The Last Touched Vertebra on Supine Radiographs Can Be the Optimal Lower Instrumented Vertebra in Adolescent Idiopathic Scoliosis Patients
Article information
Abstract
Objective
To determine whether the last touched vertebra (LTV) on supine radiographs is suitable for the lower instrumented vertebra (LIV) in adolescent idiopathic scoliosis (AIS) correction surgery.
Methods
In total, 57 patients were included in the study following posterior instrumentation and fusion. The average follow-up period was 2.2 years. Patients were classified into 4 groups according to the relationship of the location of LIV, LTV, and the last substantially touched vertebra (LSTV) on upright radiographs and the LTV on supine radiographs. In group 1, the upright LTV and supine LTV were the same. Group 1 was subdivided into group 1A and group 1B according to whether the LTV and LSTV were different or the same, respectively. In group 2, the upright LTV was selected as the LIV, whereas in group 3, the supine LTV was selected as the LIV. The baseline characteristics and the preoperative and postoperative radiographic/clinical outcomes of the groups were analyzed.
Results
No differences were found in the preoperative clinical and radiographic baseline characteristics of the 4 groups except the LIV-central sacral vertical line distance. The immediate, 6-month, 1-year, and 2-year postoperative outcomes were not significantly different among the 4 groups. One patient (4.3%) in group 1A experienced radiographic adding-on without clinical symptoms. No patients underwent revision surgery.
Conclusion
The group in whom the LIV was selected as the LTV on supine x-rays showed similar postoperative radiographic and clinical results to other groups. The LTV on preoperative supine radiographs is acceptable as the LIV in AIS surgery to maximize motion segments.
INTRODUCTION
The most important factor influencing the postoperative results in adolescent idiopathic scoliosis (AIS) patients is the selection of the fusion level [1]. Improper selection of the fusion level can lead to under- or overcorrection of the major and compensatory curves, and may result in failure to stabilize the index curve, which can cause truncal imbalance and decompensation [2-4]. Moreover, several studies have shown that longer fusion in AIS patients results in greater functional loss and a higher incidence of disc degeneration and low back pain in a long-term follow-up [4-6]. Thus, the goal of AIS surgery is to obtain spinal balance and to prevent the adding-on (AO) phenomenon and distal junctional kyphosis (DJK), while fusing the minimum number of motion segments, expecting that the unfused curve will spontaneously accommodate to compensate for the corrected position of the fused curve.
To date, numerous studies have been conducted to identify the optimal lower instrumented vertebra (LIV) in AIS surgery, but no consensus has been reached. Matsumoto et al. [7] obtained good postoperative outcomes when the last touched vertebra (LTV), defined as the last cephalad vertebra touched by the central sacral vertical line (CSVL), was selected as the LIV. Lenke et al. [8] reported that selecting the LTV as the LIV for Lenke type 1A curves produced acceptable radiographic results at a minimum 5-year follow-up. However, in actual clinical practice, if the CSVL touches the LTV slightly, choosing the proper LIV can be challenging. Thus, Cho et al. [9] proposed the concept of the ‘‘last substantially touched’’ vertebra (LSTV), defined as the most proximal vertebra where the CSVL either intersects the pedicle outline or is medial to the pedicle outline.
Although there are several methods for selecting the optimal LIV, they do not reflect the patient's actual intraoperative status. Studies have investigated the traction x-ray under general anesthesia (TrUGA) method as a way to solve this problem [10]. However, the TrUGA method has several disadvantages. The surgical plan can be changed intraoperatively because it is not possible to make a surgical plan before surgery or general anesthesia. Furthermore, the LIV can be changed depending on the amount of muscle relaxant or intraoperative traction. The hypothesis of this study was that the LTV on supine x-rays could be the optimal LIV in most types of Lenke curves. Supine radiographs are easy to take and the curve can be reduced in a more relaxed state without gravity and weight-bearing, similarly to the intraoperative posture. In other words, supine radiographs reflect the flexibility of the curve, saving unfused motion segments that are expected to undergo compensation. Therefore, the purpose of this study was to analyze whether using the LTV on supine x-rays as the LIV could enable us to save motion segments when selecting the fusion level in AIS patients.
