Cervical Sagittal Alignment: Literature Review and Future Directions
Article information
Abstract
Cervical alignment as a concept has come to the forefront for spine deformity research in the last decade. Studies on cervical sagittal alignment started from normative data, and expanded into correlation with global sagittal balance, prognosis of various conditions, outcomes of surgery, definition and classification of cervical deformity, and prediction of targets for ideal cervical reconstruction. Despite the recent robust research efforts, the definition of normal cervical sagittal alignment and cervical spine deformity continues to elude us. Further, many studies continue to view cervical alignment as a continuation of thoracolumbar deformity and do not take into account biomechanical features unique to the cervical spine that may influence cervical alignment, such as the importance of musculature connecting cranium-cervical-thoracic spine and upper extremities. In this article, we aim to summarize the relevant literature on cervical sagittal alignment, discuss key results, and list potential future direction for research using the ‘5W1H’ framework; “WHO” are related?, “WHY” important?, “WHAT” to evaluate and “WHAT” is normal?, “HOW” to evaluate?, “WHEN” to apply sagittal balance?, and “WHERE” to go in the future?
INTRODUCTION
The concept of cervical spinal alignment has gained interest in the field of spinal deformity research over the last decade. However, the number of studies on normative data remain limited [1-5]. Initial studies focused on the correlations between sagittal alignment and outcomes of surgical treatment of cervical myelopathy [6,7]. Changes of sagittal balance following laminoplasty and cervical disc arthroplasty (CDA) were also topics of interest in this period [8-11]. The concept of sagittal spinal alignment had been studied extensively in the thoracolumbar spine since the 2000s, and eventually these concepts were extended to the cervical spine in the 2010s.
The number of studies on cervical sagittal alignment have increased dramatically over the last several years (Fig. 1). Broad areas of research focus in this space have been: (1) correlation of cervical alignment with thoracolumbar spine following surgical treatment; (2) novel measurement parameters correlating cervical spine and thoracolumbar-pelvic alignment including ‘T1 sagittal angle’ (2010, identical to T1 slope) [12], thoracic inlet alignment (2012) [13]; and (3) correlation of health-related quality of life (HRQoL) and cervical radiographic alignment parameters such as cervical sagittal vertical axis (SVA, 2012) [14].
Despite the robust research efforts, the definition of normal cervical sagittal alignment continues to elude us. Further, many studies continue to view cervical alignment as a continuation of thoracolumbar deformity, and do not take into account biomechanical features unique to the cervical spine that may influence cervical alignment, such as the importance of musculature connecting cranium-cervical-thoracic spine and upper extremities. In this article, we aim to summarize the relevant literature on cervical sagittal alignment, discuss key results, and list potential future direction for research using the ‘5W1H’ framework.
“WHO” ARE RELATED?
1. Degenerative Cervical Spine; Laminoplasty, Disc Arthroplasty, Cervical Fusion, Adjacent Segment Pathology
Correlation between cervical sagittal alignment and the outcomes of cervical myelopathy following laminoplasty has been an important topic in the cervical literature. Because the decompression effect of laminoplasty mainly depends on the posterior spinal cord drift, the cervical sagittal alignment has been shown to correlate with outcomes. Since Suda et al. [6] reported correlation between cervical kyphosis and less favorable neurological recovery in 2003, many articles have reiterated the conclusion [7,15-17]. Kyphosis more than 10°–13° was demonstrated to be an important cutoff for cervical laminoplasty. In addition, investigators focused on alignment changes of the cervical spine following laminoplasty [10,15,18]. Many studies concluded that anterior cervical decompression and fusion with lordosis reconstruction was a more appropriate option for kyphotic cervical spine instead of posterior surgery [19-24].
With popularity of CDA, there was an increased interest in studying adjacent segment pathology (ASP) comparing CDA versus anterior cervical discectomy and fusion (ACDF) starting the 2000s. Pickett et al. [8] and Johnson et al. [9] reported preserved global cervical sagittal balance after Bryan prosthesis even with mild kyphotic changes of the CDA segments in 2004, and several studies have presented similar results [11,25,26].
Since then, multiple studies have since reported that the sagittal malalignment might influence development of ASP. In 2011, Faldini et al. [27] presented mean 16-year follow-up results of 107 patients and concluded that proper lordotic alignment of cervical spine is significant to decrease the risk of adjacent segment degeneration. In a systematic review by Hansen et al. [28] in 2012, they found increased risks of ASP associated with malalignment with low-grade evidence. But recently, Snowden et al. [29] reported that the preoperative and postoperative sagittal alignment do not affect on radiographic ASP at following of CDA and ACDF at least 7 years prospectively. Although the evidence is low and the etiology of ASP is multifactorial, it is generally accepted that the malalignment may contribute to development of ASP [30].
2. Thoracolumbar Deformities: AIS, SD, ASD
Since the late 1990s, cervical kyphosis in adolescent idiopathic scoliosis (AIS) is relatively well-known phenomenon with incidence of 36%–40% and thought to be a reactive change to the hypokyphosis of thoracic spine [31]. The spontaneous correction of cervical kyphosis following instrumented fusion of the thoracolumbar deformity has been reported by numerous authors in 2010s [32-37], which is mainly contributed from the restoration of the thoracic kyphosis (TK) and reciprocal changes between the cervical and thoracic segments. In contrast, radiographic analyses of Scheuermann disease (SD) showed hyperlordosis of cervical spine in the literature with similar compensatory mechanism for the hyperkyphosis of the thoracic spine [38,39].
