Phenotypes and Prognostic Factors of Syringomyelia in Single-Center Patients With Chiari I Malformation: Moniliform Type as a Special Configuration
Article information
Abstract
Objective
The specific association between morphometric characteristics of the syrinx and the prognosis of Chiari malformation type I (CM-I) with syringomyelia following surgical procedure seems to have not been fully elaborated. This study focused on the preoperative clinical and radiologic parameters in CM-I patients with syringomyelia to find out the relationship between the patients’ clinical status and the phenotypes of the syrinx with surgical outcome.
Methods
A continuous series of pediatric and adult patients with CM-I and syringomyelia from a prospectively maintained database in a single center were included, and we explored the related factors affecting the prognosis following decompression surgery through retrospective analysis of clinical presentations, imaging characteristics, and the morphological features of syringomyelia, to provide a clinical reference for the treatment of syringomyelia.
Results
There were 28 pediatric patients (13.8%), and 174 adults (86.2%) included in our study. The average Chicago Chiari Outcome Scale score was 14.56±1.78. The overall prognosis after surgery was good in our series, among them 152 cases (75.25%) with a favorable prognosis, and syrinx was resolved effectively in 172 cases (85.15%). According to the univariate and multivariate analyses, the preoperative symptom duration, observation time, and with/without moniliform type were independent factors affecting the prognosis in adults. The most obvious difference between moniliform type and nonmoniliform type lies in the preoperative symptom duration, ventral subarachnoid space at the foramen magnum, and with/without straightened cervical physio-curve.
Conclusion
Timely decompression surgery could achieve a better outcome in CM-I patients with syringomyelia. Moniliform syringomyelia may suggest a relatively better prognosis.
INTRODUCTION
Syringomyelia is a fluid-filled cavity that originates in the tissue or central canal of the spinal cord [1,2]. That may occur secondary to various etiologies, including Chiari malformation type I (CM-I), trauma, tumor, tethered cord syndrome, or spinal arachnoiditis [3,4]. Among these, CM-I is a condition characterized by caudal displacement of the cerebellar tonsils through the foramen magnum (FM) [5]. Many hypotheses have been brought forward to explain the pathophysiological basis for the development of the syringomyelia associated with CM-I, which usually points to a gradual neurological deterioration caused by subarachnoid space (SAS) obstruction that extends over many years [4,6-8]. At present, the conclusions on the pathogenic mechanisms of the disease and related predicting factors remain inconsistent.
In recent years, with the widespread use of magnetic resonance imaging (MRI), there was an increasing number of patients screened with syringomyelia. Surgical management initially focused on treating the etiology of the syringomyelia [9], primarily by re-establishing the physiologic pathways of cerebrospinal fluid (CSF) in the SAS [10]. Mostly, the surgical goal is to reconstruct the craniovertebral junction (CVJ) with duraplasty [11]. Previous studies have suggested that early diagnosis and surgical intervention such as posterior fossa decompression (PFD) have made it possible to reduce the size of the syrinx [12]. No evidence was seen for surgical treatment of incidental asymptomatic syringomyelia, but it is recommended to treat without delay for stepwise evolutive syringomyelia, which means a severe disease with a bad impact on quality of life [13]. There have been numerous case series of pediatric and adult patients describing clinical presentation and prognosis following surgical procedure, with widely varying surgical outcomes [14-18]. Neither the extent of tonsillar herniation nor the size of the posterior cranial fossa would necessarily predict the presence or resolution of syringomyelia and surgical outcome [17,19-21]. Therefore, there may be other factors playing a role in the pathogenesis and prognosis of syringomyelia. The morphometric characteristics of the syrinx in CM-I patients may contain different parameters, such as the size, length, configuration, and deviation of the syrinx, while the specific association between morphometric characteristics of syrinx with the prognosis seems to have not been elaborated.
In the present study, a continuous series of CM-I patients with syringomyelia from a single center were included. We explored the related factors affecting the prognosis of neurological function through retrospective analysis of clinical presentations, imaging characteristics, and the morphological features of syringomyelia, to provide a clinical reference for improving the prognosis.
MATERIALS AND METHODS
1. Patient Selection
From January 2017 to December 2020, a consecutive series of CM-I patients with syringomyelia were retrospectively reviewed in a single institution. Clinical records and radiologic data in this study were retrospectively analyzed from a prospectively maintained syringomyelia database. According to screening, a total of 202 pediatric and adult CM-I patients with syringomyelia who underwent PFD finally met the inclusion criteria of our study.
Inclusion criteria: (1) CM-I with syringomyelia, with MRI showing cerebellar tonsils more than 5 mm below the FM; (2) patients underwent PFD with duraplasty in our center.
Exclusion criteria: (1) patients with atlantoaxial dislocation, basilar invagination, congenital vertebral anomalies, degenerative cervical spondylosis, tumor, trauma, myelomeningocele, or tethered cord; (2) secondary CM-I due to hydrocephalus or intracranial space-occupying lesions; (3) a history of CVJ surgery with cervical or occipital fusion and instrumentation; (4) incomplete clinical data or lost follow-up after surgery.
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Xuanwu Hospital, Capital Medical University University (No. 2018027). We obtained consent from all patients participating in this study.
