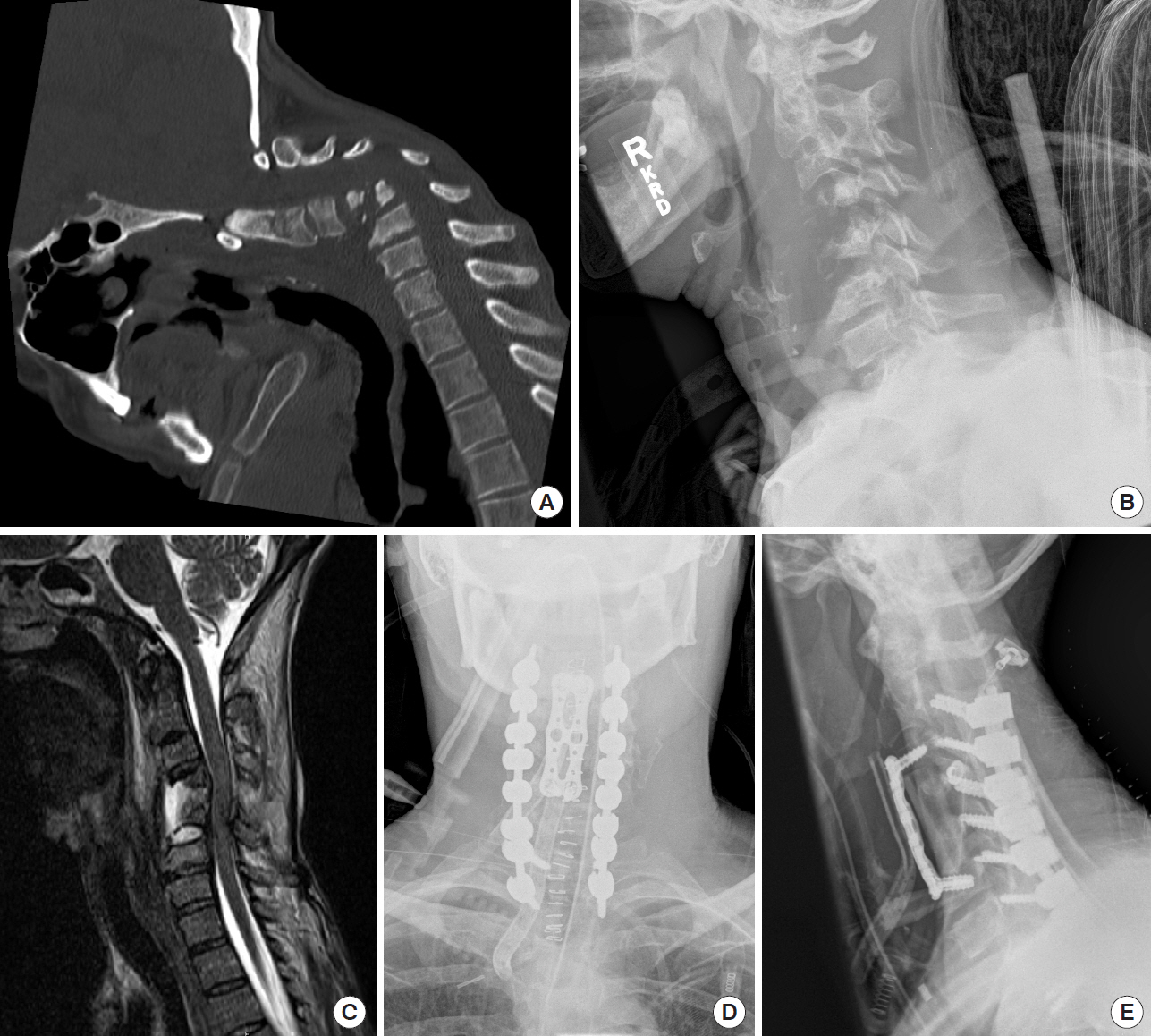
A 63-year-old male who presented with progressive cervical myelopathy and acute-on-chronic quadriparesis. (A, B) Preoperative lateral X-ray and computed tomography scan demonstrating severe cervical kyphosis. (C) Preoperative sagittal magnetic resonance imaging demonstrating spinal cord compression and T2 signal abnormality within the cord. The patient underwent multilevel anterior cervical discectomy and fusion from C2 to C7 to correct the kyphotic deformity, as well as, C2-T1 posterolateral instrumented fusion and decompression. (D, E) Postoperative anteroposterior and lateral radiographs demonstrating deformity correction.