In adult spinal deformity (ASD), extensive research on the global spinal alignment has been performed since the 2000s and 2010s but most research did not include cervical spine. The studies have elucidated lumbopelvic balance, represented by the formula, PI (pelvic incidence)= SS (sacral slope)+PT (pelvic tilt), and spinopelvic compensation mechanism including pelvic retroversion, hip extension, and knee flexion. Although several authors have commented the cervical lordosis (CL) increases per the increased kyphosis, not many studies had not extended interest in the cervical spine. Berthonnaud et al. [40] included the statistical correlation between CL and TK in their analysis of the spinopelvic balance in 2005. Followed studies on this topic mirrored similar correlation between cervical and thoracolumbar alignment [41,42].
Spontaneous improvement of cervical alignment after correction of global sagittal balance following thoracolumbar osteotomy was published by Smith et al. [43] in 2012. Since then numerous articles have presented the reactive changes of cervical spine including CL and cervical spine SVA [44-46]. In 2014, Smith et al. [47] also reported prevalence of cervical deformity (defined as cervical kyphosis > 0° or C2–7 SVA > 4 cm) by 53% in 470 thoracolumbar ASD patients’ database.
Compensatory correction of the thoracolumbar alignment after the correction of the cervical deformity has been reported by Lee et al. [48] in 2016, Mizutani et al. in 2018 [49] and 2019 [50]. Those studies have indicated that the cervical alignment or deformity has significant correlation with thoracolumbar alignment and their changes.
“WHY” IMPORTANT?
1. Correlation With Disc Degeneration, Neck Pain, Clinical Outcomes Following Surgery
The clinical implications of sagittal alignment of the cervical spine remain controversial. Okada et al. [51] in 2009. They followed 487 asymptomatic volunteers with magnetic resonance imaging (MRI) at an average of 11.3 years and found no significant correlation between the sagittal alignment of the cervical spine and clinical symptoms. But several articles have been published the effect of sagittal alignment on the clinical symptoms. Lee et al. [52] (2014) reported increased thoracic inlet inclination is a predictor of chronic neck pain. Yang et al. [53] (2015) reported increase T1 slope is related to cervical disc degeneration. Iyer et al. [54] reported low T1 slope (T1S)-CL and high C2–7 SVA area independent predictors of high preoperative Neck Disability Index (NDI).
Previously, Chin-Brow Vertical angle (CBVA) has been presented as an important parameter of the functional outcomes following corrective osteotomy for ankylosing spondylitis patients [55]. Lafage et al. [56] (2016) found that CBVA of < -4.8° or > 17.7° correlated with an Oswestry Disability Index of 40. The first statistical analysis on the clinical correlation with cervical sagittal parameter was presented by Villavicencio et al. [57] in 2011, which demonstrated increased segmental lordosis was related to higher degree of improvement in clinical outcomes in 122 anterior cervical fusion patients with mean 37.5-month followup. In 2102, Tang et al. [14] presented standing cervical SVA including C2–7 SVA SVA C7orrelated with HRQoL parameters in the cohort underwent posterior cervical fusion. Protopsaltis et al. [58] (2015) reported changes in CL correlated to HRQoL improvement in thoracolumbar ASD. Hyun et al. [59] (2017) presented T1S–CL > 22.2° and C2–7 SVA > 43.5 mm correlated with NDI in their posterior cervical fusion patients. Since then, many studies have presented clinical correlation with cervical SVA and T1S–CL.
However, there have been conflicting articles on their conclusions. Vavruch et al. [60] (2002) reported the reconstruction of disc height and lordosis were not related clinical outcomes after ACDF. Lee et al. [61] (2016) reported no significant difference of HRQoL or number of fusion levels in patients had solid anterior cervical fusion without correlation with SVA or CL. Bao et al. [62] (2017) and Lau et al. [63] (2020) have also failed to identify significant association between CL and HRQoL outcomes in their cervical fusion cohort. This implies there could be a range of alignment providing forgiveness without affecting the HRQoL.
“WHAT” TO EVALUATE AND “WHAT” IS NORMAL?
1. Conventional Parameters: Angular and Translational
The first searchable study on cervical spine alignment published by Borden et al. [1] in 1960. They measured the maximum horizontal distance from the line connecting the posterior part of the dens and posteroinferior corner of C7 and the mean value was 12 mm in random chest lateral radiographs of 180 patients.
The conventional evaluation of cervical alignment can be categorized into 2 categories. The first one is angle measurement. Although there have been several methods have been presented to measure CL, including Gore method [2], tangential method [64] etc., Cobb method is the mainstay since their publication in 1948, measuring angles between the upper endplate of the uppermost segment and the lower endplate of the lowest segment because of the simplicity and high reliability [65,66]. Most researchers divide CL into C0 (occiput)–C2 lordosis and C2–7 lordosis to evaluate the upper cervical and subaxial cervical spine alignment.
Another conventional parameter is SVA. A distance from the C7 plumb line and the posterosuperior corner of S1 considered as C7 SVA in thoracolumbar spine alignment. Cervical SVA was reported by Kuntz et al. [5] for the first time in their study on the normative measurement study. A C2–7 SVA or center of gravity (COG)–C2 or C7 SVA are using the same plumb line method to evaluate the translation of cervical spine. The CBVA, which is measured by an angle between a line drawn from chin to brow and vertical angle, is the first parameter to assess horizontal gaze [55]. Initially it was mainly applied to ankylosed spine but now getting more interest to evaluate the HRQoL related to horizontal gaze in patients with extensive cervicothoracic or thoracolumbar fusion [42,56,67,68].