2. Clinical Evaluation
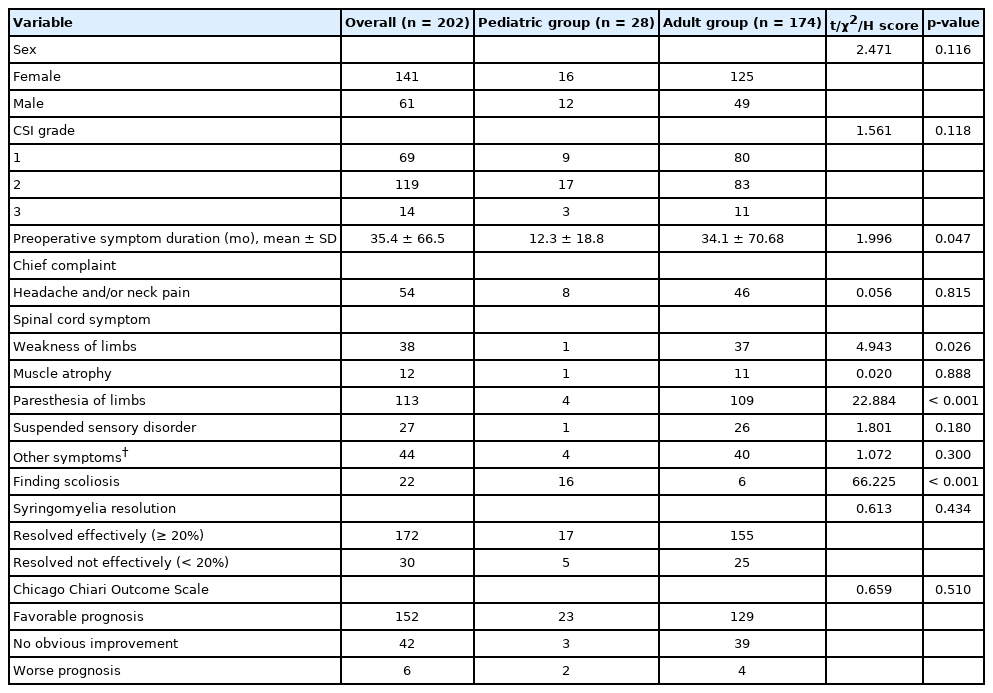
Clinical symptoms were divided into general symptoms, spinal cord-related symptoms such as suspended sensory disorder, amyotrophy and weakness of limbs, and other symptoms such as cerebellar syndrome and cranial nerve dysfunction. Some patients had multiple clinical symptoms at the same time. The Chiari Severity Index (CSI), a preoperative grading system proposed by Greenberg et al. [22] was used to assess the preoperative status of each patient. The specific data were summarized in Table 1.
3. Radiographic Evaluation
Preoperative x-rays were measured using the CAD Canvas X (ver. 20.0; Canvas GFX, Boston, MA, USA), a computer-aided drafting software. All relative radiologic measurements were repeated at least 3 times, independently by one surgeon and another radiologist. We could determine whether there was obvious scoliosis (Cobb angle of main curve ≥ 10° in the coronal x-ray). The value of cervical Cobb angle in the sagittal plane at the range of -5° to 5° was defined as the straight cervical spine, and the positive value larger than this range was defined as the lordosis; the negative value lower as the kyphosis.
RadiAnt DICOM Viewer software (ver. 4.6.9, Medixant, Poznan, Poland) was used to view and measure MRI images. A routine MRI examination was taken within 1 week before surgery. Postoperative MRI was conducted regularly on a 1 month, 3 months (± 1 month), 6 months (± 3 month), 1 year, 1.5 years basis, and later every year after decompression surgery until evidence for effective syrinx resolution was found. The following indicators were measured at the T2-weighted median sagittal and transverse positions of MRI: (1) maximal syrinx/cord (S/C) ratio: the ratio of syrinx diameter to the spinal cord diameter at the same level. (2) syrinx length: the number of vertebral segments spanned by the syrinx. (3) A radiographic improvement rate in the maximal S/C ratio or syrinx length was calculated using the following formula: (preoperative value–postoperative value)/preoperative value. Furthermore, we assessed the following angles that related to the CVJ region and posterior cranial fossa: basal angle, the angle of the tentorium cerebelli to the Twining line, clivo-axial angle, clivus gradient, and ventral and dorsal SAS at FM on median sagittal MRI (Supplementary Fig. 1)
4. Operation Strategy
Operation reports were reviewed including 202 patients who underwent PFD with duraplasty and C1 laminectomy. The posterior arch of the C1 (1.5 cm on each side) and the FM (1.5 cm on each side, about 3 cm upwards) were resected until the dura mater transition at the cerebellar hemisphere was seen. After incision of the dura mater, the arachnoid was opened for further exploration of the fourth ventricle outlet.
5. Prognostic Evaluation
Immediate postoperative outcomes were evaluated at discharge. Long-term follow-up was defined as the last available follow-up that was more than 6 months after surgery.
