Utility of the MISDEF2 Algorithm and Extent of Fusion in Open Adult Spinal Deformity Surgery With Minimum 2-Year Follow-up
Article information
Abstract
Objective
Long-segment fusion in adult spinal deformity (ASD) is often needed, but more focal surgeries may provide significant relief with less morbidity. The minimally invasive spinal deformity surgery (MISDEF2) algorithm guides minimally invasive ASD surgery, but it may be useful in open ASD surgery. We classified ASD patients undergoing focal decompression, limited decompression and fusion, and full correction according to MISDEF2 and correlated outcomes.
Methods
A retrospective study of ASD patients treated by 2 surgeons at our hospital was performed. Inclusion criteria were: age > 50, minimum 2-year follow-up, and open ASD surgery. Tumor, trauma, and infections were excluded. Patients had open surgery including focal decompression, short segment fusion, or full scoliosis correction. All patients were categorized by MISDEF2 into 4 classes based upon spinopelvic parameters. Perioperative metrics were assessed. Radiographic correction, complications and reoperation were recorded.
Results
A total of 136 patients met inclusion criteria. Mean follow-up was 46±15.8 months (range, 24–118 months). Forty-seven underwent full deformity correction, 71 underwent short segment fusion, and 18 underwent decompression alone. There were 24 cases of class I, 66 cases of class II, 23 cases of class III, and 23 cases of class IV patients. Patients in class I and II had perioperative complication rates of 0% and 16.7% and revision rates of 8% and 21.2% when undergoing focal decompression or limited fusion. However, class II patients undergoing full correction had higher perioperative complications rate (p=0.03) and revision surgery rates (p=0.047). This difference was not seen in class III patients (p>0.05). All class IV patients underwent full correction, but they had higher perioperative complication rates (p<0.019), comparable revision surgery rates (p=0.27), and better radiographic realignment (p<0.001). In addition, full deformity correction was associated with longer length of stay, increased blood loss, and longer operative time (p<0.001).
Conclusion
The MISDEF2 algorithm may help guide ASD surgical decision making even in open surgery, with focal treatment used in class I and II patients as a viable alternative and full correction implemented in class IV patients because of severe malalignment. However, class II patients with ASD undergoing full deformity correction do have higher complication rates.
INTRODUCTION
Adult spinal deformity (ASD) surgery usually requires long-segment fusion to address the entire pathology, but the morbidity is not trivial. Foraminal up-down compression causing radiculopathy may prompt the patient to seek surgical care because of disabling pain. Such disabling symptoms may manifest from the focal pathology (radiculopathy or listhesis), not from the chronic scoliosis. In such patients, one option may be to treat the focal pathology, especially in frail patients or in patients who do not want a multilevel fusion [1].
There is a concern that a decompression only in spinal deformity may simply worsen the deformity and result in symptom recurrence or progression [2]. There is also the concern that short-segment fusion fails to correct the deformity and that the remainder of the unfused curve may continue to cause symptoms [3]. Both the limitations of focal surgeries and the morbidity of complete scoliosis correction capitulate the need for guidance with regard to choosing the right type of surgery for each patient [3-6]. Silva and Lenke [7] published a scheme that presented 7 types of treatment for ASD, but there was no patient cohort to validate this scheme as to its efficacy, durability, or surgical appropriateness. However, with the advent modern minimally invasive surgery (MIS), the feasibility and advantages of MIS ASD surgery began to emerge [8]. To specifically address the role of focal surgery using MIS techniques, the minimally invasive spinal deformity (MISDEF) algorithm was published, later updated to MISDEF2 to incorporate such advanced MIS techniques as the mini-open pedicle subtraction osteotomy (PSO) and anterior column re-alignment/release (ACR) [9-12]. Because the diagnosis of ASD is the same regardless of MIS or open treatment and because many surgeons now treat ASD with both open and MIS surgery, we wished to examine the applicability of the MISDEF2 algorithm in open ASD surgery.