2. Innovative Parameters, Since the Concept of ‘T1 Slope’
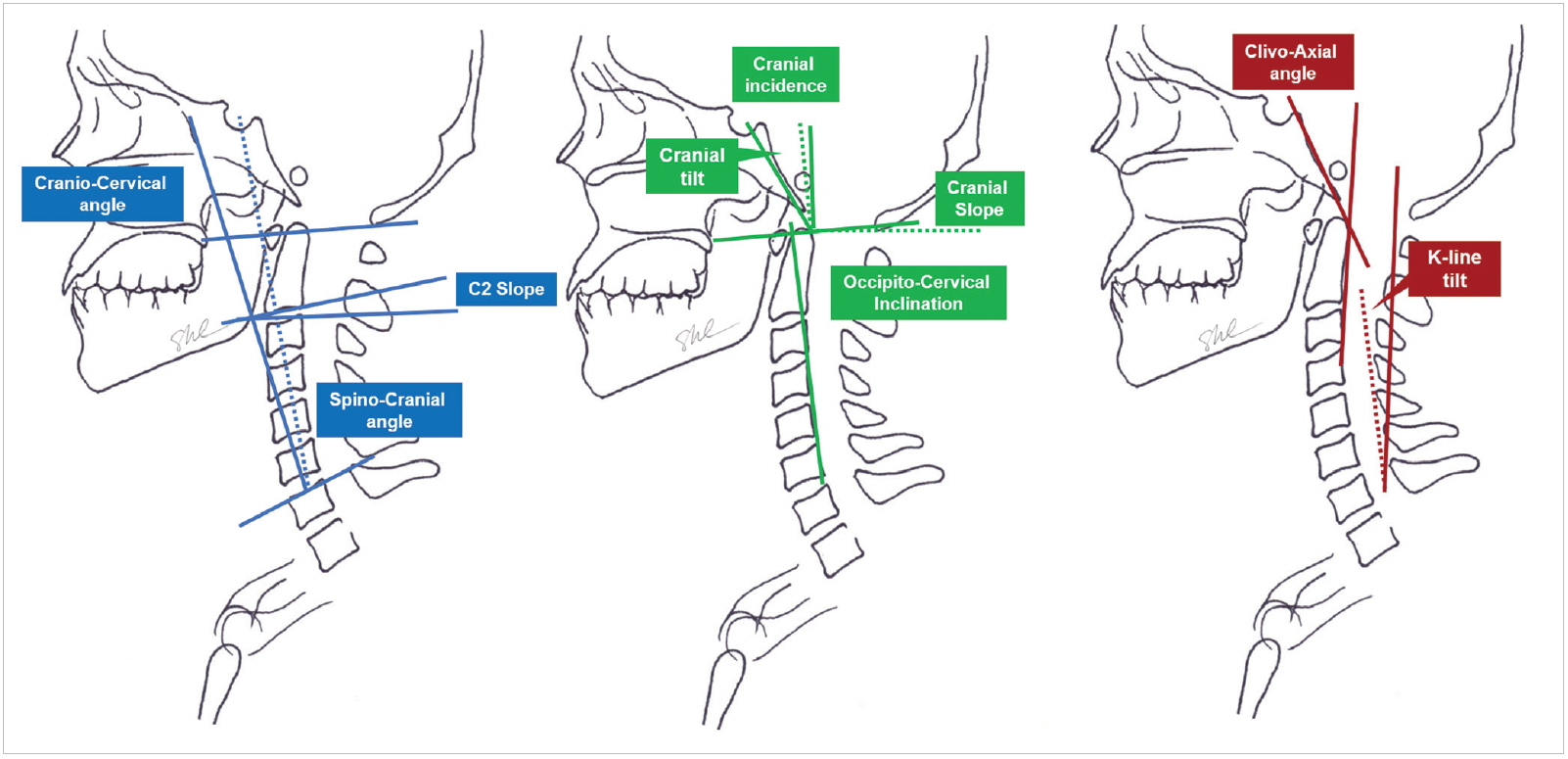
In 2010, Knott et al. [12] presented the use of ‘T1 sagittal angle’ (identical to current T1S) as an important parameter to predict overall sagittal balance of the spine from cervical spine to lumbopelvic alignment. The concept of T1S started to bring additional interest in the cervical spine alignment. Lee et al. [13] (2012), published an innovative thoracic inlet alignment measurement including thoracic inlet angle (TIA), neck tilt (NT), T1S, cranial tilt (CT), and cervical tilt, etc. (Fig. 2). The term T1S was firstly introduced in this article. The concept was based on the idea that the sagittal balance of the cranium and cervical spine could be influenced by the shape and orientation of immobile thoracic inlet to get a balanced upright posture and horizontal gaze like the PI in the pelvis.

Schematic drawings of the conventional cervical alignment parameters including thoracic inlet alignment. SVA, sagittal vertical axis.
