Management of Pseudarthrosis With Implant Failure at a Multilevel Vertebral Column Resection Site: A Case Report
Article information
Abstract
Pseudarthrosis in the setting of 3-column osteotomies such as vertebral column resection (VCR) is not well described, and pseudarthrosis at the VCR site itself has never been reported. This study reports pseudarthrosis with 4-rod implant failure at a multilevel VCR site. The authors report a case of pseudarthrosis in a patient treated previously for severe segmental thoracolumbar kyphosis resulting in significant pain and myelopathic signs in the setting of radiation therapy for metastatic myeloma. This patient initially underwent 2-level VCR (T11, T12) and fusion from T4-sacrum. This was complicated by pseudarthrosis and associated with same-level 4-rod fracture, resulting in prominent, painful implants, and worsening kyphosis. This patient underwent revision VCR during which time significant motion was found only at the site of the prior VCR with a loose anterior cage. A new expandable VCR cage was placed and the spine was reinstrumented, resulting in significant improvement in coronal and sagittal alignment. Pseudarthrosis at a VCR site has not been previously described. Technical considerations presented in the revision procedure include a 6-rod spanning construct, meticulous endplate repreparation, and the generous use of osteo-inductive and -conductive augments to promote solid fusion.
INTRODUCTION
Spinal osteotomies are often employed to increase flexibility in the setting of complex adult spinal deformity (ASD) [1]. When rigid, angular deformity, severe sagittal imbalance, and pathology that requires large curve corrections are present, vertebral column resection (VCR) may be indicated in conjunction with instrumented spinal arthrodesis [2]. Among the complications encountered in ASD surgery, pseudarthrosis is particularly dreaded as it is disabling and often requires complex revision surgery. A retrospective study of 232 patients who underwent surgical treatment of ASD by Kim et al. [3] identified pseudarthrosis in 40 patients (17.2%), most commonly at the thoracolumbar and lumbosacral junctions, with 13 of these patients having underwent an unspecified spinal osteotomy. There are few studies describing pseudarthrosis in the setting of a VCR, and no studies with pseudarthrosis at the VCR site itself.
This case report presents the previously undescribed phenomenon of a pseudarthrosis at a multilevel VCR site.
CASE REPORT
A 42-year-old Caucasian male was initially evaluated for thoracolumbar back pain of 3 months duration with associated right greater than left leg pain and weakness. He had previously undergone a L4–5 decompression, transforaminal lumbar interbody fusion (TLIF), and posterior spinal instrumented fusion (PSIF) for degenerative spondylolistheis with radiculopathy, approximately 1 year prior to presentation at an outside institution. On initial presentation to our institution, his physical examination was notable for stooped forward posture, and myeloradiculopathy characterized by right-sided lower extremity weakness including 4/5 tibialis anterior, extensor hallucis longus, quadriceps, and hip flexors, bilateral positive Babinski sign, and several beats of clonus in both ankles (Fig. 1A). Importantly, he had a history of stage IV melanoma (V600E BRAF mutation) involving the adrenal gland, liver, lung, and bone (most recent fluorodeoxyglucose positron emission tomography/computed tomography [FDG PET/CT] with increased uptake in clavicle, ischium, femur, however, with no obvious spinal metastasis) and was status post targeted immunotherapy. His initial FDG PET/CT 4 years prior to index surgery showed uptake in T10–L1 vertebral bodies for which he underwent targeted radiation therapy 3 years prior to the index surgery. Posteroanterior and lateral radiographs of the spine were obtained on initial presentation and demonstrated prior L4–L5 PSIF, +15 cm of sagittal balance on the sagittal vertical axis, compression fracture deformity of T11 and T12 with marked kyphosis from T10 to L1 of 57° (Fig. 1).

Initial preoperative posteroanterior and lateral spine radiographs (A, B) and clinical photos (C, D) showing prior L4–5 posterior spinal instrumented fusion and marked thoracolumbar segmental kyphosis in the setting of T11 and T12 vertebral body compression fracture deformity.