MATERIALS AND METHODS
This was a retrospective study of a patient series at a single academic institution. This study was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (IRB No. B-2107-695-103). The baseline characteristics and radiographic data were collected from January 2014 to March 2019. The inclusion criteria were as follows: (1) any AIS patients treated with posterior pedicle screw constructs, (2) with a minimum follow-up of 1 year. Patients with neuromuscular disease or congenital spinal deformity and those who underwent revision surgery were excluded. The demographic and surgical data were recorded, including sex, age at surgery, the curve type by Lenke classification [11], the number of fused vertebrae, the correction rate of the main curve, and the length of follow-up. To evaluate clinical outcomes, the Scoliosis Research Society (SRS)-22 questionnaire was utilized. Fifty-seven patients (14 males and 43 females) were enrolled in this study. The mean age at surgery was 16.7 years (range, 10.0–21.6 years). The average follow-up period was 2.2 years (range, 1.0–3.2 years). All patients were surgically treated by a single senior attending surgeon.
1. Radiographic Measurements
Upright posteroanterior (PA) and lateral plain radiographs, as well as supine anteroposterior (AP) radiographs of the entire spine, were obtained at 5-time points: preoperatively, immediately postoperatively, and 6 months, 1 year, and 2 years postoperatively.
Distal AO was defined as a progressive increase in the number of vertebrae included distally within the primary curve combined with either an increase of more than 3 cm in the deviation of the LIV from the CSVL or an increase of more than 10° in the angulation of the first disc below the instrumentation. DJK was defined by a distal junctional angle greater than 10° between the caudal endplate of the LIV to the caudal endplate that was one vertebra below. In this study, poor radiographic outcomes were defined as a distance > 3 cm from the CSVL to the center of the LIV, or a discal angle between LIV and LIV+1> 10° in the coronal or sagittal plane at the final follow-up.
The radiographic parameters measured included the Cobb angle of the thoracic curve (TK, thoracic kyphosis), the thoracolumbar/lumbar curve (TL/L), lumbar curve (LL, lumbar lordosis), the angulation of the first disc below the LIV, the sagittal angulation of the first disc below the LIV, the LIV-CSVL distance, and LIV tilt.
2. Grouping of Patients
Patients were categorized into 4 groups according to the relationship of the location of the LIV, LTV, and LSTV on upright plain radiographs and LTV on supine radiographs.
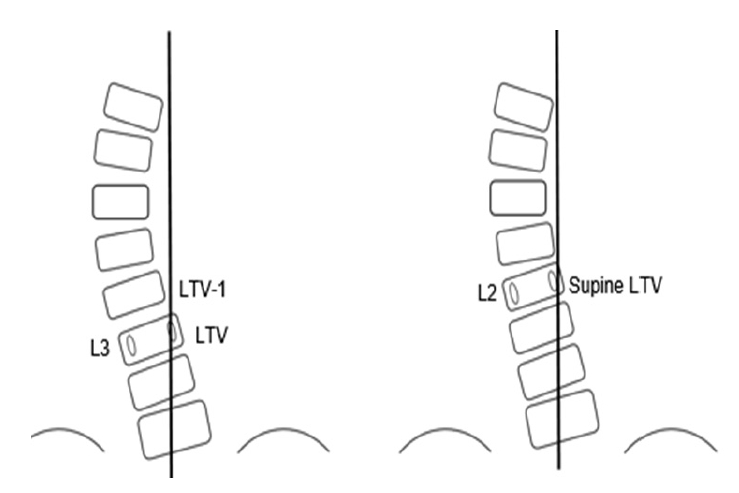
Group 1 included patients whose upright LTV and supine LTV were the same; therefore, that vertebra was selected as the LIV for corrective surgery. Group 1 was then divided into groups 1A and 1B according to the relationship between the LTV and LSTV on upright radiographs. Group 1A contained patients in whom the LTV and LSTV were different (Fig. 1), while group 1B included patients whose LTV and LSTV were the same. Groups 2 and 3 contained patients with different upright LTV and supine LTV. In group 2, patients’ upright LTV was selected as the LIV for surgery. In contrast, in group 3, the supine LTV was selected as the LIV, meaning that they had a 1-level shorter extent of instrumented fusion than group 2 (Fig. 2).