Generally, targeted levels are those that demonstrate significant ventral neural compression and/or those at the apex of the kyphosis. Initial steps include optimal supine positioning with a shoulder bump to allow for the head and neck to gently rest in extension. After anterior surgical exposure, placement of vertebral body pin distractors (e.g., Caspar pins) in a divergent trajectory allows for segmental lordosis. Distraction after complete discectomy, osteophytectomy, and release of the posterior longitudinal ligament optimally creates lordosis, as the distractor is positioned anterior to the IAR. Special care should be made to avoid over distraction which may put the neural elements on stretch, or risk failure of the distraction pins in patients with poor bone density. Moreover, focal hyper-extension may cause buckling of the ligamentum flavum posteriorly resulting in canal stenosis, as the interlaminar distance is shortened. Careful study of preoperative imaging to assess for extent of ligamentum flavum hypertrophy is critical to minimize risk of this complication. Additionally, lateral bridging osteophytes or incompletely resected or ossified posterior longitudinal ligament may resist distraction across the disc space.
Placement of lordotic shaped intervertebral grafts can further enhance appropriate sagittal contour, specifically with increased anterior graft height. Positioning of these grafts to avoid subsidence is critical for maintaining lordotic correction. Anterior plate fixation across multiple levels allows for further restoration of lordosis. In a kyphotic or sigmoid cervical alignment, the intervening vertebral bodies can be “pulled towards” a lordotic anterior plate using a lag screw technique [17]. This strategy, however, depends on adequate bone density to prevent screw pull out failure. It also should be noted that while this approach may improve the overall cervical lordotic contour, it is less effective at improving the tilt of the upper-instrumented vertebra.
2. Anterior Cervical Corpectomy and Fusion
Anterior cervical corpectomy and fusion (ACCF) can be applied to treat a fixed kyphotic deformity or a focal angular kyphosis secondary to a wedge vertebral body (e.g., pathologic fracture) as demonstrated in Fig. 6. The surgical exposure is similar to ACDF. Instead of achieving multisegmental correction through the disc spaces, the ACCF technique relies on distraction of the terminal vertebra across the corpectomy defect either through a strut graft or expandable cage. Subsequent anterior plating secures the overall construct [18-20]. The lack of intervening points of fixation compromises the biomechanical advantage for deformity correction, as well as, does not allow for using a lag screw technique to conform the spine to a lordotic plate. Further, special attention should be made to the overall tilt of the rostal vertebra. Placement of an expandable cage in the setting of uncorrected positive sagittal imbalance and a forward tilted rostral vertebra can position the distraction forces posterior to the IAR, and inadvertently distract the spine into further kyphosis.
A 50-year-old female with chin-on-chest deformity and complete collapse of the C4 and C5 vertebral bodies secondary to osteomyelitis. The patient had significant upper extremity weakness and profound weight loss due to severe dysphagia. (A) Preoperative sagittal computed tomography demonstrating severe kyphotic deformity centered at C4–5. The deformity was nonrigid and the patient was placed in halo traction for gradual reduction (B). (C) Post traction, preoperative magnetic resonance imaging demonstrating cervical stenosis and destruction of the C4 and C5 vertebral bodies. The patient underwent 2 level (C4–5) anterior corpectomy and fusion supplemented with C2-T2 posterior instrumented fusion (D, E).