MATERIALS AND METHODS
1. Patient Population
A retrospective study of ASD patients who underwent open surgical correction by 2 attending spine surgeons at our hospital from 2006 to 2016 was undertaken. Inclusion criteria were: minimum 2-year follow-up, age > 50 years, degenerative scoliosis (Cobb angle> 10°) with or without kyphosis, and open ASD surgical treatment with either decompression alone, decompression with fusion ≤ 3 levels, full ASD correction encompassing entire scoliosis Cobb angle or correction of sagittal imbalance. Patients who underwent decompression or decompression with fusion did not undergo deformity correction. Infection, tumor, and trauma were excluded. Patient demographics, perioperative variables, complications, and revision surgery rates were collected.
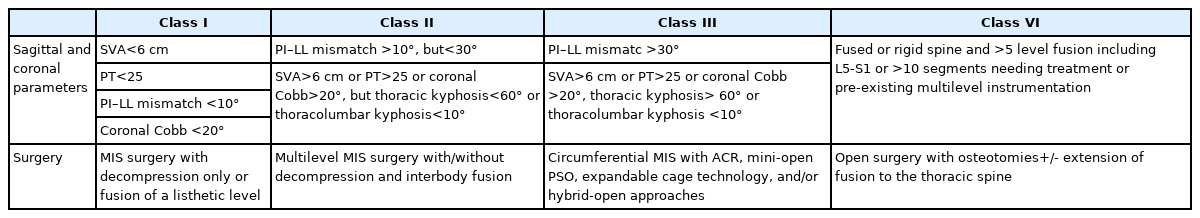
2. The MISDEF Algorithm
Mummaneni et al. [9] proposed the MISDEF algorithm and revised version [10] to provide a guideline for surgeons to choose an MIS approach for ASD surgery. The revised algorithm is based on the radiographic parameters: sagittal vertical axis (SVA), pelvic tilt (PT), pelvic incidence (PI) minus lumbar lordosis (LL) (PI–LL) mismatch, and coronal Cobb angle. Additionally, the algorithm considers whether the spine is rigid, the extent of fusion needed, and pre-existing instrumentation (Table 1). We retrospectively classified patients undergoing surgery for ASD according to MISDEF2 and correlated outcomes.
3. Radiographic Measurements
Full-length 36-inch anteroposterior and lateral radiographs were obtained preoperatively and at last clinic follow-up. Radiographic analyses included measurements of SVA, LL, thoracic kyphosis (TK), thoracolumbar kyphosis (TLK), PI, sacral slope, PT, PI–LL, and pre- and postoperative Cobb angles. All patients were classified by MISDEF2 into 4 classes (class I: SVA < 6 cm, PT< 25°, PI–LL < 10°, Cobb< 20°; class II: SVA> 6 cm, PT > 25°, PI–LL > 10° < 30°, Cobb > 20°; class III: LL–PI > 30°, TK > 60°, TLK > 10°; and class IV: > 5-level fusion including L5–S1 or > 10 levels) (Table 1).
4. Surgical Technique
In the decompression only group, patients underwent bilateral hemi-laminotomies with preservation of the spinous processes and interspinous ligaments. In the decompression with limited fusion, the patients underwent laminectomy and instrumented fusion at the levels of decompression. Patients who underwent full correction had multilevel instrumentation to span the entire Cobb angle.
5. Statistical Analysis
All data collection and radiographic analysis was performed either a spine fellow or an attending spine surgeon. Analysis of variance was used to detect if there was a difference among the 3 groups. The chi-square test was used to compare the differences in complication and revision rates among the 4 MISDEF2 classes. A p<0.05 was regarded as statistically significant. IBM SPSS Statistics version 20.0 (IBM Corporation, Armonk, NY, USA) was used.