Given his debilitating pain, profound deformity, and progressive myelopathy, the patient was indicated for surgical intervention. The patient was placed prone on an spinal table with Gardner-Wells tong and 15 pounds of traction and a posterior midline incision from T4 to the sacrum was performed. The prior instrumentation at L4–5 was visualized and removed without complication and with a noted solid fusion mass. The spine was then instrumented beginning with S2 alar-iliac (S2AI) screws, and pedicle screws placed up to L4, with dual-headed screws placed bilaterally at the S1 level. Iliac fixation was utilized distally to promote solid fusion in this patient requiring significant deformity correction in the setting of a long-segment construct. This construct was provisionally distracted with a temporary rod to allow for L5–S1 TLIF with a titanium cage. A L5–S1 TLIF was utilized because long-fusion constructs have high pseudarthrosis rates at this level [4] and because the patient had preoperative L5–S1 disc space narrowing, degenerative spondylolisthesis, radiculopathy referable to L5, and the TLIF cage provided indirect decompression (in addition to the thorough direct decompression that was performed). Following this, pedicle screws were placed up to T4 using a freehand technique as described previously by Kim et al. [5], with accurate screw position confirmed with an intraoperative CT scanner. Next, an all-posterior VCR at T11 and T12 was performed, as previously described by Lenke et al. [6] A custom 20-mm height VCR cage was placed into the anterior defect from T10–L1 and augmented with autologous local bone graft. The cage was then compressed and rods were placed with 4 rods crossing the VCR site. The distal rods bilaterally were 6-mm cobalt-chrome (CoCr), and the proximal rods bilaterally were 5.5-mm CoCr rods. The accessory rods were secured to the construct distally by means of the dual-headed S1 screws and proximally by side-to-side connectors. Accessory rods were secured proximally at T9 on the left and T10 on the right. Specimens were sent from the osteotomy which on Hematoxylin and Eosin stain showed fragments of fibrocartilage and bone, and on immunohistochemistry did not show any positive tumor cells.