Corpectomies that span 3 or more levels are associated with high instrumentation failure rates, particularly without supplemental posterior fixation [21,22]. Osteoporosis can increase failure rates even in the setting of 1–2 level corpectomy [23,24]. Sparing of an intermediate vertebral body by performing an ACCF coupled with an adjacent ACDF (i.e., “hybrid construct”) provides an additional intervening fixation point, which may decrease risk of pseudarthrosis and instrumentation failure [25].
3. Anterior Osteotomy
Anterior osteotomy (ATO) is an extended ACDF approach that involves resection of the uncovertebral joint in addition to complete discectomy. This technique is a more invasive and destabilizing osteotomy as it completely releases any anterior tension band that may limit distraction and widening of the anterior disc space [26,27]. After exposure of the kyphosis apex, blunt dissection to the lateral uncinate is performed. The costal process (anterior ring of the transverse foramen) is a landmark for lateral dissection. Using the blunt dissector to shield the vertebral artery laterally, a high-speed drill can be used to thin the uncinate process from medial to lateral, with final shelling of the remaining cortical rim with a microcurrette.
Lordotic correction with ATO occurs as a result of several maneuvers. First, divergent Caspar pins are placed above and below the disk space and expanded after the osteotomy to generate lordosis. Second, with the patient positioned with a shoulder bump and a headrest, the headrest is carefully removed with the head supported. Controlled downward pressure on the forehead allowing the head to rest in maximal extension enhances correction. A large lordotic shaped graft is then placed in the disk space. If the surgical plan includes subsequent posterior correction and fixation, an anterior buttress plate should be placed to prevent graft extrusion.
4. Posterior Instrumentation and Fusion
Flexible kyphotic deformity may be corrected via a conventional posterior approach with instrumented fusion (Fig. 7). Like ACDF, this surgical technique is commonly performed for routine degenerative conditions and allows for efficient decompression of multiple levels when indicated. This approach is appropriate for cervical kyphosis in the setting of relatively well-preserved disc height and mobility, as may be seen in patients with a compromised posterior tension band (e.g., postlaminectomy kyphosis) or underlying neuromuscular disease [28,29]. Proper positioning is the critical step in correction of alignment. Once intubated, the patient is positioned prone with a skull clamp. The head and neck are extended in a military tuck position with the skull clamp secured to the operating room table. Performing this maneuver in an anesthetized patient with spinal cord compression and myelopathy may require intraoperative neuro-monitoring to prevent neurologic injury. Once adequate cervical alignment is confirmed with intraoperative fluoroscopy and gross visualization, the cervical spine can be surgically stabilized with multilevel posterior fixation to maintain correction. Additional lordosis creation can be achieved by compression across the posterior instrumentation, however, this is often modest due to the limited pullout strength of cervical lateral mass screws [4]. Particular attention should be made when performing a complete facetectomy prior to compression across posterior cervical instrumentation to ensure that no residual articulating process (superior or inferior) impinges on the exiting nerve root in the foramen.
A 33-year-old male after motor vehicle accident several months prior presented with worsening neck pain and bilateral arm paresthesias with imaging findings of cervical kyphosis. Panel A demonstrates lateral upright cervical X-ray with midcervical kyphotic deformity. (B) Sagittal T2 magnetic resonance imaging demonstrating erosive changes throughout the midcervical spine and loss of disc height resulting in cervical kyphosis. (C) Deformity was reduced with cervical traction and patient was secured preoperatively with a halo vest. (D, E) Postoperative anteroposterior and lateral upright cervical X-rays after C2-T2 posterior cervicothoracic instrumentation and fusion demonstrating restoration of cervical lordosis.