RESULTS
1. Comparisons of Demographic, Clinical, and Radiological Parameters
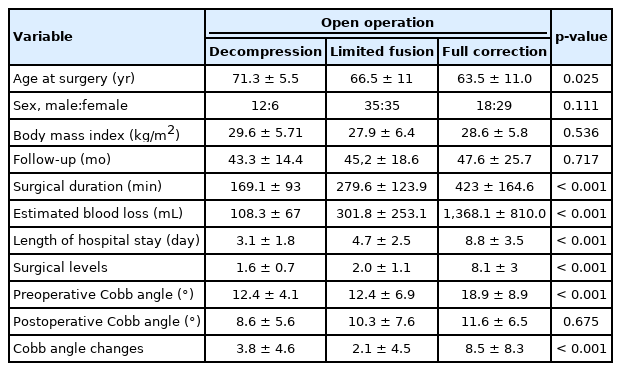
One hundred thirty-six patients met inclusion criteria, with 71 females and 65 males (Table 2). There were 24 cases of class I, 66 cases of class II, 23 cases of class III, and 23 cases of class IV patients. Forty-seven underwent full deformity correction, 71 underwent limited decompression and fusion, and 18 underwent decompression alone. The mean age was 71.3±5.5 years (range, 55–86 years). The mean body mass index was 28.4 kg/m2. The mean follow-up was 46±15.8 months (range, 24–118 months). The average number of surgical levels was 1.6 for decompression alone, 2.0 for limited fusion, and 8.1 for full correction. The mean operative time was 169 minutes for decompression alone, 279.6 for limited fusion, and 423 for full correction. The mean estimated blood loss was 108.3 mL for decompression alone, 301.8 mL for limited fusion, and 1,368.1 mL for full correction. The average length of stay was 5.9±2.8 days (Table 2).
Focal decompression had 4 class I, 12 class II, 2 class III, and 0 class IV; limited fusion had 20 class I, 38 class II, 13 class III, and 0 class IV; and full correction had 0 class I, 16 class II, 8 class III, and 23 class IV. The mean preoperative coronal Cobb angle was 12.4°±4.1° for decompression alone, 12.4°±6.9° for limited fusion, and 18.2°±9.8° for full correction. The mean postoperative coronal Cobb angle was 8.6°±5.6° for decompression alone, 10.3°±7.6° for limited fusion, and 11.6°±6.5° for full correction. There was a statistically significant difference in the coronal Cobb angle correction among the 3 types of surgeries (p<0.001) (Table 2).
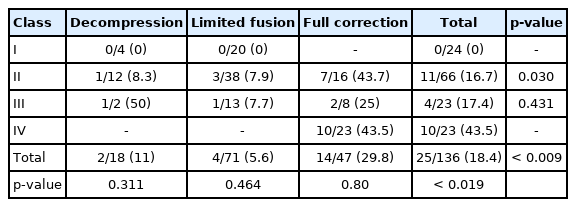
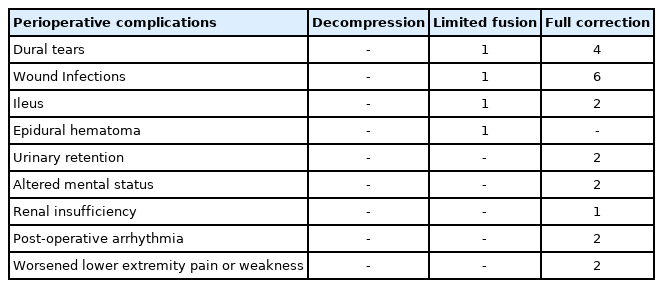
2. Perioperative Complication and Revision Surgery
When analyzing by MISDEF2, patients in classes I and II had peri-operative complication rates of 0/20 and 4/50 (8%) and revision rates of 2/24 (8%), and 6/50 (12%) when they underwent focal decompression or limited fusion (p=0.5, p=0.74) (Figs. 1, 2). No class I patient underwent full correction. Class II patients undergoing full correction had higher revision surgery rates (50%, 8 of 16) and complication rates (43.7%, 7 of 16) than patients undergoing focal decompression or limited fusion (p=0.047, p=0.030) (Tables 3, 4; Fig. 3). There was no difference in perioperative complication and revision rates for class III patients regardless if they underwent limited fusion or full correction (p=0.541, p=0.431) (Tables 3, 4). All class IV patients underwent full correction (Fig. 4), and they had higher perioperative complication rates (43.5%, 10 of 23) than class I patients (0 of 24), class II patients (16.7%, 11 of 66), and class III patients (17.4%, 4 of 23) (p<0.019) (Table 4). The revision rate of class IV patients 8 of 23 (34.8%) was not statistically different compared to class I (8%, 2 of 24), class II (21.2%, 14 of 66), and class III (13%, 3 of 23) (p=0.27) (Table 3). Compared to focal decompression and limited fusion, full correction resulted in better coronal radiographic realignment (Cobb angle correction was 3.8°±4.6°, 2.1°±4.5°, and 8.5°±8.3° respectively for decompression, limited fusion and full correction) (p<0.001) (Table 2). Full deformity correction was also associated with longer length of stay (3.1±1.8, 4.7±2.5, and 8.8±3.5 days), more blood loss (108.3±67, 301.8±253.1, and 1,368.1±810 mL), and longer operative times (169.1±93, 279.63±123.9, and 423±164.6 minutes), respectively for decompression, limited fusion and full correction (all p<0.001) (Table 2). The reasons for revision surgery and perioperative complications are listed in Tables 5 and 6.