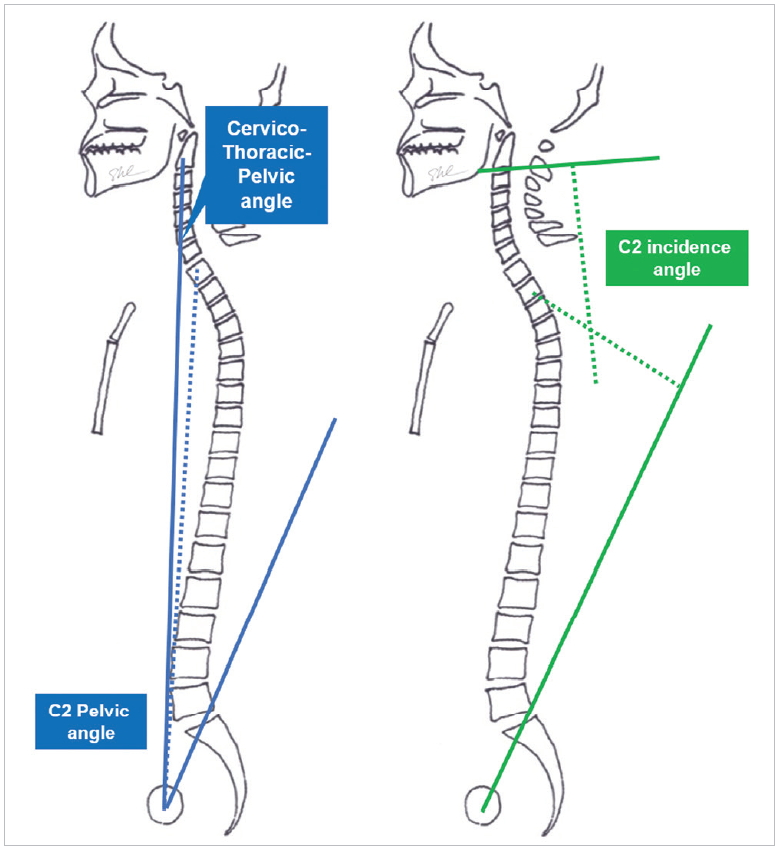
Since then, the concept of T1S widely expanded the variable innovative measurements of cervical spine as well as thoracolumbar spine, pelvis, and lower limb alignment (Table 1, Fig. 3). Studies on numerous innovative parameters have followed with radiographic correlation with the traditional measurement parameters such as TK, lumbar lordosis (LL), PI, SS, etc.
Ames et al. [67] (2015) introduced the parameter T1S–CL in their cervical deformity classification system like PI–LL mismatch in thoracolumbar deformity. Le Huec et al. [69] (2015) proposed a concept of cranial incidence (CI), cranial slope (CS), and CT, with a formula CI=CT+CS, to analyze the anatomical characteristics of crainocervical alignment. They used C7 slope instead of T1S and used spino-cranial angle (SCA) to evaluate the craniocervical alignment. Protopsaltis et al. [70,71] (2017) measured several novel angles including craniocervical angle, C2 pelvic angle, cervicothoracic pelvic angle to evaluate cervical alignment including whole spine sagittal alignment. Yoon et al. [72] (2017) reported occipitocervical inclination. Hashimoto et al. [73] (2018) used a clivoaxial angle to evaluate Dropped head syndrome. Kim et al. [74] (2018) presented K-line tilt as a correlating parameter with C2–7 SVA and T1S–CL. Most recently the measurement extended to upper cervical spine. Protopsaltis et al. [75] (2019) reported C2 slope as another parameter correlates with outcomes and Choi et al. [76] (2019) proposed C2 incidence angle to evaluate the cervical alignment (Fig. 4). Despite of the multiple radiographic parameters that have been described, only T1S and T1S–CL have been shown to correlate with clinical outcomes.
3. Normal Alignment and Compensation; Intra- and Extracervical Spine (Table 2)
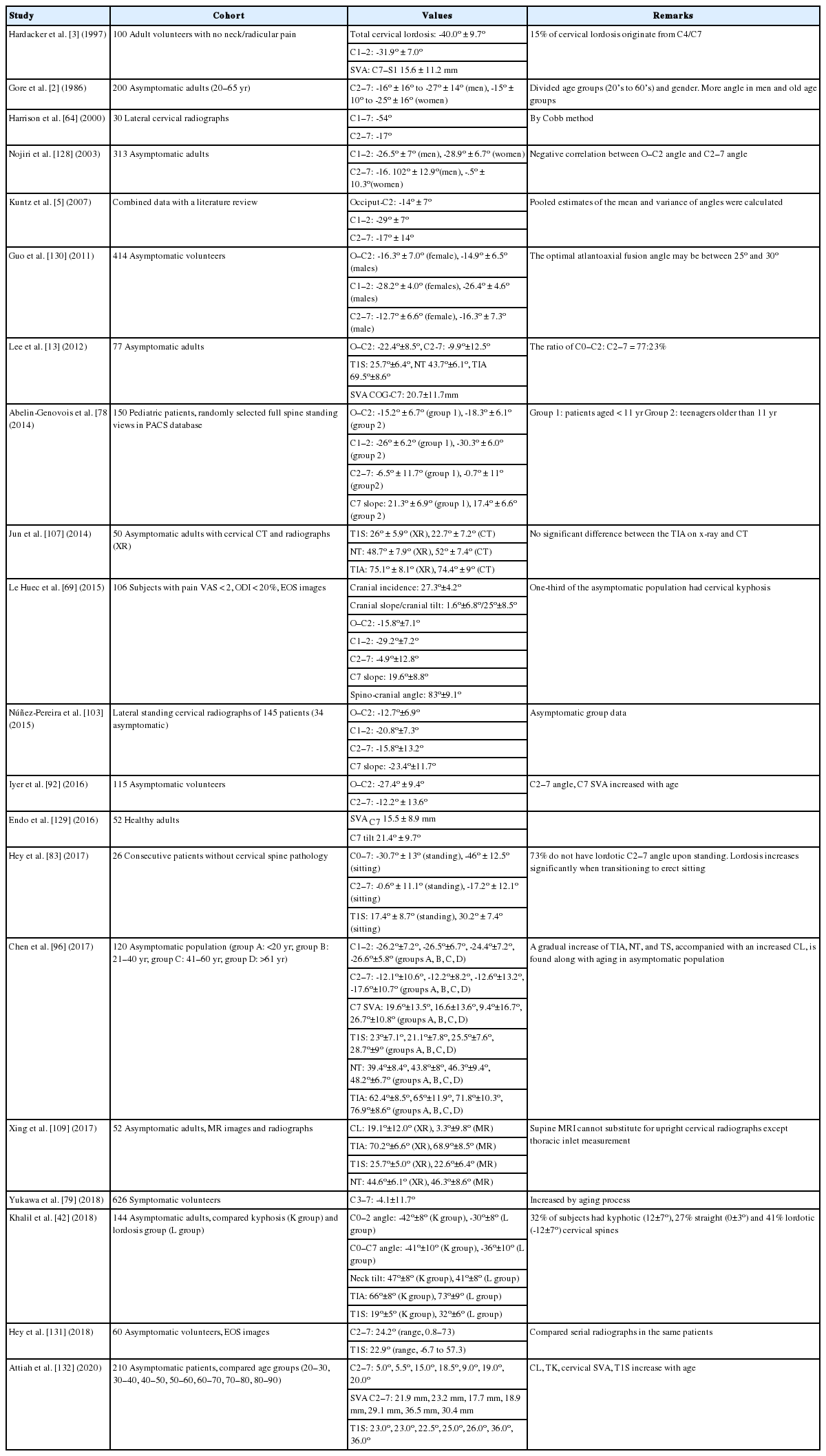
Normative cervical spine measurement values in the asymptomatic cohort in the literature, by the published year order
There is still no consensus definition of ‘normal’ cervical alignment. Although lordosis is accepted as major presentation of natural cervical alignment, it is well known that significant number of asymptomatic cervical spine is not lordotic. Hardacker et al. [3] (1977) already reported kyphotic cervical alignment of 5° or greater in 36% of asymptomatic volunteers in their study. Kim et al. [77] (2018) reported a 26.3% incidence of kyphotic cervical alignment in asymptomatic cohort and Khalil et al. [42] (2018) reported 32% of kyphosis and 41% of lordosis. Overall, the incidence of asymptomatic kyphosis is approximately 30%.