The Chicago Chiari Outcome Scale (CCOS) was used to evaluate the surgical efficacy from 4 aspects: pain symptoms, nonpain symptoms, functionality, and complications, with a score from 1 to 4 for each item [23]. The better the prognosis, the higher the score, with the CCOS score groupings (4–8, 9–12, 13–16) presenting the prognosis as favorable between 13 and 16, no obvious improvement between 9 and 12, and worse between 4 and 8. The latter 2 groups (4–12) were defined as having no improvement.
6. Variable Definition
The preoperative symptom duration was defined as the time from the onset of symptoms to the initial diagnosis of syringomyelia at admission to our institution. Observation time represented the time from the indication for surgery determined (with syringomyelia confirmed by MRI, but the patient refused surgery) to decompression surgery. The postoperative syrinx was reported to be either reduced (syrinx decreased in size ≥ 20%) or unchanged (syrinx decreased in size less than 20% or remained the same size). The event of significant improvement of syrinx was defined as a more than 20% decrease in maximal S/C ratio on follow-up MRI.
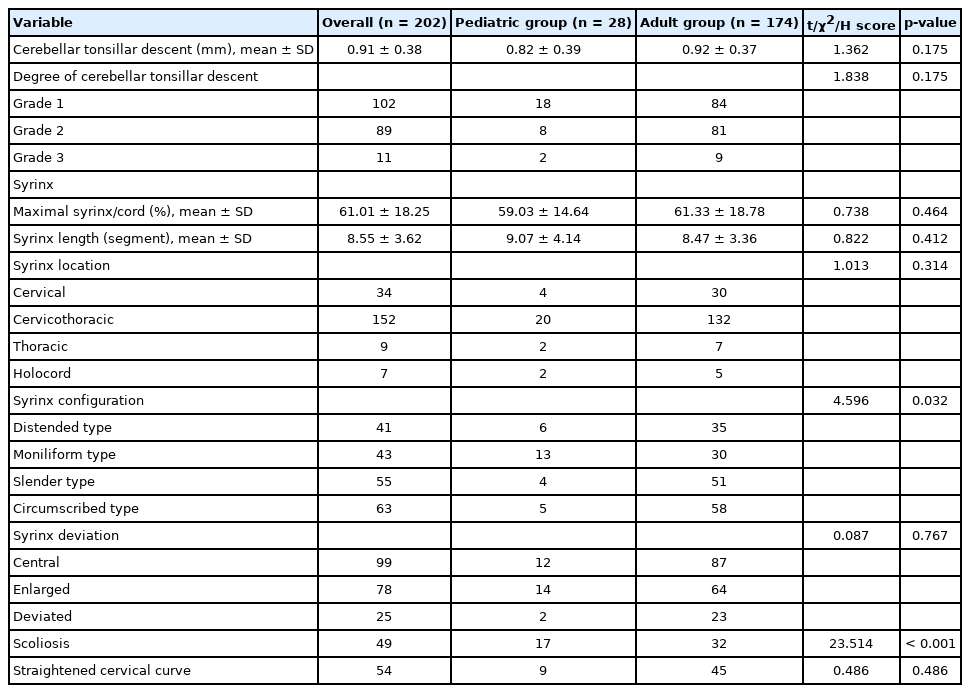
As previously proposed by Ono et al. [24], the configuration of syrinx can be divided into 4 types: A, distended type; B, moniliform type; C, slender type; D, circumscribed type (Fig. 1). Syrinx with continuous septations (≥ 3) was referred to as moniliform type. The preoperative degree of cerebellar tonsillar descent was divided into 3 stages: grade 1, the cerebellar tonsil descends beyond the FM but does not reach the C1 arch; grade 2, reaches the C1 arch; grade 3, descends beyond the C1 arch.
The configuration of the syrinx in the adult group (A–D) and pediatric group (E–G). It can be divided into 4 types: distended type (A, E); moniliform type (B, F); slender type (C, G); circumscribed type (D, H). The arrows of panels B and F means continuous separation located inside the moniliform syringomyelia.
7. Statistical Analysis
IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis. For continuous variables, the mean values are presented with standard deviations, and the differences between the 2 groups were analyzed using the Student t-test. A chi-square or Fisher exact test was used to assess associations between dichotomous categorical variables. The Kruskal-Wallis H test was used for multiple categorical variables. A p-value of < 0.05 was considered statistically significant. Intraclass correlation coefficient (ICC) was used to evaluate the intrarepeatability of different observers (interobserver reliability). One independent researcher blinded to the group allocation completed the evaluations.
RESULTS
1. Patient Characteristics
A total of 202 CM-I patients with syringomyelia were admitted to a single center between January 2017 and December 2020. There were 28 cases (13.8%) younger than 18 years old, including 16 females (57.1%) and 12 males (42.9%) with a mean age of 7.8±4.1 years (range, 1.0–17.0 years) in the pediatric group. There were 71.8% females and 28.2% males with a mean age of 47.4±10.4 years (range, 23.0–73.0 years) in the adult group. Compared with the adult group, the pediatric group showed a much lower incidence of paresthesia of limbs and a proportion of patients who suffered weakness of limbs. There was quite a high incidence of scoliosis in children than in adults. A longer clinical presentation was seen in the adult group (Table 1).