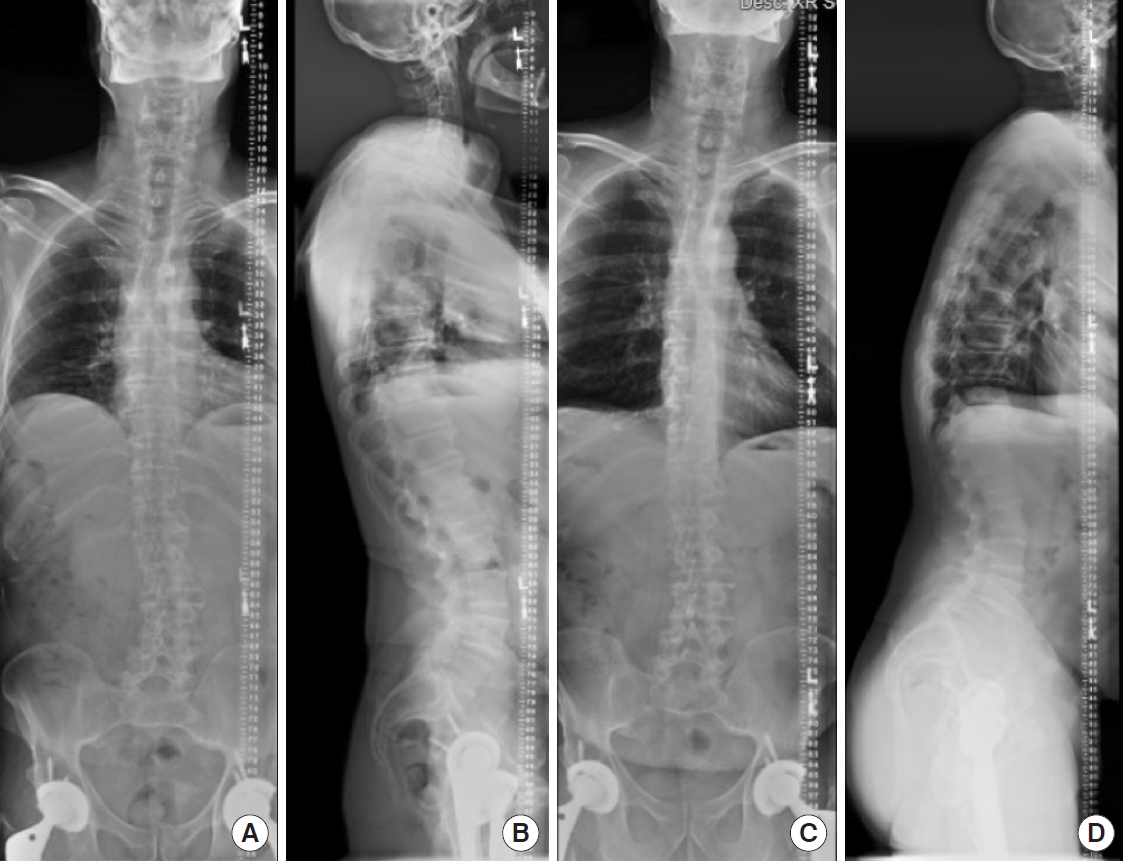
MISDEF2 algorithm class I patient with compression alone. Preoperative coronal and sagittal parameters: sagittal vertical axis, 23 mm; Cobb angle, 14°; pelvic incidence (PI), 61°; pelvic tilt, 18°; sacral slope, 43°; lumbar lordosis (LL), -64°; PI–LL, 3°. (A) Preoperative anteroposterior (AP) radiograph. (B) Preoperative lateral radiograph. (C) Postoperative AP radiograph at 2-year follow-up. (D) Postoperative lateral radiograph at 2-year follow-up.