5. Smith-Petersen Osteotomy
Smith-Petersen Osteotomy (SPO), also known as Ponte osteotomy, is an extended posterior approach that involves complete bilateral resection of the inferior and superior articulating processes at a motion segment. This “pedicle-to-pedicle” posterior bony release allows for added compression across posterior screw fixation for segmental lordosis. This technique relies on a mobile disc with relatively preserved disc height. Greater global cervical lordosis may be achieved by performing SPOs at multiple levels (Fig. 8). After the SPOs have been performed and posterior screws have been placed, the skull clamp may be released from the operating table and the patient’s head and neck manually extended in a controlled fashion. Once the optimal alignment has been achieved, the skull clamp is reconnected to the operating room table. The rods are contoured according to the corrected alignment and inserted into the screws for definitive stabilization.
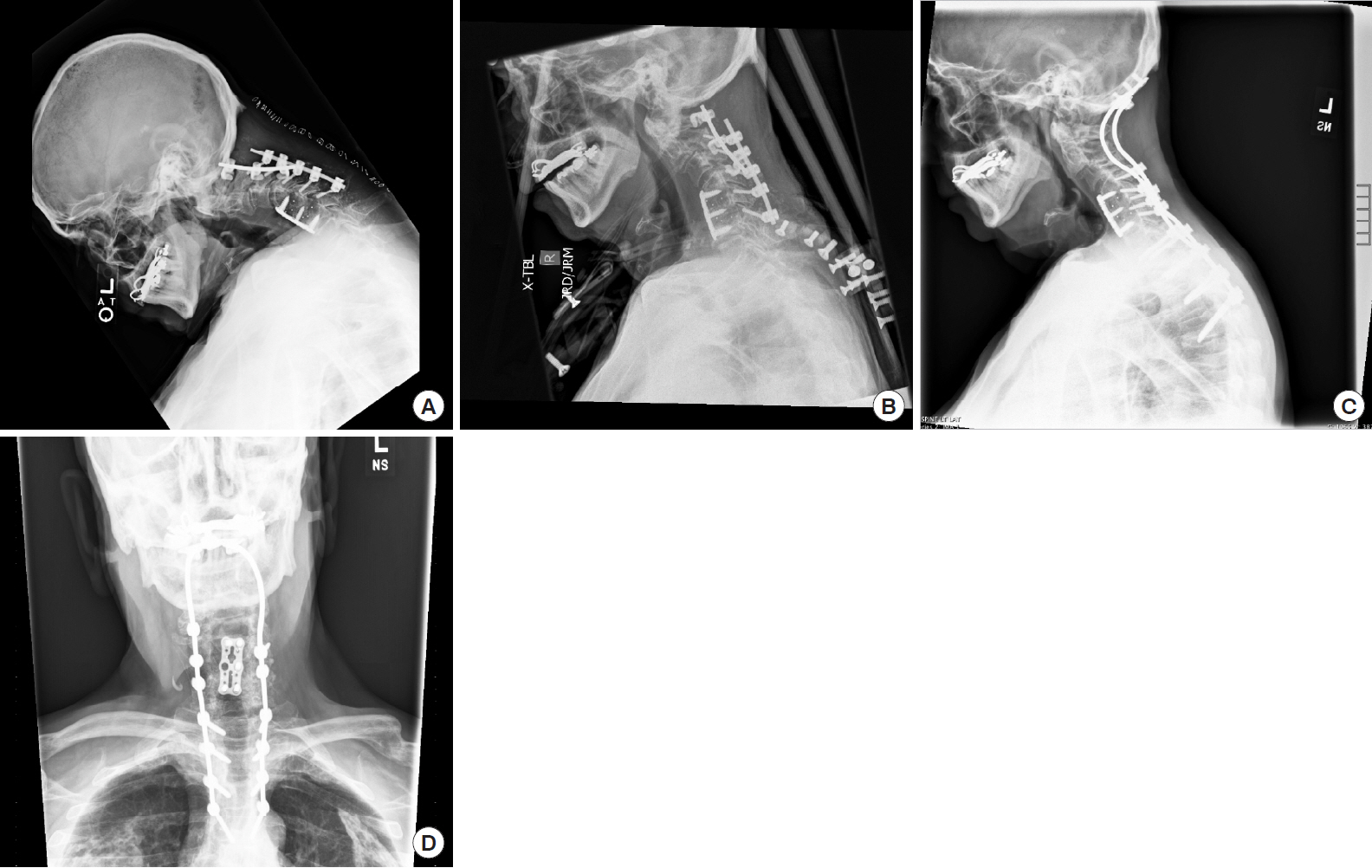
A 73-year old male with Parkinson disease and remote history of anterior cervical discectomy and fusion (ACDF) who underwent recent posterior cervical spine surgery at another facility. He presented with new postoperative worsening kyphosis and chin-on-chest deformity. (A) Lateral upright cervical spine X-ray demonstrating prior ACDF and recent posterior cervical instrumentation with failure of lateral mass screw and sublaminar hook and rod construct. (B) He was placed in cervical traction and secured with a halo vest, with incomplete reduction of his kyphosis. (C, D) Postoperative upright cervical anteroposterior/lateral X-rays after undergoing removal of previous posterior cervical hardware, Ponte osteotomies at C2/3, C3/4, C5/6, C6/7, and C7/T1, and occipital-thoracic posterior instrumentation and fusion.
6. Opening Wedge Osteotomy
The opening wedge osteotomy is a cervical deformity correction technique specifically for patients with diffuse cervical ankylosis (Fig. 9). This technique was originally described to correct chin-on-chest deformity in patients with ankylosing spondylitis. The opening wedge osteotomy is a posterior surgical approach typically performed at C7, as the vertebral artery is generally not confined within the transverse foramen at this level. For a C7 opening wedge osteotomy, a complete laminectomy is performed at C6, C7, and T1 [30]. The C7 facet complex and pedicles are resected, as well as, the inferior articulating process of C6 and superior articulating process of T1. In a controlled maneuver, the head and neck is then maximally