Hardacker et al. [3] (1997) reported normal O–C7 angle as 40°±9.7° lordosis. In their results, most lordosis occurred at the C1–2 angle and the lower cervical spine C4–7 contributed only 15%. Gore et al. [2] (1986) presented mean C2–7 angle as variable as -15°±10° to -27°±14° according to the age group and gender. Since then many normative studies have presented CL in asymptomatic cohort. O–C2 angle ranged from -12.3° to -32.5° and C2–7 angle ranged from -4.1° to -16.3°. Overall, reported total CL (C0–7) was approximately 30° [5,78,79].
Compensation mechanism within and outside of cervical spine is a well-established phenomenon and has been supported by many studies. Kyphosis of a single or multiple segments can be compensated by the upper or lower adjacent segments, and a kyphotic alignment changes in subaxial cervical spine can be compensated by the hyperlordotic upper cervical spine (C0–2) and vice versa [71,80-82]. Kyphotic changes of cervical spine decrease TK to compensation the alignment and keep the ‘cone of economy’ of global spinal balance. Likewise, increased TK causes hyperlordotic cervical alignment and vice versa. An interesting point is that there is no direct correlation between LL and CL in studies on cervical alignment including thoracolumbar spine and pelvic alignment [47,52]. The LL influences TK and has only indirect effect on the cervical alignment [40,41]. Another compensation mechanism between the T1S and CL has presented by Lee et al. [13] (2012). They presented the concept of thoracic inlet alignment and concluded large TIA increased T1 slope and CL and vice versa to preserve neck tile around 44° and horizontal gaze.
Few studies have presented normative cervical SVA, T1 slope, TIA, and NT values. Lee et al. (2012) [13] reported COG–C7 SVA as 20.7±11.7 mm, T1S 25.7°±6.4°, TIA 69.5°, and NT 43.7° in asymptomatic cohort. Hey et al. [83] (2017) reported C2–7 SVA as 8.8±24.2 mm, T1S as 17.4°±8.7°, and Khalil et al. [42] (2018) reported the range from 21–22 mm of COG–C7 SVA, 19°–32° of T1S, TIA 66°–73° and NT 41°–47°. In summary, C2–7 SVA and T1S are reported approximately 20 mm and 25° respectively. Reported TIA and NT values are around 70° and 45° in the literature [42,83-86].
Aging and sex also influence cervical alignment. In many reports, aged population showed increases cervical SVA, CL, and T1S which is mainly contributed from increased TK [4,87-95]. Chen et al. [96] (2017) and Liu et al. [97] (2019) presented increasing TIA and NT with aging process as well as CL and T1S.