At 2 months postoperatively, the patient regained full strength of bilateral lower extremities, improvement in gait, as well as back pain. Repeat FDG PET/CT postoperatively showed remission of his metastatic melanoma at previously active sites. Posteroanterior and lateral radiographs of the spine showed implants in good position without any complications and improved sagittal alignment (Fig. 2). Ten months postoperatively, the patient was involved in a motor vehicle accident. Repeat radiographs taken at an outside institution did not reveal any instrumentation failure immediately after this accident. Thirteen months after the index surgery, the patient returned to clinic due to worsening thoracolumbar back pain, palpable and prominent implants in the distal thoracic spine without threatened skin, and without any neurological deficits or myelopathic signs. Repeat radiographs taken at this visit revealed a fractured left-sided rod at the thoracolumbar junction adjacent to the prior VCR site, disengagement of the 4-rod construct across the VCR site with tilting of the anterior VCR cage, and 40° of segmental kyphosis from T10–L1, all indicative of an obvious pseudarthrosis at the prior VCR site (Fig. 3). Also noted were incidental fractures of both S2AI screws thought to be from sacroiliac (SI) joint motion.
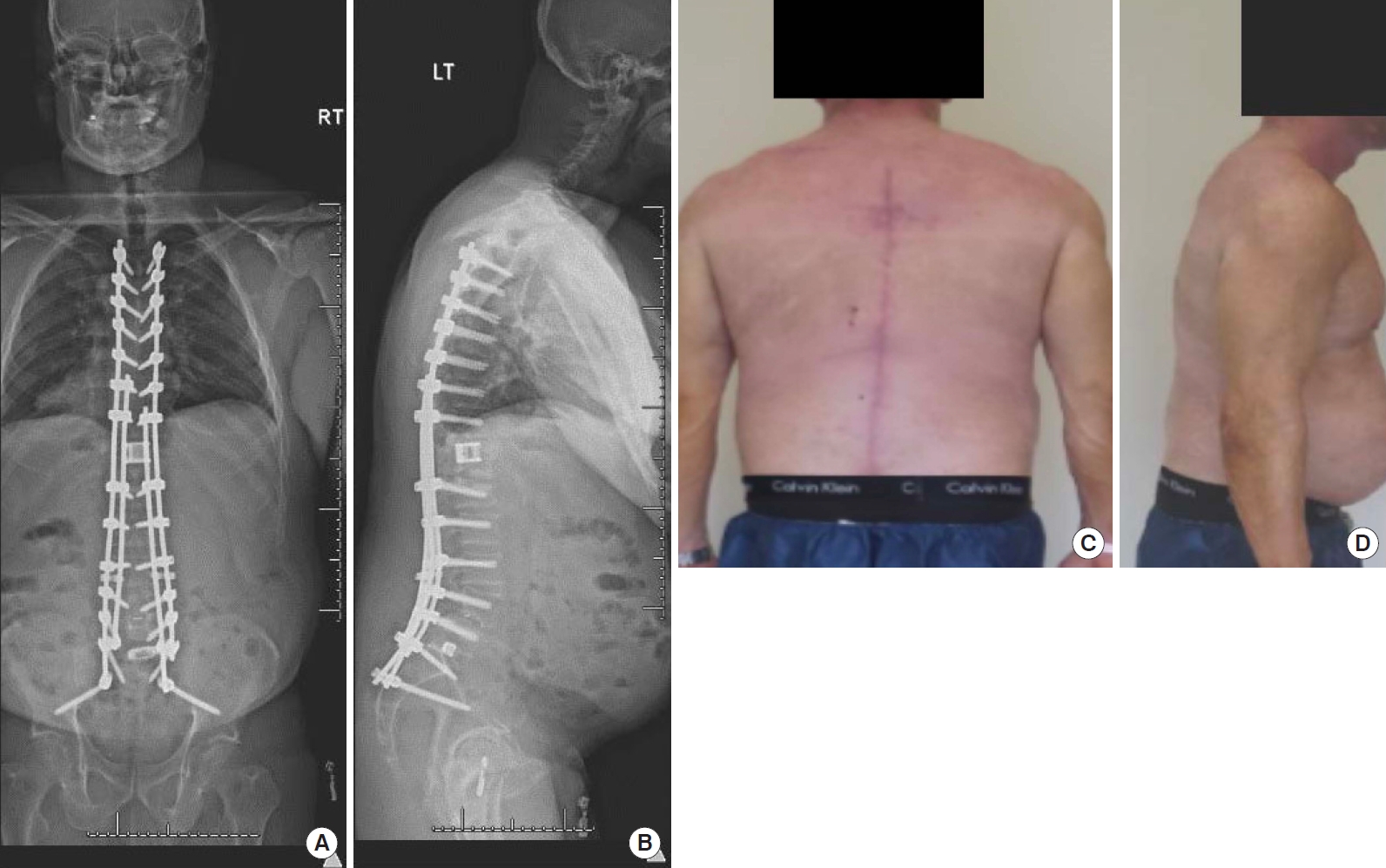
Two-month postoperative posteroanterior and lateral spine radiographs (A, B) and clinical photos (C, D) after initial T4-sacrum posterior spinal instrumented fusion with T11 and T12 vertebral column resection (VCR). Radiographs show a multirod construct with anterior titanium cage spanning the VCR site, with significant improvement in sagittal and coronal alignment relative to preoperatively.
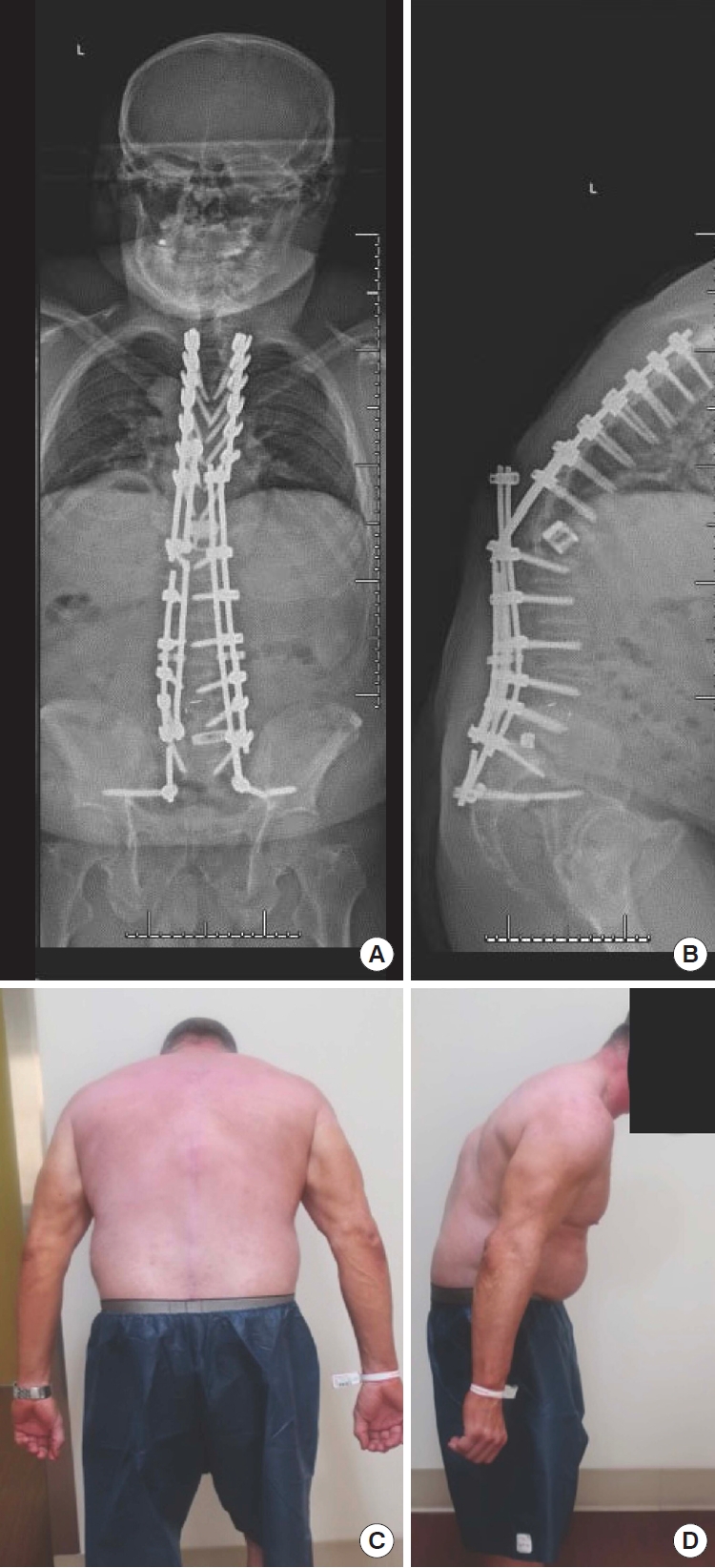
Thirteen-month postoperative posteroanterior and lateral spine radiographs (A, B) and clinical photos (C, D) demonstrate obvious pseudarthrosis at the vertebral column resection site with significant segmental kyphosis and implant failure along with and right-sided S2AI screw fracture and distal left rod fracture between the S1 and S2AI screws.