extended creating an osteoclastic opening wedge fracture through the anterior vertebral column. Intraoperative neuro-monitoring is performed before, during and after correction to assess for any neurologic change. Additionally, the spinal cord dura is closely inspected during the corrective maneuver to assess for any undue buckling or compression along the laminar edge. The corrected alignment is then secured with posterior spinal fixation across multiple levels rostral and caudal to the osteotomy.

A 66-year-old male with history of ankylosing spondylitis. (A-C) He suffered minor trauma and subsequently developed chin-on-chest deformity secondary to fracture of the C7 vertebral body as demonstrated on preoperative sagittal computed tomography (CT), lateral radiograph, and magnetic resonance imaging. In the setting of diffuse ankylosis, he underwent a posterior opening wedge osteotomy at C6 with posterior fixation of C2 to T3. Panel D demonstrates immediate postoperative X-ray with corrected sagittal alignment and posterior instrumented stabilization. (E) Midsagittal CT demonstrating deformity correction at the C6 vertebral body with anterior osteoclastic opening wedge osteotomy.
This approach achieves an aggressive correction and is typically reserved for severe chin-on-chest deformity. Diffuse cervical ankylosis with a longer lever arm is necessary to transmit sufficient force to create the osteoclastic opening wedge fracture. Underlying osteopenia or osteoporosis often seen in ankylosing spondylitis further enhances the surgical maneuver. Due to the iatrogenic 3-column destabilization, various techniques have been described to prevent catastrophic intraoperative injury. Hinged rods can be affixed to the posterior screws with the hinge temporarily in the released position [31]. When the opening wedge is performed, the hinged rod allows for sagittal realignment while preventing translational displacement. After the head and neck are repositioned in corrected alignment, the hinge is secured and the end caps are definitively tightened.
7. Cervical Pedicle Subtraction Osteotomy
Pedicle subtraction osteotomy (PSO) is a three-column corrective technique that is primarily used in the setting of a circumferential fixed deformity (e.g., prior surgical fusion; Fig. 10) [32]. PSO is typically performed at C7 or T1 due to the relatively wider spinal canal, the vertebral artery is often anterior to the C7 transverse process, preservation of hand function in the event of a C8 root injury, and the greater correction of head position with a more caudal level osteotomy [33,34].