“HOW” TO EVALUATE?
1. Conventional Radiographs and Positional Variations
Simple radiographs are the most important tool to evaluate the alignment of spine. However, still there is no established radiographic guideline to evaluate cervical spine sagittal balance. It is well known that position changes in the arm cause significant variation in standing whole spine lateral radiograph [98]. Likewise, many factors influencing on the measurement results in cervical spine lateral radiographs have been reported.
To keep the horizontal gaze, Lee et al. [13] (2012) evaluated cervical spine lateral radiograph in standing position with horizontal Frankfart plane (an extended line connecting the lower border of the orbit and the external auditory meatus) and they evaluated the thoracolumbar alignment with separate standing whole spine lateral radiographs. Park et al. [99] (2015) reported significant decrease T1S and CL in the standing whole spine lateral radiographs with fist on clavicle position, caused by posterior cranial shift in 101 asymptomatic volunteers. Kusakabe et al. [100] (2019) reported 28.7% showed decreased CL and 29.6% showed increased CL in the sitting position compared the standing position with whole spine lateral radiograph. Based on results of the literature, evaluation of cervical spine alignment by either standing whole spine radiographs or sitting cervical spine lateral radiographs will be less reliable [101,102].
Another huddle to accurate measurement of cervical spine radiograph is unclearly visible lower cervical and upper thoracic spine endplate in patients with short neck or high shoulder contour. Measuring C7 instead of T1 has been recommended by several authors because C7 is clearly visible than T1 in more patients, C2–6 Cobb angle and C7 slope are correlated well with C2–7 angle and T1 slope [69,103-106].
2. Newer Measurement Methods: EOS, CT, MRI
Several innovative imaging techniques have been proposed. Singhatandgige et al. [84] (2015) reported reliable results measured by EOS lateral whole-body stereo-radiograph compared to conventional cervical lateral radiograph. Studies presenting measurement of cervicothoracic junction including thoracic inlet alignment using computed tomography or MRI have been published [86,107-110]. The CT or MRI can visualize C7 lower endplate, T1 upper endplate, the end of manubrium well in the midsagittal images better than conventional radiographs [111]. The supine position in axial imaging may potentially skew the weight-bearing neutral position of the cervical spine. Additional considerations are cost and radiation exposure with CT.
“WHEN” TO APPLY SAGITTAL BALANCE?
1. Definition of Cervical Deformity
As there is no consensus on “normal” cervical alignment, the precise definition of cervical deformity is a moving target. Smith et al. [47] (2014) initially defined cervical deformity as C2–7 angle > 0° and C2–7 SVA > 4 cm in their thoracolumbar deformity cohort. But later the same study group proposed C2–7 kyphosis > 10° and C2–7 SVA > 4 cm based on the correlation with HRQoL [67]. Passias et al. [112,113] (2018) expanded the definition of cervical deformity as cervical kyphosis: C2–7 Cobb angle > 10°, cervical scoliosis: coronal Cobb angle > 10°, positive cervical sagittal imbalance: C2–C7 SVA> 4 cm or T1S–CL > 10°, or horizontal gaze impairment: chin-brow vertical angle> 25°.
2. Location of the Deformity
Location of the deformity is an important factor to consider for planning surgical correction. Passias et al. [112] (2018) classified the ‘primary driver’ of the cervical deformity as cervical when the lower instrumented vertebra is higher than C7 and cervicothoracic when LIV is T3 or higher. Lee et al. [114] (2018) proposed C5–T3 angle as the cervicothoracic junction based on the significant correlation between the major radiographic parameters including CL, TK, and clinical outcome parameters.
Lee et al. [115] (2019) proposed a surgical treatment strategy based on T1S and cervicothoracic junction angle (Fig. 5). When T1S is normal and cervicothoracic junction is normal, the deformity is located with the cervical spine so need anteriorposterior surgery. The correction should be on the lower cervical spine including pedicle subtraction osteotomy when T1S is normal and cervicothoracic junction angle is kyphotic. A high T1S and kyphotic cervicothoracic junction angle mean the deformity is on the upper thoracic spine and a high T1S and normal cervicothoracic junction implies the correction should be performed on the mid or lower thoracic spine.
3. Cervical Deformity Classifications Presented and Lessons From Dropped Head Syndrome
To date, several classification systems have been proposed. Lamartina and Berjano [116] (2014) presented spinal sagittal plane deformity classified by the location of the regional deformity and compensation mechanism, however, they did not focus on cervical spine in detail.
Ames et al. [67] (2015) proposed a comprehensive cervical spine deformity classification system based on a modified Delphi approach. The classification system included a deformity descriptor and 5 modifiers that incorporated sagittal, regional, and global spinopelvic alignment and neurological status. The descriptors included: ‘C,’ ‘CT,’ and ‘T’ for primary cervical kyphotic deformities with an apex in the cervical spine, cervicothoracic junction, or thoracic spine, respectively; ‘S’ for primary coronal deformity with a coronal Cobb angle > 15°; and ‘CVJ’ for primary craniovertebral junction deformity. The modifiers included C2–7 SVA, horizontal gaze (CBVA), T1S-CL, myelopathy by modified Japanese Orthopedic Association score, and the Scoliosis Research Society-Schwab classification for thoracolumbar deformity. This system covers wide spectrum of thoracolumbar deformity, neurological status as well as the cervical spine deformity in both coronal and sagittal plane.