At admission, the mean maximal S/C of the syrinx was 0.61±0.18 (ICC=0.911) and the mean syrinx length (vertebral segments) was 8.55±3.62 (ICC=0.924). The difference was not seen in syrinx location, syrinx deviation, and cervical physio-curve. There was no significant difference in CSI and degree of cerebellar tonsillar descent between the 2 groups. Moniliform type was more common in children than adults (Table 2).
2. Surgical Outcome
The average CCOS score was 14.56±1.78 points. The overall postoperative prognosis was good, among all the patients, 152 cases (75.25%) with a favorable prognosis, and 50 cases (24.75%) were without improvement. There was no significant difference in the prognosis evaluated by CCOS and effective resolution of syrinx between the 2 groups. Syrinx was resolved effectively in 172 cases (85.15%), and 30 cases (14.85%) stayed unchangeable or worsened in terms of syrinx resolution.
No serious neurologic complications occurred in the 2 groups of patients. There were 7 cases (3.5%) with postoperative transient headache, 9 cases (4.5%) with short-term CSF leakage, and 4 cases (1.5%) with incisional infection.
3. Factors Predicting the Surgical Outcome in the Adult Group
The preoperative clinical parameters and radiologic measurements from the 174 adult patients were assessed using univariate and multivariate analyses to identify factors for predicting clinical improvement (composite CCOS) following surgery (Table 3).

Factors predicting composite CCOS improvement using univariate and multivariate logistic regression models in adults
The primary univariate test showed that longer preoperative syndrome duration (p<0.001) and longer observation time (p<0.001) were associated with a statistically significant increase in the likelihood of no improvement. In addition, moniliform type (p=0.008) and syrinx length (p=0.002) were also significant predictors of clinical improvement (composite CCOS). However, CSI, degree of cerebellar tonsillar descent, CVJ parameters including basal angle, clivo-axial angle, and clivus gradient, or any other factors were not associated with prognosis.
Through further multivariate analysis, it was found that preoperative syndrome duration, observation time, and with/without moniliform type were independent factors affecting the prognosis. The receiver operating characteristic (ROC) curve suggested that the preoperative syndrome duration predicted the clinical improvement (composite CCOS) with high accuracy (area under the curve=87.1%, p<0.001) (Fig. 2).
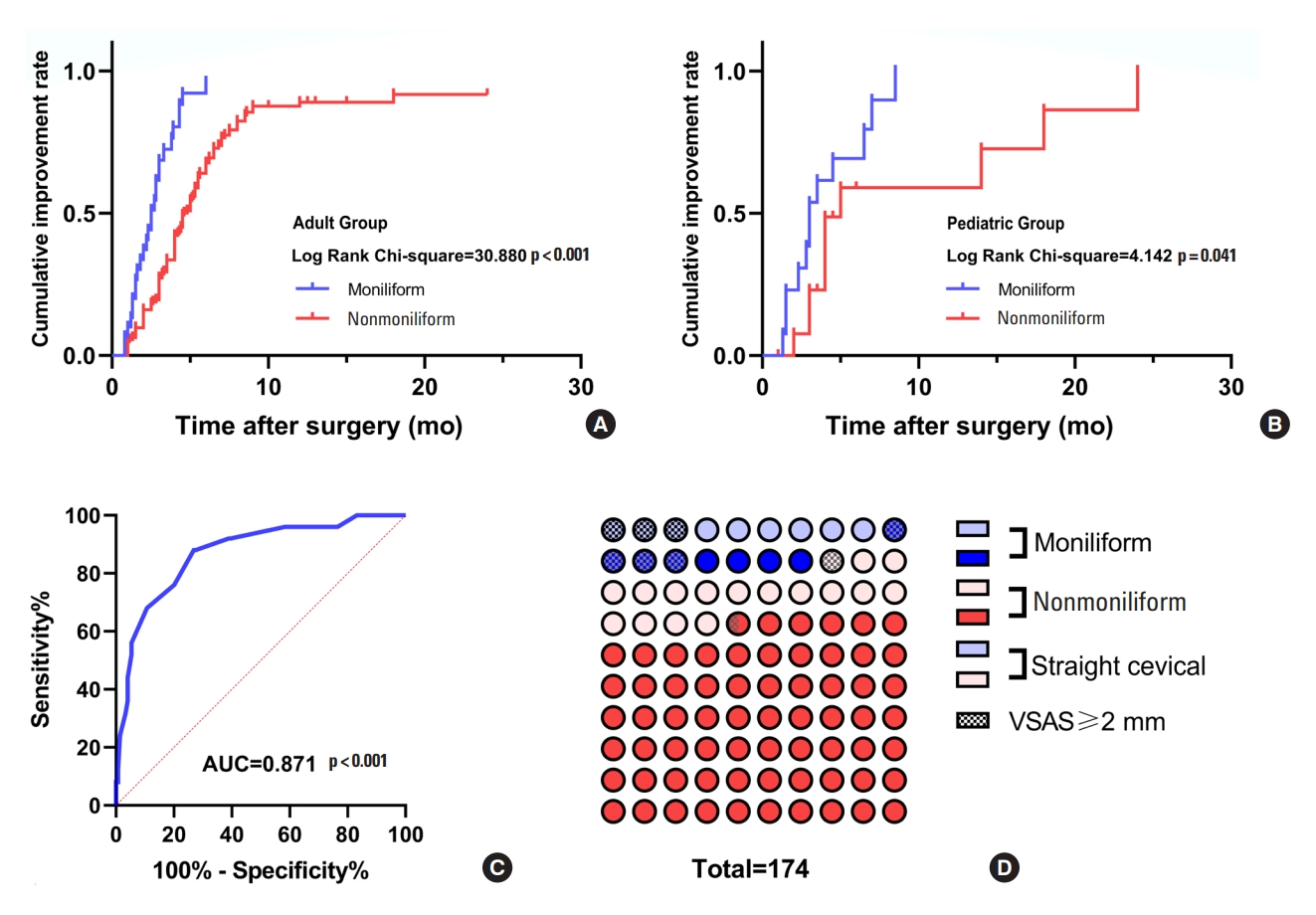
The analysis curves and graphs about independent influencing factors affecting prognosis. A Kaplan-Meier analysis demonstrated the cumulative incidence rate of effective syrinx resolution between moniliform and nonmoniliform in adults (A) and children (B). The receiver operating characteristic curve suggested that the preoperative symptom duration predicted the composite Chicago Chiari Outcome Scale improvement with high accuracy (area under the curve [AUC]=87.1%; p<0.001) in adults. (C) The percentage dot plot illustrated that the proportion of the moniliform type, and (D)its relative factors such as straight cervical spine and ventral subarachnoid space ≥ 2 mm. VSAS, ventral subarachnoid space.
A Kaplan-Meier analysis demonstrated the cumulative incidence rate of effective syrinx resolution. The effectiveness of syrinx resolution in patients with moniliform type was significantly higher than that with the nonmoniliform type (p<0.001 by log-rank test) in the adult group. It was seen that pediatric patients with moniliform type could also achieve better syrinx resolution (p=0.042 by log-rank test) (Fig. 2).
4. Differences Between Moniliform Type and Nonmoniliform Type