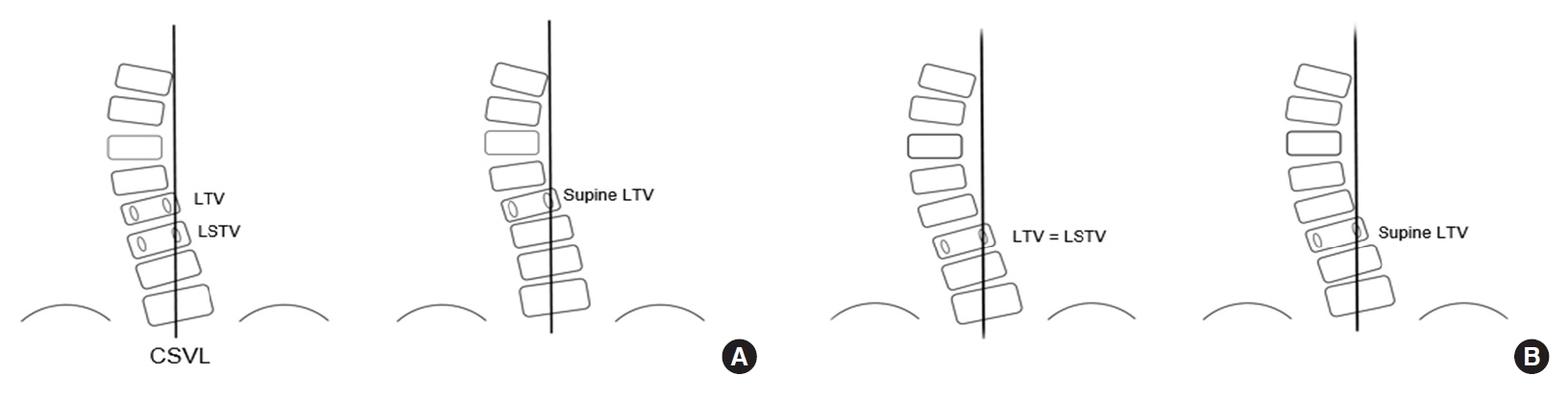
Illustration of groups 1A and 1B. The left illustration shows an upright radiograph and the right one shows a supine x-ray. (A) The last touched vertebra (LTV) and supine LTV are at the same level, but the LTV and last substantially touched vertebra (LSTV) are at different levels (group 1A). (B) The LTV, supine LTV, and LSTV are all at the same level (group 1B).
3. Statistical Analysis
All continuous variables were presented as mean±standard deviation for each group and were subjected to statistical analysis. For the 4 groups, the chi-square test and the Kruskal-Wallis H test were used to compare patient characteristics and preoperative radiographic data. The postoperative radiological and clinical outcomes of the 4 groups were compared using the Kruskal-Wallis H test. The Wilcoxon signed-rank test was used to analyze changes in clinical outcomes after the operation. A p-value of < 0.05 was considered to indicate statistical significance. Statistical analyses were performed using IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA).
RESULTS
1. Preoperative Evaluation
The distribution of the Lenke types of the 4 groups is summarized in Table 1. The clinical and radiographic baseline characteristics of the 4 groups are summarized in Table 2. No significant differences were found between the groups in terms of age, sex, TK, TL/L, LL, angulation of the first disc below the LIV, sagittal angulation of the first disc below the LIV, and LIV tilt. The LIV-CSVL distance on upright PA plain radiographs was significantly higher in group 3 than in the other groups (p<0.05) (Table 2).
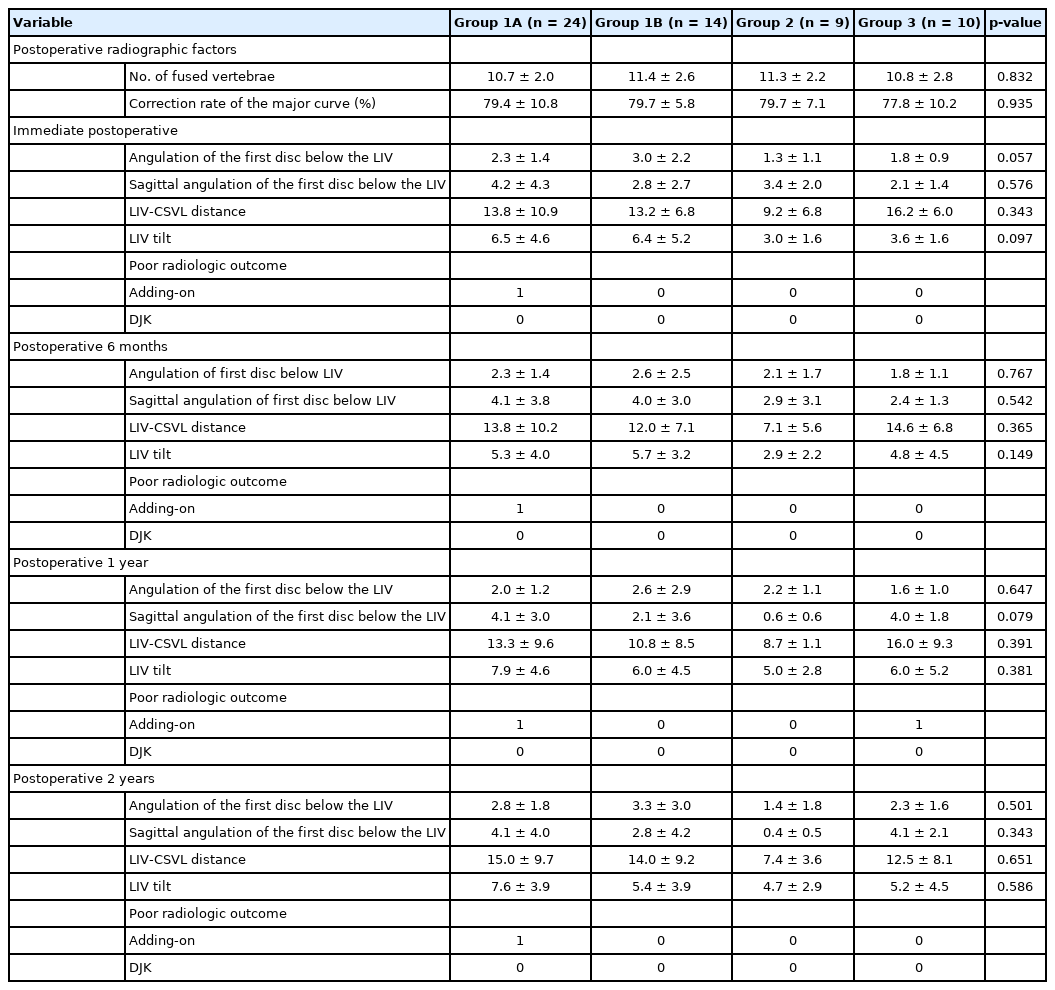
2. Postoperative Radiological Results
The mean number of fused vertebrae was 10.7±2.0 in group 1A, 11.4±2.6 in group 1B, 11.3±2.2 in group 2, and 10.8±2.8 in group 3. The correction rate of the major curve was 79.4%±10.8% in group 1A, 79.7%±5.8% in group 1B, 79.7%±7.1% in group 2, and 77.8%±10.2% in group 3. The number of fused vertebra and correction rate of the major curve were not significantly different among the groups (p=0.832 and p=0.935, respectively) (Table 2).