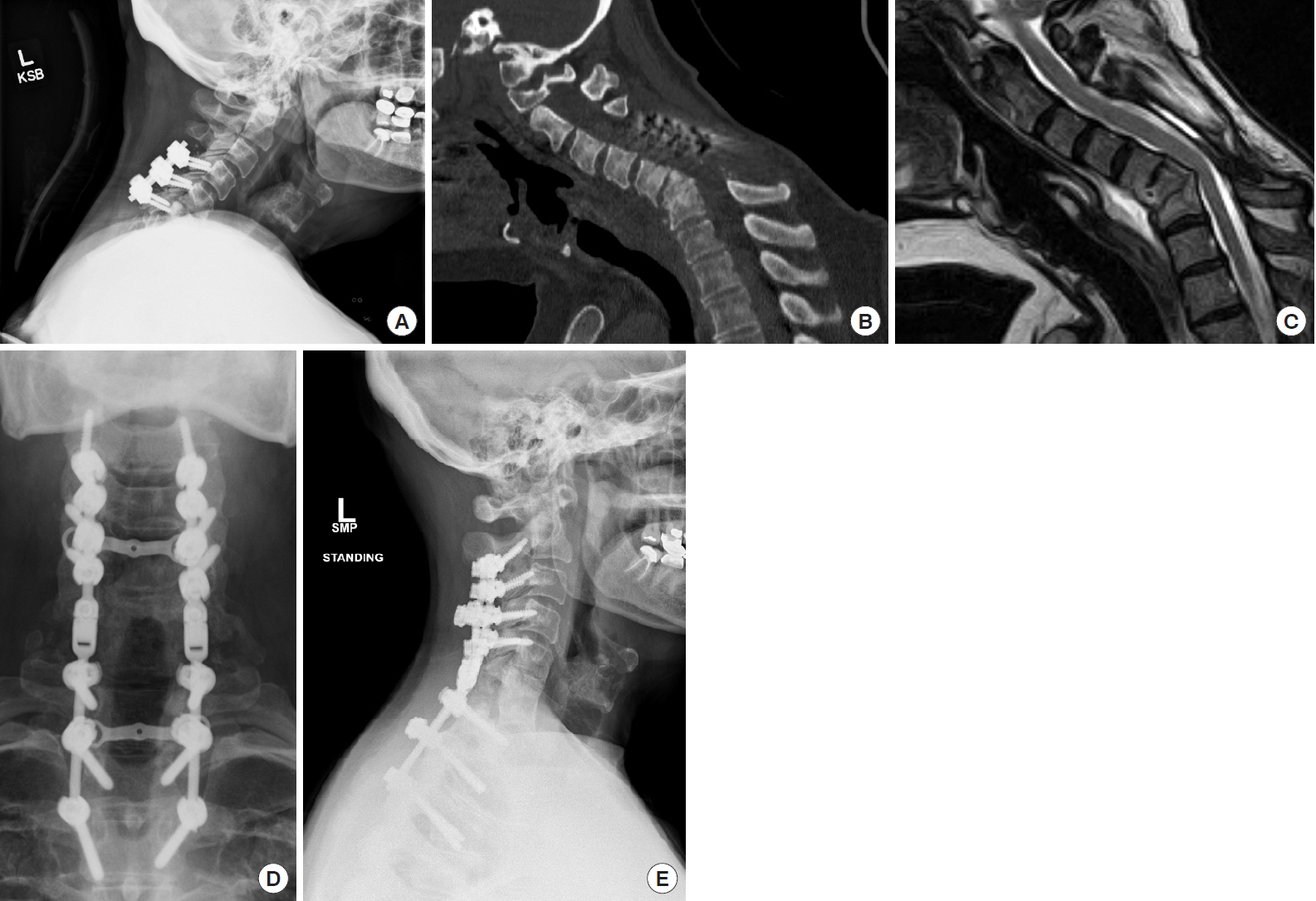
A 59-year-old female who underwent posterior decompression and fusion from C4 to C6 for spinal epidural abscess and osteomyelitis at another facility. (A) She subsequently presented with cervicothoracic junction kyphosis with chin-on-chest deformity. (B, C) Preoperative sagittal computed tomography and magnetic resonance imaging demonstrating a fixed deformity, positive sagittal imbalance, and spinal cord compression secondary to ventral spinal cord compression. The patient underwent a posterior approach for C7 pedicle subtraction osteotomy with posterior segmental instrumentation from C2 to T3. (D, E) Postoperative anteroposterior and lateral radiographs demonstrating posterior instrumented fusion and sagittal deformity correction.