The most obvious difference between moniliform type and nonmoniliform type lies in the preoperative symptom duration (p=0.029), ventral SAS at the FM (p<0.001), and the patients with straightened cervical physio-curve or not (p<0.001) (Table 4).
DISCUSSION
Due to CM-I often associated with other CVJ malformations, there are inevitably some confounding factors that make the evaluation criteria of CM-I inconsistent [25]. Moreover, children and adults share different clinical courses, not only for the natural history but also the postoperative prognosis. Our study focused on the preoperative clinical and radiologic parameters in simple CM-I patients with syringomyelia to find out the relationship between the clinical status of the patients and the morphometrical characteristics of the syrinx with surgical outcome.
1. Differences Between Pediatric and Adult Patients With CM-I and Syringomyelia
It is considered that children are still in the stage of growth and development. In a subset of pediatric patients with Chiari malformation without surgical treatment, the syringomyelia could even resolve spontaneously at follow-up [26]. According to comparisons of the preoperative clinical and radiologic characteristics in our continuous series of patients between adults and children, it was illustrated that the main difference lies in the duration of preoperative symptoms. What’s more, children often found CM-I with syringomyelia on further workup due to scoliosis. In adults, syringomyelia is mostly diagnosed when weakness or paresthesia of limbs occurs. All patients in the 2 groups completed the operation successfully, and there was no perioperative death or serious fatal complications.
Improvements in syringomyelia-related symptoms, however, do not always correspond to reductions in the size of the syrinx [27,28], so we analyzed both syrinx resolution and CCOS score respectively to comprehensively assess the surgical outcomes. The prognosis of both groups was generally favorable, no significant differences existed in the syrinx resolution and clinical outcomes between the 2 groups. Through further comparisons of radiologic parameters, it was found that syrinx in moniliform type was more common in children, which may be related to the relatively shorter natural history of CM-I in the pediatric group. There were no statistically significant differences in other baseline factors. It is unknown whether the more frequent occurrence of the moniliform syrinx in children is due to the high compensation of syringomyelia in pediatric CM-I. If so, it is necessary to further include phenotypic factors of syringomyelia in adults to analyze its association with prognosis through multivariate analysis.
2. Univariate and Multivariate Logistic Regression Models in Adult Patients
By reviewing the natural history of CM-I in children and adults, combined with the comparison between the 2 groups of cases in this series (children vs. adults), it is suggested to further explore the relevant factors affecting the prognosis in adult patients, and whether it is related to the specificity of typical moniliform type.
Firstly, through univariate analysis in adults, we concluded that preoperative syndrome duration (p<0.001), observation time (p<0.001), the length of the syrinx (p=0.002), and with/without moniliform type (p=0.008) were related factors affecting the prognosis. Next, the multivariate analysis illustrated that the duration of preoperative symptoms, observation time before surgery, and with/without moniliform type were independent prognostic factors. Moreover, the effectiveness of syrinx resolution in patients with moniliform type was significantly higher than that with nonmoniliform type.