The radiological outcomes were not significantly different among the groups at any of the time points (Table 3). At 1 year postoperatively, 2 patients (with Lenke type 2A and 5C, respectively) were diagnosed with AO, 1 in group 1A and 1 in group 3.
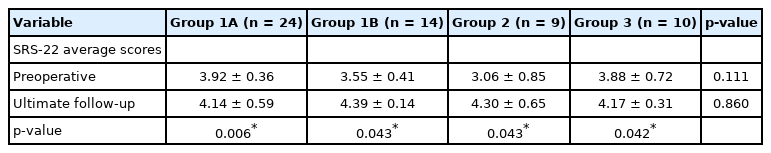
3. Clinical Outcomes
No patients underwent revision surgery. No significant differences were found in the average SRS-22 scores between the groups preoperatively and at the last follow-up (p=0.111 and p=0.860, respectively) (Table 4). All 4 groups showed significant improvement in SRS-22 average scores after surgery.
DISCUSSION
The purposes of corrective surgery for a deformity are to achieve a well-balanced spine and to prevent further progression of the deformity, while maximally preserving motion segments [4,12-15]. The selection of the LIV plays an important role in AIS correction surgery, because improper selection of the LIV leads to AO or DJK [16,17]. Numerous studies have investigated the appropriate LIV for AIS surgery, and various concepts have been introduced by previous researchers [18-26]. Previous studies with different curve types based on the Lenke classification revealed that selecting the LTV or LSTV as LIV can achieve satisfactory radiographic and clinical results [27-29]. However, in actual clinical practice, if the CSVL touches the LTV slightly (Fig. 1A), choosing the proper LTV can be challenging, and the LTV does not reflect the intraoperative prone posture that reduces the scoliotic curve due to a lower gravitational force of the body and muscle relaxation. Therefore, this study aimed to demonstrate the usefulness of supine AP plain radiographs by confirming that the postoperative outcomes following selection of the supine LTV as the LIV did not differ from those achieved when the upright LTV or LSTV was used as the LIV for AIS surgery.