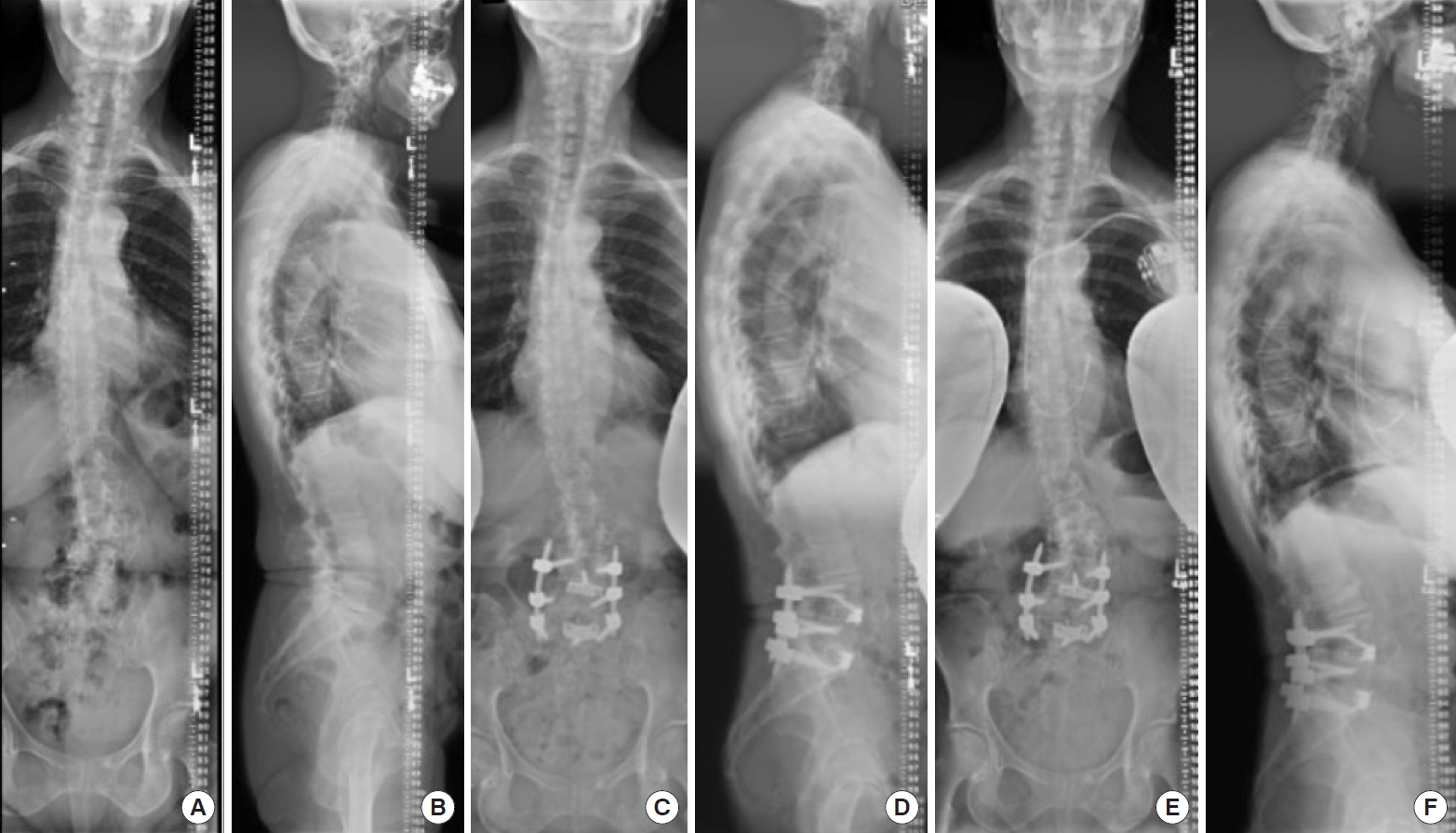
MISDEF2 algorithm class II patient with limited fusion. This was planned as a minimally invasive spinal (MIS) procedure, but converted to open. Because the MIS equipment was ready, the MIS rods were used even though the procedure was open. Preoperative coronal and sagittal parameters: sagittal vertical axis, 20 mm; Cobb angle, 22°; pelvic incidence (PI), 44°; pelvic tilt, 15°; sacral slope, 29°; lumbar lordosis (LL), -40°; PI–LL, 4°. (A) Preoperative anteroposterior (AP) radiograph. (B) Preoperative lateral radiograph. (C) Postoperative AP radiograph at 1-year follow-up. (D) Postoperative lateral radiograph at 1-year follow-up. (E) Postoperative AP radiograph at 3-year follow-up. (F) Postoperative lateral radiograph at 3-year follow-up.

MISDEF algorithm class II patient with full correction. Preoperative coronal and sagittal parameters: sagittal vertical axis, 68 mm; Cobb angle, 31°; pelvic incidence (PI), 45°; pelvic tilt, 24°; sacral slope, 21°; lumbar lordosis (LL), -25°; PI–LL, 20°. (A) Preoperative anteroposterior (AP) radiograph. (B) Preoperative lateral radiograph. (C) Postoperative AP radiograph at 3-month follow-up. (D) Postoperative lateral radiograph at 3-month follow-up. (E) Postoperative AP radiograph at 1-year follow-up. (F) Postoperative lateral radiograph at 1-year follow-up proximal Junctional Kyphosis.
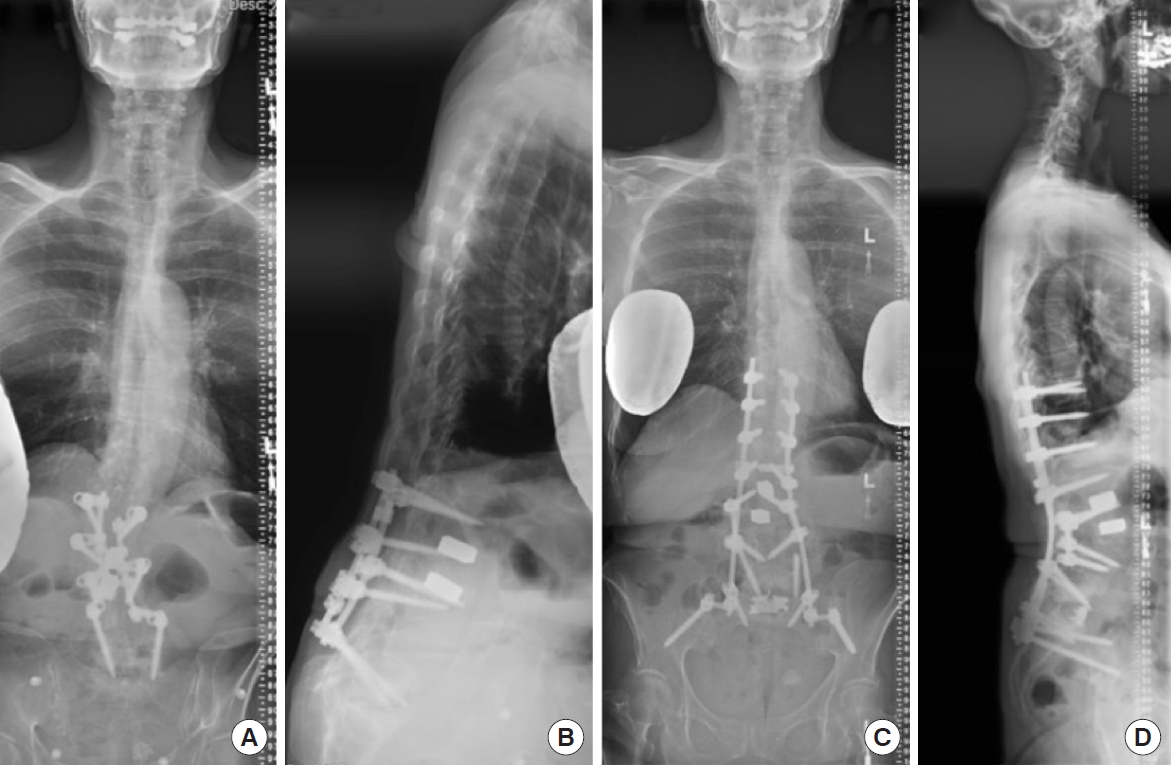
MISDEF algorithm class IV patient with full correction. Preoperative coronal and sagittal parameters: sagittal vertical axis, 145 mm; Cobb angle, 20°; pelvic incidence (PI), 64°; pelvic tilt, 39°; sacral slope, 25°; lumbar lordosis (LL), -15°; PI–LL, 49°. (A) Preoperative anteroposterior (AP) radiograph. (B) Preoperative lateral radiograph. (C) Postoperative AP radiograph at 2-year follow-up. (D) Postoperative lateral radiograph at 2-year follow-up.