Appropriate time of intervention for syringomyelia was important [19,29]. The shorter the preoperative symptom duration and the shorter the observation time for decompression surgery, the better the prognosis. Timely decompression surgery could achieve a better outcome, which was reflected in a higher CCOS score and syrinx resolution rate. The ROC curve also illustrated the duration of preoperative symptoms to guide prognosis with high accuracy. Therefore, surgical decompression should be taken as soon as possible once the indication for surgery is determined, which is beneficial to improving the prognosis. According to the natural history of the occurrence and development of syringomyelia, timely surgical intervention for the moniliform syringomyelia may allow patients to obtain better surgical efficacy, which would be discussed further in the following text.
There was a paucity of detailed studies on the relationship between prognosis after decompression surgery and syringomyelia morphology, which contained syrinx length, width, configuration, and deviation [30-32]. Syrinx configuration has rarely been regarded as predicting factors in previous studies. Our results confirmed that most factors above were not involved in predicting surgical outcomes. The syrinx length was only a related factor, rather than an independent factor affecting the prognosis. However, we interestingly found that the CCOS score improvement in syrinx with moniliform type was relatively better than that with nonmoniliform type.
3. The Particularity of Syringomyelia With Moniliform Type
Why does syrinx with moniliform type show better prognostic improvement? Does the formation of moniliform syrinx indicate some kind of protective mechanism, or bring about some inspiration in the clinical diagnosis and treatment of the syringomyelia-related disease? The clinical prognosis of syringomyelia in moniliform type is relatively better, simultaneously with higher effectiveness of syrinx resolution shown by the survival curve in both pediatric and adult groups (Fig. 2). On the one hand, this may be related to the relatively short duration of its natural history, on the other hand, such syrinx may have strong compensatory effects for decompression surgery. During the postoperative follow-up, we found that the moniliform syringomyelia tended to move towards a smaller S/C, but the intrinsic separation of the syringomyelia appeared to persist in the short period after surgery (Figs. 3, 4). In terms of imaging characteristics, its continuous separation located inside the syrinx may be the source of the highly compensatory pathophysiological mechanism of such syringomyelia [33].
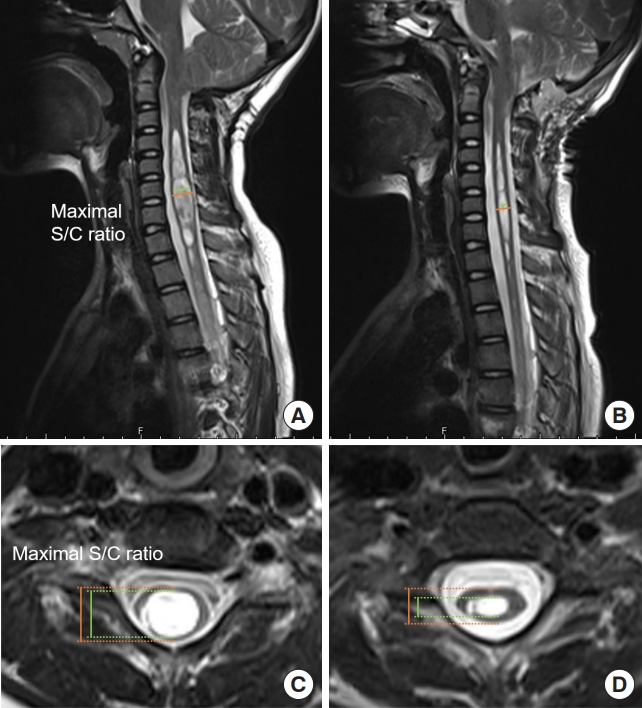
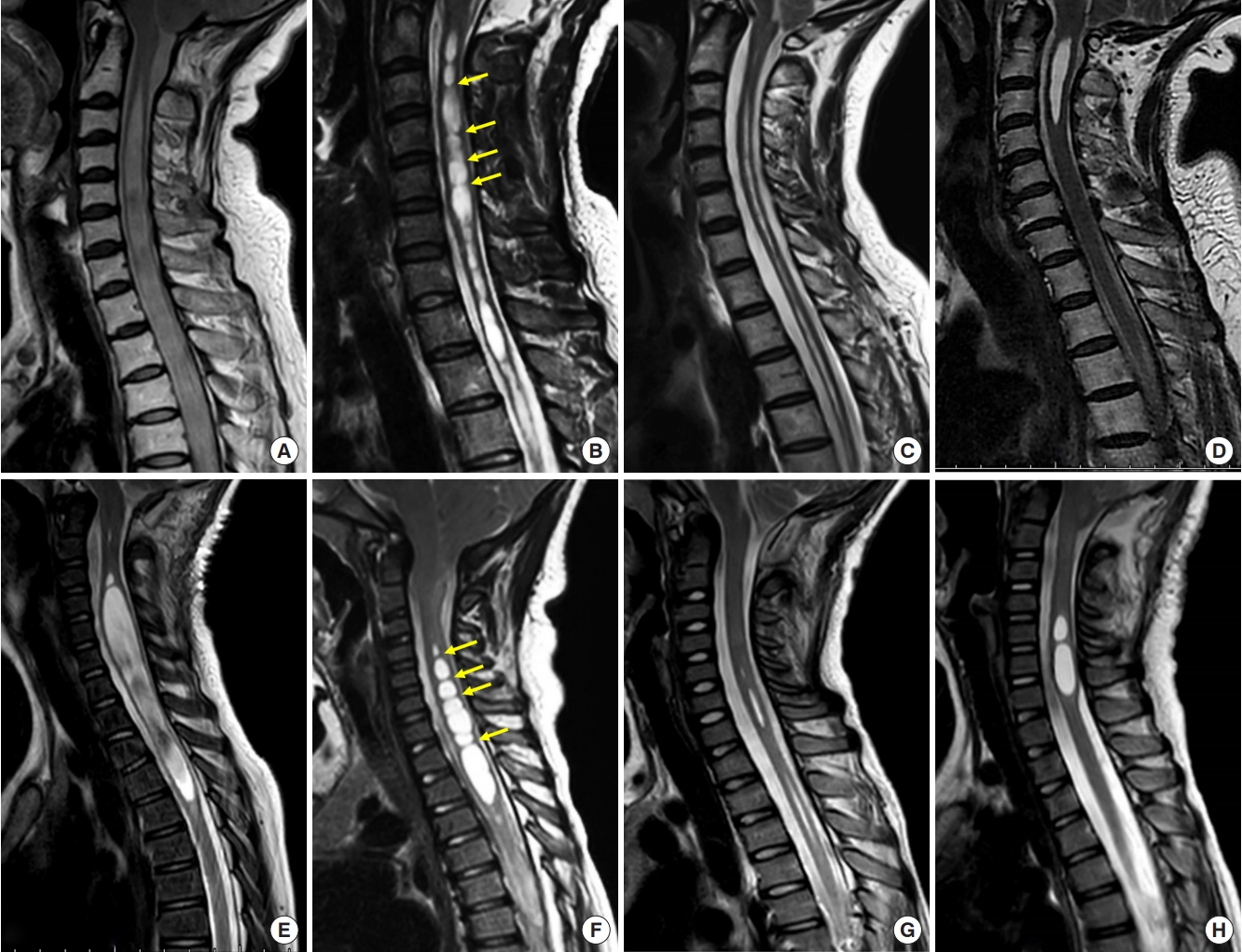
A 10-year-old girl with Chiari I malformation and moniliform syringomyelia. (A, C) Preoperative magnetic resonance images showed a syrinx with a maximal syrinx/cord (S/C) ratio of 0.844 and a length of 14 vertebral segments. (B, D) The 3-month postoperative magnetic resonance imaging showed that the S/C ratio had decreased to 0.637, and the length of the syrinx had decreased to 7 vertebral segments.
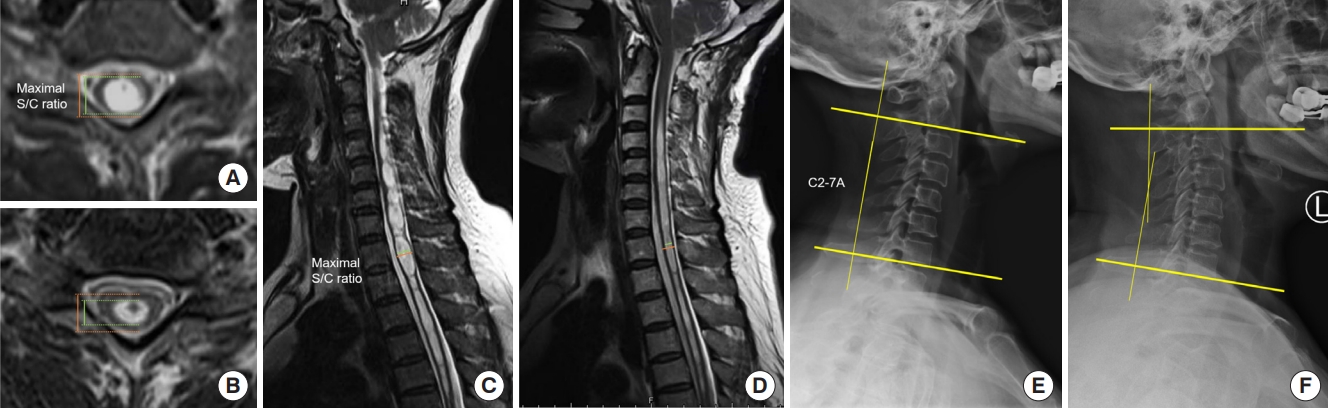
A 55-year-old female with Chiari malformation type I and moniliform syringomyelia. (A, C) Preoperative magnetic resonance imaging (MRI) showed a syrinx with a maximal syrinx/cord (S/C) ratio of 0.847. (B, D) The 3-month postoperative MRI showed that the S/C ratio had decreased to 0.594. (E) Preoperative x-ray showed a straightened cervical physio-curve with the Cobb angle of -1.2°, but (F) she recovered to the normal cervical lordosis during syrinx resolution after surgery.