In our study, we divided a total of 57 patients into 4 groups using a combination of upright and supine plain radiographs. The demographic and preoperative radiographic data were not substantially different among the 4 groups, with the exception of the preoperative LIV-CSVL distance, which was significantly higher in group 3 (28.3±4.7; p=0.001) than in other groups. This is because the supine LTV was selected as the LIV in group 3, which is 1 level proximal than other groups; therefore, the distance from the CSVL to the LIV was higher.
Our results suggest that supine x-rays can be useful for LIV selection, since the group where the supine LTV was selected as the LIV (group 3), maximally saving motion segments, did not show poorer postoperative radiographic and clinical outcomes than other groups. We summarized the occurrence of poor radiographic outcomes (e.g., AO, DJK, and proximal junctional kyphosis) at the immediately postoperative time point, as well as at postoperative 6 months, 1 year, and 2 years (Table 3). Only 2 patients showed poor radiographic outcomes, in group 1A (at the final follow-up after surgery) and group 3 (at 1 year after surgery), respectively. Interestingly, the patient in group 3 was compensated by the saved lumbar curve, and the CSVL-LIV distance improved on the 2-year radiographs. The patient in group 1A showed persistent radiographic AO, but did not undergo revision surgery because she was clinically asymptomatic. Therefore, the postoperative results of group 3, in whom the LIV was selected based on the supine x-ray, did not show inferior outcomes at the final follow-up (Fig. 3).

A representative case of group 3. (A) A 15-year-old girl with L4 touched by the central sacral vertical line (CSVL) on an upright radiograph and a LIV-CSVL distance of 26.6 mm. (B) The supine last touched vertebra (LTV) was L3 on a supine plain radiograph. Therefore, she was categorized into group 3. (C) After corrective surgery, the LIV-CSVL distance was 13.6 mm and the angulation of the first disc below the LIV was 2.3°. The patient showed good clinical outcomes at immediate postoperative period. (D) The LIV-CSVL distance was 14.7 mm and the angulation of the first disc below the LIV was 2.5° at the 2-year follow-up. Clinical outcomes were excellent at the 2-year follow-up.
Few reports have described attempts to select an optimal LIV through radiographs other than the conventional upright radiograph method. Hamzaoglu et al. [10] described the use of TrUGA to select the fusion level, and evaluated whether their fusion selection criteria based on TrUGA helped to save the L3–4 motion segment when compared with other conventional methods in patients with Lenke type 3C and 6C curves. However, the TrUGA method has several practical disadvantages. For instance, preoperative TrUGA was obtained immediately after a patient was intubated, thereby increasing the duration of surgery and anesthesia. Furthermore, the LIV can be changed depending on the amount of muscle relaxant or intraoperative posture (e.g., whether Gardner-Wells tongs and halo-femoral traction were applied). Given its similarity to patients’ intraoperative posture, supine AP plain radiographs can be an appropriate option for LIV selection.
There are several limitations of this study. The study had a retrospective design and included a relatively small number of subjects, which resulted in a low statistical power. Moreover, a relatively short follow-up period of 2.2 years is the limitation of the study. AO and DJK may occur differently between subgroups in long-term follow-up. Therefore, additional long-term follow-up studies with substantially larger populations are required to substantiate our conclusions. Another weakness of the study is that we included all curve types in the Lenke classification. Nevertheless, we suggest that selecting the supine LTV as the LIV could be acceptable. The selection criteria of the LIV have 2 categories: stopping around the TL junction around the lower end vertebra of the thoracic major curve or stopping at L3/L4 at or below the lumbar major curve. The supine LTV around the TL junction for all lumbar A or B modifiers and selective thoracic fusion of all lumbar C modifiers can be chosen as the LIV. The supine LTV around the lower lumbar spine for Lenke types 5 and 6 and nonselective thoracic fusion for all lumbar C modifiers can be chosen as the LIV.
CONCLUSION
The group in whom the LIV was selected as the LTV on supine AP plain radiograph showed similar postoperative radiographic and clinical results to those of the other groups. The LTV on preoperative supine radiograph can be an acceptable LIV in AIS surgery to maximize motion segments.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: SH, KK; Data curation: DK, SH; Formal analysis: DK; Methodology: DK, SH, CL, KK; Project administration: DK, SH; Visualization: DK, SH; Writing-original draft: DK; Writing-review & editing: DK, SH, CL, KK