DISCUSSION
The treatment of adult scoliosis can be challenging with high complication rates, complex treatment planning, and an aging, osteoporotic population. Patients with long-standing scoliosis for decades may not have disabling back pain that leads to surgery, but lateral listhesis, spondylolisthesis, or severe stenosis may drive the patient towards surgical treatment. Such patients may simply want their neurogenic and radicular symptoms eliminated with a focal fusion of the listhetic levels and not an entire scoliosis fusion. However, treating a limited portion of the scoliotic curve leaves the rest of the curve untreated and the potential for further degeneration because of partial fusion. Further, there are cases of severe sagittal or coronal imbalance, and complete realignment of the spine is really the only solution to alleviate disability. Finally, there are cases in which the scoliosis itself can be extremely painful because of a high Cobb angle that can no longer properly support the weight of the torso. In our study, we found that the treatment algorithm of MISDEF2 to open spinal deformity has potential to be relevant and applicable.
The first consideration is to ensure that surgery has a high chance of alleviating the patient’s symptoms. Performing a hemi-laminotomy or adding another fusion level on in a patient with iatrogenically fused flatback and back pain because of a forward stooped posture will most likely be a failure, leading to disappointment for both the surgeon and patient. Performing the proper operation for the patient should still be the goal of the surgery. The second consideration is to weigh the morbidity and the patient’s medical comorbidities with the risks and benefits of surgery.
Guidelines for the appropriate treatment options in adult scoliosis are few but studies have reported on the variable surgical strategies for adult scoliosis. Lee et al. [13] reported that short fusion may be a reasonable option in patients with de novo adult degenerative lumbar scoliosis without sagittal imbalance. However, this report was a meta-analysis, not a direct comparison between the two groups. Nonetheless, their review indicated that limited fusion in balanced spines was associated with less morbidity than full fusion with similar decrease in disability in both groups. Weidenbaum [6] reported success with decompression without fusion in adult scoliosis patients when the primary complaint was not the curve itself. However, this was a limited series without any direct comparison group. Given the very powerful methods of indirect decompression with modern interbody fusion, Chou et al. [14] and Amara et al. [15] have reported that limited fusion of the fractional curve in adult scoliosis can achieve comparable reduction of leg pain. Although there were comparable immediate results with regard to pain reduction, longer term revision surgery rates appeared to be higher in fusion of the fractional curve only. Lee et al. [16] evaluated scoliosis curve progression in limited fusion cases compared to the natural history of scoliosis progression, and they found no difference in curve progression between the 2 groups. However, their study focused on surgery for degenerative lumbar stenosis who happened to have some component of scoliosis, not scoliosis patients per se.