From the point of the association among cerebellar tonsillar herniation, CSF circulation obstruction, and syringomyelia, we agreed that syringomyelia generally underwent a dynamic process: presyringomyelia stage, progressive stage, and stable stage [34]. We further analyzed the differences of various factors at baseline between moniliform type and nonmoniliform type syringomyelia and tried to trace the particularity from the origin and development of the moniliform syringomyelia. Such configuration tends to have a shorter duration of preoperative symptoms, and ventral SAS ≥2 mm is more concentrated in this type, suggesting that a moniliform type may represent the morphological feature in the early course of the disease. Because the cerebellar tonsillar herniation obstructs the circulation of CSF at the FM (especially in dorsal SAS), ventral SAS ≥ 2 mm was more common in the moniliform type group, which could be derived from some “buffer space” in the ventral SAS in the early stage.
Moreover, straightened cervical physio-curve appears to be more common in patients with moniliform syrinx than nonmoniliform syrinx. Some scholars have previously reported that compared with normal people, patients with syringomyelia will have a certain loss in cervical lordosis, but they have not mentioned the intrinsic relationship between the specific syringomyelia type and the corresponding changes in cervical sagittal alignment [35]. We speculated that the compensatory decrease in cervical lordosis during syringomyelia formation may act as a compensatory physiological response to get better CSF circulation in the SAS. This mechanism may be more pronounced in the moniliform syrinx. With the syrinx resolution after surgery, the lordosis may have a certain tendency to recover (Fig. 4), but that still needs to be confirmed by more randomized controlled trials.
4. Clinical Significance of This Study
The results in this study did not show that other factors such as CSI, degree of cerebellar tonsillar descent, CVJ measurements, the presence or absence of scoliosis, and cervical physio-curve were directly related to clinical prognosis, nor did it show a difference in these factors between the moniliform and nonmoniliform syringomyelia. Although they may be relevant factors that need to be comprehensively considered before surgery, they had no obvious predictive significance for guiding prognosis. However, CM-I often accompanies other CVJ malformations, and it is difficult to identify the prognosis through only one single index. It must be analyzed on a case-by-case basis combined with other comprehensive factors.
This paper proposes a special morphological feature of syringomyelia, the moniliform type syringomyelia, associated with the surgical outcome from the perspective of clinical symptoms, imaging features (phenotypes of syringomyelia and biomechanical structures of the CVJ and cervical spine), and multivariate prognostic analysis. Based on the previous studies [24], we give a new definition for this type of syringomyelia, that is moniliform syrinx with continuous obvious separation on MRI, which presents as a wide ventral SAS at FM, and tends to have a relatively shorter natural history and more common straightened cervical curve, and most importantly it may suggest a better prognosis. In the future, more clinical research is needed to dynamically observe the change of syringomyelia from the perspective of the pathophysiological mechanism of the occurrence and development of syringomyelia, finally to make clear the structure and function of syringomyelia separation and the biological characteristics of moniliform syringomyelia.
5. Strengths and Limitations
Moniliform type was elicited based on clinical and radiographic comparisons between different age groups. It was confirmed that such type may have an impact on the prognosis in adults, which was assessed using both syrinx resolution and CCOS. Finally, the particularity of moniliform syringomyelia was analyzed.
However, it was undeniable that there were some shortcomings in our study. The survival curve was analyzed based on the event of the effective resolution of the syrinx by postoperative MRI, so a short time interval was selected as much as possible, but there was still interval error, for example, the occurrence of the event happened to fall within the empty period between the checkpoints. Besides, there was a lack of longer follow-up after the effective resolution of the syringomyelia, so more research and evaluations are needed in the future to achieve the maximal ablation effect of the syringomyelia.
CONCLUSION
Timely decompression surgery could achieve a better outcome in CM-I patients with syringomyelia. The moniliform syringomyelia with representative syrinx separations may suggest a relatively better prognosis. That provides more insight into the pathophysiological mechanism during the dynamic progression of syringomyelia to find the intrinsic protection strategy from the clinical experience.
SUPPLEMENTARY MATERIALS
Supplementary Material: Supplementary Fig. 1 can be found via https://doi.org/10.14245/ns.2244332.166.
Measurements of craniovertebral junction (CVJ) and posterior cranial fossa (PCF): basal angle (BA), the angle of the tentorium cerebelli to the Twining line (TTA), clivo-axial angle (CAA), clivus gradient (Cl-Gr), Ventral subarachnoid space (VSAS) and dorsal subarachnoid space (DSAS) at foramen magnum (FM), and tonsillar herniation (TH) on median sagittal magnetic resonance imaging. (A) Schematic diagram of the mechanism demonstration in our speculation about the relationship among the syrinx, cerebrospinal fluid (CSF) circulation, imaging factors of CVJ, PCF, and cervical spine. (B) The wider subarachnoid space at FM and the loss of cervical lordosis may both help to ensure the CSF circulation.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study was supported by Beijing Municipal Natural Science Foundation (grant number: L212007).
Author Contribution
Conceptualization: FJ; Data curation: CL, LM, CY, LC, XW, WD, KW, ZC, HW, GZ; Formal analysis: CL, LM, CY, LC, ZC, HW, FJ; Methodology: CL, LM, CY, XW, WD, KW, Z Chen, GZ, FJ; Project administration: GZ, FJ; Visualization: LM, CY, LC, WD, KW, Z Chen, HW, GZ, FJ; Writing - original draft: CL, FJ; Writing - review & editing: CL, FJ.