Koller et al. [117] (2019) published Cervical Spine Research Society-European classification of cervical deformity. It provided 4 types, A to D, based on global trunk balance/imbalance and cervical (cervicothoracic) kyphosis/lordosis. Virk et al. [118] (2020) have presented a classification for severe cervical deformity. They grouped the patients into 3 sagittal morphotypes: focal deformity, flat neck (large TS–CL and lack of compensation), or cervicothoracic.
Given that most cervical deformity is in the sagittal plane, several classifications have focused on the kyphosis and compensation mechanism from the trunk. The compensation of cervical kyphosis by thoracolumbar spine has been studied for ‘Dropped head syndrome.’ Dropped head syndrome is defined as a severe cervical kyphosis or chin-on-chest deformity in the standing or sitting position causing significant cervical sagittal imbalance. The causes are still unclear but thought to be posterior neck muscle weakness, also known as an isolated neck extensor myopathy. Association with other neuromuscular disease has been reported including amyotrophic lateral sclerosis, polymyositis, mitochondrial myopathy, Lewy body dementia, etc. Because of the disabling nature of deformity, corrective surgery is required in selected cases [70,119,120].
Hashimoto et al. [73] (2018) classified the Dropped head syndrome as SVA+ and SVA– types based on their SVA with similar degree of cervical kyphosis angles. SVA– type includes patients whose cervical kyphosis was compensated by decreased TK and increased LL. SVA+ type means absent compensation mechanism in the thoracolumbar spine. They indicated osteoporotic compression fracture, and/or diffuse idiopathic skeletal hyperostosis at the thoracic region and loss of lumbar lordosis due to lumbar spinal stenosis and degenerative lumbar diseases at the lumbar region. Mizutani et al. [49] (2018) presented a cervical kyphosis classification as ‘head-balanced’ and ‘trunk-balanced’ type in cervical deformity patient cohort. The head-balanced type is defined as the head COG plumb line is balanced on the pelvis and the C7 plumb line is shifted posteriorly to compensate cervical kyphosis by thoracolumbar spine. A trunk-balanced type shows the C7 plumb line is balance on the pelvis and the head COG plumb line is anterior to the C7 plumb line because of the compensation failure by the thoracolumbar spine. Endo et al. [119] (2019) also presented similar classification in Dropped head syndrome patients: positive balanced type (C7 SVA ≥ 0 mm) and negative balanced type (C7 SVA < 0 mm).
The studies of Dropped head syndrome studies explain that the cervical kyphosis compensated by thoracolumbar spine shows decreased TK, T1S and increased LL. But the cervical kyphosis without thoracolumbar compensation shows increased TK, T1S and decreased LL. We could extrapolate that compensation by thoracolumbar spine should be one of the important factors to consider for surgical correction of cervical kyphosis based on the studies of Dropped head syndrome.
“WHERE” TO GO IN THE FUTURE?
1. Thoracic Inlet Alignment Studies and Revisiting the Concept of ‘Neck Tilt’
The studies on cervical alignment based on T1S and thoracolumbar alignment have provided significant advancement in our understanding of cervical alignment. Many studies in the literature lack the possible influence of weight and musculature connecting cervical spine, thoracic cage, and upper extremities.
Lee et al. [13] (2012) introduced the concept of TIA=T1S+NT, similar to the PI= SS+PT in the thoracolumbar spine, based on the postulation that there could be a separate balancing mechanism of the cranium and cervical spine influenced by the shape and orientation of thoracic inlet. Because there is no range of motion in thoracic inlet, TIA could provide an anatomical base for the craniocervical alignment in normal asymptomatic cohort. They indicated large TIA increases T1S to preserve NT around 44° in the conclusions. Since then, several studies using radiograph, computed tomography, and MRI have reiterated the conclusion of the article by normative data.
In a study of Scheuermann Disease, Janusz et al. [38] (2015) reported TIA and T1S decreased after correction of TK but NT did not change significantly. Pan et al. [121] (2017) reported similar changes of thoracic inlet alignment after the correction of posttuberculosis cervical kyphosis. Wang et al. [122] (2018) presented higher T1S and TIA in cervical spondylolisthesis group than nonspondylolisthesis group but the NT was unchanged. Song et al. [123] (2020) reported stable NT values and TIA after correction of kyphotic deformities in patients with Hirayama disease. In the results of those studies, T1S increased and TIA decreased according to the correction of cervico TK, but NT remained stable. There results lend support to the hypothesis that TIA compensates to alignment changes of the cerviothoracic junction, and NT remains stable to preserve physiologic cranial and cervical spine balance. The result is minimization of energy expenditure of head and neck muscles akin to the ‘Cone of Economy’ concept in the erect spine.
2. Preliminary NT Measurement Data
To prove the hypothesis of ‘stable NT,’ we measured thoracic inlet alignment (TIA, SS, NT) as well as major radiographic parameters (CL, TK, LL, PI, SS) in 23 patients who underwent primary cervical spine deformity surgery. The groups were divided into head-balanced and trunk-balanced patients. There was a significant difference in the 2 groups in the T1S (0.9° vs. 46.3°, p< 0.01) and TIA (47.5° vs. 90.2°, p< 0.01) but no significant difference in the NT (46.5° vs. 44°). After the corrective surgery, the head-balanced group showed significantly increased T1 slope and TIA, while the trunk-balanced group showed decreased T1S and TIA (Table 3, Figs. 6, 7).