The MISDEF2 algorithm guides minimally invasive ASD surgery, but it conceptually makes sense to also guide open ASD surgery since the pathology is the same, regardless of treated MIS or open. Using a modified Delphi approach, the MISDEF2 algorithm and recommends 4 treatment classes that incorporate such newer MIS approaches as the ACR [17] and minimally invasive PSO [11]. MISDEF2 takes into account spinopelvic parameters and Cobb angle magnitude, and it also accounts for whether the spine is rigid. Although initially designed for MIS deformity surgery, we retrospectively classified our cohort of deformity patients undergoing focal decompression, limited decompression and fusion, and full correction by the MISDEF2 algorithm to evaluate the feasibility of using the algorithm in open surgery. Consistent with the decision tree of MISDEF2, class I and II patients who underwent limited and focal surgery did not have higher revision rates than full correction patients, indicating that in fairly well-balanced spines, patients who present with isolated stenosis or listhesis may consider a focal operation instead of correction of their entire scoliosis. This may be secondary to larger surgeries in class II having higher complication rates, but focal surgeries being fairly effective, precluding revision surgery complications. In class III, however, many of these patients may have needed full correction, yet more focal surgeries resulted in complications because of inadequate correction. These findings are consistent with previous studies. Simmons [18] and Chen et al. [19] have reported that decompression with limited fusion without deformity correction is reasonable in patients who have moderate to severe stenosis affecting 3 or more levels, smaller curves (< 30°), no progression of deformity, and no sagittal malalignment [18,19]. Glassman et al. [20] also reported similar findings. In general, small curves (10°–20°) with limited rotation and normal sagittal balance were identified as potential candidates for decompression alone. Moderate curves (15°–40°) with segmental instability, significant rotation, or severe concave compression, may be candidates for decompression and fusion with only limited deformity correction. Larger curves (> 40°) or patients with significant coronal or sagittal imbalance generally undergo decompression, fusion, and full deformity correction [20]. However, consistent with previously published reports, full correction surgery was associated with more length of stay, more blood loss, and more operative time (p<0.001) (Table 2). In addition, full correction had higher perioperative complication rates than focal decompression or limited fusion (p<0.009). However, full correction also resulted in better radiographic correction (p<0.001).
There are limitations for this paper. First, it is a retrospective, single center study. Second, the MISDEF2 algorithm was designed for MIS deformity surgery, not open deformity surgery. Applying this algorithm to open surgery is a novel and unchartered concept. However, our application of the MISDEF2 algorithm to open cases yielded results that are consistent with the underlying principles of the MISDEF2 and consistent with previously published literature regarding focal surgeries compared to full corrective surgeries for adult scoliosis. Third, the actual surgeries that were carried out had selection bias; older, more frail patients may have undergone smaller surgeries because they simply could not have tolerated larger reconstructive procedures. This selection bias should be considered when interpreting the data. Fourth, the selection of surgery types and the MISDEF2 were retrospectively compiled; the actual selection of surgery was implemented well before the development of MISDEF2. Thus, the surgical selection was based upon surgeon judgement and patient frailty, but the application of the MISDEF2 was retrospectively applied. This could have resulted in selection bias and confounding error. However, the classification of the scoliosis itself was performed via MISDEF2, and the surgeries were analyzed only after classification. Thus, “appropriateness” of surgery was categorized after application of MISDEF2 classification, not as an actual choice of surgical technique. The strengths of this manuscript are minimum 2-year follow-up, complete evaluation of all scoliosis patients with 36-inch standing films, and data analyzing revision surgery and complication rates.
CONCLUSION
In patients who have deformities within class I and II by MISDEF2, open surgeries with decompression only and focal fusions may be viable options for surgical treatment. However, class II patients with ASD appear to have higher complication rates with full correction. Class III patients may be candidates for limited surgery, but this should be individualized with each patient. Generally, class IV deformities should undergo full correction and realignment of the spine. The MISDEF2 algorithm—although designed for MIS deformity surgery—may also be useful for surgical decision making in open ASD surgery.
Notes
The authors have nothing to disclose.