Given the patient’s prior VCR with obvious pseudarthrosis resulting in failed implants and with associated prominent and painful rod fracture as well as marked sagittal imbalance, he was indicated for prompt revision surgery. Again, the patient was placed prone on an OSI table with a Gardner-Wells tong with 15 pounds of traction. After incision through the prior surgical site, all rods were removed and a thorough fusion exploration was performed. The patient had solid fusion from T4 to T10, significant motion at T10 to L1 across the prior VCR site as expected, and solid fusion from L1 to the sacrum. Bilateral S2AI screws were removed and replaced with 2 new S2AI screws on each side to maximize distal fixation. The prior VCR site was then explored posteriorly to careful remove the scar across the previous laminectomy site, then going lateral on both sides of the dural sac to be able to find the anterior gap of the previous VCR and cage placement. The anterior cage was found to be loose, and easily removed and the cephalad and caudad endplates were further decorticated to fresh, bleeding bone. At this point, an expandable anterior titanium corpectomy cage was packed with autologous bone graft and bone morophogenic protein (BMP) at a dose of 1.2 mg/mm and using a collage sponge carrier. The cage was expanded and compression was placed upon the cage using the temporary posterior rod instrumentation, which resulted in firm locking of the cage in situ. Next new rods were placed from T4-sacrum/ilium with 6 rods placed across the VCR site to maximize stability across this highly unstable pseudarthritic area. Posteriorly, autogenous bone taken from the areas of prior fusion above and below the VCR site along with morselized allograft were used for fusion along with an allograft rib sutured in place across the laminectomy defect from T10–L1. The patient’s postoperative course was uncomplicated and there were no intraoperative neuromonitoring data changes with standing upright radiographs showing correction of the thoracolumbar kyphosis and restoration of a more normal global sagittal alignment (Fig. 4).

Postoperative posteroanterior and lateral spine radiographs (A, B) after revision T11 and T12 vertebral column resection (VCR) and T4-sacrum posterior spinal instrumented fusion demonstrate 6 rods crossing VCR site, an expandable anterior cage and restoration and coronal and sagittal alignment.
Written informed consent was received from this patient.