A cervical deformity patient showing head-balanced kyphosis. The preoperative radiographs show low TIA and low T1S to compensate the cervical kyphosis. The SVAs (blue: SVA COG, yellow: SVA C2, red: SVA C7) show a head-balanced over the pelvis alignment. Also, preoperatively hypokyphosis was noted to compensate the cervical kyphosis and preserve global spinal balance. Postoperative radiographs show reversed SVAs, increased thoracic kyphosis as well as increased T1S and TIA. However, the NT remains stable. T1S, T1 slope; TIA, thoracic inlet angle; SVA, sagittal vertical axis; NT, neck tilt; TK, thoracic kyphosis; LL, lumbar lordosis; PI, pelvic Incidence; KA, knee angle; AA, ankle angle.

A cervical deformity patient showing trunk-balanced kyphosis. The preoperative radiographs show high TIA and high T1S but the thoracic spins is not compensating cervical kyphosis. The SVAs (Blue: SVA COG, Yellow: SVA C2, Red: SVA C7) show a trunk-balanced over the pelvis alignment. The preoperatively hyperkyphosis means that the deformity is contributed from both cervical and the upper thoracic spine. Postoperative radiographs show corrected cervical kyphosis, SVAs, decreased kyphosis as well as decreased T1S and TIA. In this type of cervical deformity, the NT remains stable. T1S, T1 slope; TIA, thoracic inlet angle; SVA, sagittal vertical axis; NT, neck tilt; TK, thoracic kyphosis; LL, lumbar lordosis; PI, pelvic Incidence; KA, knee angle; AA, ankle angle.
Based on these results, several observations can be made: (1) Cervical deformity compensated by the thoracolumbar spine shows decreased T1S and TIA (Fig. 6). (2) Cervical deformity or cervicothoracic deformity without thoracolumbar compensation shows increased T1S and TIA (Fig. 7). (3) Correction of cervical/cervicothoracic deformity normalizes T1S and TIA. (4) NT is unchanged despite surgical intervention (Fig. 8).

Clinical presentation of cervical kyphosis based on the compensation mechanism by the thoracolumbar spine and location of the major deformities. Neck tilt is remaining stable and providing a stable compensation zone like ‘cone of economy’ for the cervical spine. T1S, T1 slope; TIA, thoracic inlet angle; NT, neck tilt; TK, thoracic kyphosis; LL, lumbar lordosis.
3. Prediction of the Ideal Cervical Alignment
Providing optimal alignment targets for surgical reconstruction of an imbalanced cervical spine is another important target of investigation. In general, it is widely accepted that high T1S, increased CK, high cervical SVA requires more CL to get a horizontal gaze.
Diebo et al. [68] (2016) proposed the alignment target of CL as CL= 10–(LL–TK)/2, to achieve ideal CL based on the thoracolumbar alignment. Ajello et al. [124] (2017) presented a result that a C2–C7 SVA < 25 mm and a CL/C7 slope greater than 0.7 had better clinical outcomes than the group less than 0.7. Staub et al. [125] (2019) presented another formula for normative CL= T1S–16.5°±2° in cervical deformity patients’ cohort using correlations between radiographic parameters. Goldschmidt et al. [126] (2020) used more complicated trigonometric methods and reported a novel δ angle subtended by the cervical height also (δ= T1S°CL/2) and 2 complicated formulas to calculate ideal cervical SVA including “SVA= CH× tan (π/180× (T1S−CL)/2)” and “(1.1× T 1)−(0.43× CL)+6.69”. Zhu et al. [127] (2020) included the thoracic inlet alignment and estimated physiologic CL as a formulas: CL= 0.762× T1S−0.392× C2–C7 SVA+0.25× TIA−13.795 (stepwise multiple regression) and CL = 0.417 × TIA−11.193 (simple linear regression), and they proved their formulas showed good correlation with postoperative alignment.
Despite of these efforts, ideal cervical alignment targets continue to elude us. Some proposed formulas are too complex to predict and not easy to utilize them in the clinical settings. Further, some do not consider thoracolumbar compensation mechanism following cervical deformity correction. Planning of correction without considering the compensation mechanism may result in over- or under-correction. Thus, establishing alignment targets for cervical correction that take TL compensation into account in a fruitful area for future research.
CONCLUSIONS
Cervical alignment as a concept has come to the forefront for spine deformity research in the last decade. Studies on cervical sagittal alignment started from normative data and expanded into correlation with global sagittal balance, prognosis of various conditions, outcomes of surgery, definition and classification of cervical deformity, and prediction of targets for ideal cervical reconstruction.
A variety of radiographic parameters have been proposed for evaluation of cervical alignment. However, identifying parameters that correlate with important clinical outcomes remains an area of investigation.
Further, radiographic evaluation method for cervical spine alignment assessment has not been standardized, including position of arms, direction of gaze, etc. Uniform methods of radiographic evaluation would potentially minimize the variability in research results.
Most studies focusing on cervical alignment are based on the concept that the cervical spine is just overlying spinal segment on top of the thoracolumbar spine. These studies do not account for the possible biomechanical influence of the musculature connecting cranium-cervical-thoracic spine and upper extremities. A future classification of cervical deformity needs to include compensation mechanism by the thoracolumbar spine as well as the cervical spine itself, in order to provide the appropriate surgical strategy for reconstruction of the ideal cervical spine alignment.
Notes
The authors have nothing to disclose.