The surgical exposure is similar to the opening wedge osteotomy with laminectomies extending one level above to one level below the PSO. Facetectomies are performed at the levels above and below with complete pedicle resection at the PSO level. Complete removal of the pedicle is critical to allow adequate space for 2 nerve roots to exit between the rostral and caudal pedicles after osteotomy closure. Partial resection of the vertebral body is performed in a posterior wedge manner using a drill or rongeurs through the bony window created by the resected pedicle. A temporary holding rod is useful on the opposite side while performing the osteotomy to prevent inadvertent translational injury. Once the posterior wedge osteotomy is completed, it is sequentially closed by gentle extension of the neck in the skull clamp. After resecuring the head clamp, lateral radiographs are performed to confirm alignment and the spinal cord dura is inspected for buckling or compression along the laminar edge. Additional lordosis can be gained with gentle compression across the screws above and below the osteotomy. Rods are contoured and placed for definitive stabilization.
8. Vertebral Column Resection
Vertebral column resection (VCR) requires a combined anterior and posterior approach for complete removal of 1 or more vertebral bodies, adjacent discs, and posterior elements (lamina, facet complex, pedicles). Subsequent anterior and posterior reconstruction is necessary. VCR completely disconnects and destabilizes the segment(s), and therefore has potential for significant multi-planar deformity correction. The inherent complexity of this approach with respect to associated neurovascular structures and associated morbidity, however, has resulted in limited reports of this technique.
In 2013, a nomenclature for 7 anatomical osteotomy grades was developed to standardize language across deformity spine surgeons [35]. These osteotomy grades, in order of increasing invasiveness, are:
• Grade 1 – partial facet joint resection or anterior discectomy
• Grade 2 – Smith-Petersen/Ponte
• Grade 3 – partial or complete corpectomy
• Grade 4 – anterior osteotomy, uncovertebral joint resection to transverse foramen
• Grade 5 – opening wedge osteotomy
• Grade 6 – cervical pedicle subtraction osteotomy
• Grade 7 – vertebral column resection
CLINICAL OUTCOMES
Postoperative restoration of sagittal alignment and balance appears to correlate with functional outcome. Roguski et al. [14] in 2014 prospectively followed 49 patients undergoing either posterior or anterior surgery for cervical spondylotic myelopathy to assess the effect of postoperative sagittal imbalance as a predictor of HRQoL. Overall, they found that patients undergoing anterior surgery had greater improvement in 36-Item Short Form Health Survey questionnaire Physical Component Summary (SF-36 PCS), Oswestry Neck Disability Index, and Euro-QoL-5D scores compared to posterior surgery. Patients with a postoperative C2–7 SVA >4 cm did not have improvement of SF-36 PCS, and increased C2–7 SVA was a negative predictor for SF-36 improvement for posterior surgery.