DISCUSSION
VCR is a powerful adjunct to increase spinal flexibility and reduce deformity in the setting of severe sagittal and/or coronal malalignment and rigid, angular deformity as demonstrated in this case report. Pseudarthrosis, which is commonly defined as lack of solid bridging fusion 1 year postoperatively, is a known complication of long-segment ASD treated with instrumentation and fusion and often requires revision spinal reconstruction [4,7]. Pseudarthrosis has been previously demonstrated to be a risk factor for implant failure, as was seen in this case report [8]. In this patient, there were rod fractures at the level of the VCR pseudarthrosis, as well as incidental distal S2AI screw fractures thought to be secondary to increased motion transfer throughout the SI joints confirmed by a solid fusion of the entire lumbar spine from L1-Sacrum during the revision procedure.
Prior studies have assessed complications after 3-column osteotomies (3CO). Kavadi et al. [9] retrospectively analyzed 26 patients who underwent a 3CO, including pedicle subtraction osteotomies (PSOs) and VCR. In adult patients (19 patients), the most common osteotomy was a PSO which was done in 18 patients, with only 4 patients (includes pediatric patients) in this cohort undergoing a VCR. Seven adult patients in this study suffered from rod breakage, with 6 of them being at the level of the osteotomy. The authors state that pseudarthrosis was often evident at the level of the rod breakage, however, presumably most if not all of these patients had a PSO as 18 of 19 adult patients had this type of osteotomy. Compared to a 2-rod construct, multirod constructs across 3CO sites, as depicted in the index (4 rods) and revision (6 rods) surgeries presented in this case report, have been reported to increase implant stability, and decrease implant failure and symptomatic pseudarthrosis rates [10].
Much of the VCR literature is clouded by patient cohorts that include other types of 3CO. In an attempt to identify outcomes in isolated VCR patients, Iyer et al. [11] performed a systematic review in 2016 that only identified one study (out of 11 assessed) that identified a pseudarthrosis in the setting of a VCR. This study was by Suk et al. [12] in which 25 patients with fixed lumbosacral deformity underwent posterior VCR, most commonly for congenital scoliosis or kyphoscoliosis. On 2-year follow-up, one patient developed a pseudarthrosis proximal to the VCR site that resulted in progressive deterioration of sagittal balance. More recently, Atici et al. [13] retrospectively assessed 17 patients who underwent posterior VCR for severe angular kyphosis in the setting of congenital pathology, posttuberculosis deformity, and neurofibromatosis. One patient was noted to have pseudarthrosis with unilateral rod fracture 18 months postoperatively, and another with pseudarthrosis and bilateral rod fracture 6 months postoperatively. It is unclear if there was a pseudarthrosis at the level of the VCR in these 2 patients, although the authors did note that they both underwent revision surgery that involved rod replacement, debridement and decortication of the pseudarthrosis site and placement of allograft, however, there was no mention of cage exchange so it is unknown, but possible that it involved the actual VCR site itself.
This case report is the first study to report on pseudarthrosis occurring at the site of a multilevel posterior VCR. It is not entirely understood why this patient went on to develop a pseudarthrosis, although he certainly did have inherent risk factors that included having a multilevel VCR with increased stress on the rods resulting in increased bending forces. He also may have been a poor host since he had prior spinal radiation therapy in the setting of metastatic melanoma, which likely decreases the osteoinductive potential for bony bridging. Additionally, the patient was on immunotherapy before and after his surgery which may have contributed to impaired bone healing. Technical considerations in this patient’s revision surgery included spanning the VCR site with 6 rods to increase posterior stability, locking in a structural expandable cage for optimal anterior biomechanical stability, meticulous repreparation of endplates, and the generous use of anterior and posterior bone grafting to promote solid fusion. An expandable cage was utilized in the revision procedure because it is thought to be more effective at providing anterior column support in the setting of posterior VCR, and has the added benefit of permitting optimal fit into a resection site and fine-tuning deformity correction in vivo [14,15]. The risk of BMP use in a patient with a history of malignancy is not fully understood, with various large-scale meta-analyses showing either a dose-dependent risk or no increased risk at all [16,17]. In this case report, BMP was utilized after close consultation with the patient’s oncologist who felt that there was no active metastatic spinal disease, and this was also corroborated on intraoperative pathology. Prompt recognition and treatment of pseudarthrosis with implant failure at prior multilevel VCR sites is imperative to optimize spinal alignment and avoid neurologic deterioration due to the inherent instability present due to 3-column involvement.
Notes
The authors have nothing to disclose.