A multicenter, prospective study of adult cervical deformity patients (n=77) with 1-year postoperative follow-up was performed [36]. Most patients underwent posterior (85%) compared to anterior (53%) surgery, with 3-column osteotomy in 24% overall. The authors report promising improvement in Neck Disability Index, neck visual analog pain score, EQ-5D index, mobility, pain/discomfort and anxiety/depression despite a minimal change in myelopathy. The authors suggest that the improvement across multiple quality of life measures without significant recovery of neurologic function may be related to the pathophysiology and chronicity of myelopathy in the setting of cervical kyphosis. In this study, the investigators did not report radiographic outcomes with respect to extent of correction or restoration of alignment.
The same multicenter study group reviewed patients with successful versus failed radiographic outcomes after cervical deformity surgery [37]. They surveyed a number of preoperative clinical and radiographic factors. They observed successful radiographic correction in 54% based on cervical SVA, and 35% based on T1S-CL. Failure to correct cervical SVA was associated with worse preoperative C2 pelvic tilt angle, and worse postoperative C2 slope, T1S-CL, concomitant thoracolumbar deformity, and revision surgery. Failure to correct TS-CL was associated with worse preoperative kyphosis, C2 pelvic tilt angle, and worse postoperative C2 slope and cervical lordosis. The investigators did not study clinical outcome measures or their relationship to radiographic outcome.
Complications from cervical deformity surgery include dysphagia, wound infection, respiratory failure, new sensory nerve deficit, new motor nerve root deficit (most commonly C5 or C8 during C7 PSO), cerebrospinal fluid leak, pseudarthrosis, and instrumentation failure [38]. The rate of new neurological injury has been reported as high as 23.0% [12]. Smith et al. [39] reviewed a prospective multicenter operative database for early surgical complications (<30 days) in 78 adults undergoing deformity surgery. They reported a total of 52 complications, with 28.2% minor complication and 24.4% major complication rate. The most common complications included dysphagia (11.5%), deep wound infection (6.4%), new C5 motor deficit (6.4%), and respiratory failure (5.1%). One (1.3%) mortality occurred. Complication occurrence was related to surgical approach with anterior only (27.3%) having the lowest risk, compared to posterior only (68.4%), and combined (79.3%) surgery. These differences in risk, however, may reflect baseline severity of deformity and invasiveness of osteotomy grade needed for correction, as well as, overall patient functional status. Etame et al. [32] in 2010 conducted a review of 14 retrospective studies (total n=399 patients) with long-term follow-up after cervical spine deformity surgery. They reported a blended mortality rate ranging from 3.1% to 6.7%, major complication rate of 3.1%–44.4%, and overall neurological complication rate of 13.5%. A recent study assessing all-cause mortality in patients undergoing cervical deformity surgery found a 9.2% rate at 1.2 years, underscoring the potentially significant risk in patients with multiple major comorbidities [40].
Among complications after cervical deformity surgery, Distal junctional kyphosis (DJK) uniquely can be a significant source of disability. DJK is the loss of alignment 1 or 2 levels caudal to the lowest instrumented vertebra, and can result from instrumentation failure, spinal fracture, and/or spondylolisthesis. When symptomatic, DJK can cause pain, radiculopathy, myelopathy or progressive deformity. In a review of 101 surgical patients undergoing cervical deformity correction with 2 years follow-up, 24% had radiographic evidence of DJK with only 6% demonstrating clinical findings [41]. Baseline worse radiographic deformity parameters, neurologic deficits, and combined anteriorposterior surgery were associated with increased risk of DJK.
CONCLUSION
Cervical kyphotic deformity may occur naturally due to aging, after prior surgery, trauma or in the setting of pathologic processes. Surgery is the primary treatment for correction of deformity and for neural decompression when present. Surgical decision-making relies on understanding fundamental biomechanical principles, characterization of radiographic parameters, and assessment of curve rigidity, as well as, clinical and neurologic factors. Clinical studies suggest that in properly selected individuals, deformity correction improves HRQoL measures. A relatively high morbidity is associated with surgical treatment indicating the overall severity of the underlying condition, and emphasizing the need for further refinement of surgical strategies.
Notes
The authors have nothing to disclose.