Surgical Outcome of a Zero-profile Device Comparing with Stand-alone Cage and Anterior Cervical Plate with Iliac Bone Graft in the Anterior Cervical Discectomy and Fusion
Article information
Abstract
Objective
A Zero-profile device is a cervical stand-alone cage with integrated segmental fixation device. We characteristically evaluated the radiological changes as well as clinical outcomes in the application of Zero-profile devices compared with stand-alone cages and anterior cervical plates with iliac bone grafts for the cervical disease.
Methods
Retrospectively, total 60 patients at least more than one year follow-up were enrolled. Twenty patients were treated with Zero-profile devices (Group A), twenty patients with stand-alone cages (Group B) and twenty patients with anterior cervical plates and iliac bone grafts (Group C) for a single level cervical disease. The clinical outcomes were evaluated by Odom's criteria and Bazaz-Yoo dysphagia index. The radiologic parameters were by subsidence and the changes of the midpoint interbody height (IBH), the segmental kyphotic angle (SKA), the overall kyphotic angle (OKA) in index level.
Results
Although there was no significant clinical difference according to the Odom's criteria among them(p=0.766), post-operative dysphagia was significantly decreased in the Group A and B compared with the Group C (p=0.04). From the immediate postoperative to the last follow-up time, the mean change of IBH decrement and SKA increment were significant in the Group B compared with the Group A (p=0.025, p=0.033) and the Group C (p=0.001, p=0.000). The subsidence rate was not significant among all groups (p=0.338).
Conclusion
This Zero-profile device is a valuable alternative to the anterior cervical discectomy and fusion with a low incidence of postoperative dysphagia and without segmental kyphotic change.
INTRODUCTION
Smith and Robinson's technique had been the "gold standard" for the surgical treatment of cervical disc disease36). However, anterior cervical plates with iliac bone grafts may be associated with higher.
postoperative chronic iliac pain14,35) and higher rates of dysphagia10,11,19,30,39). For those reasons, stand-alone cervical cages have also been used to avoid these complications. The polyethyletherketone (PEEK) cage has good biomechanical properties and reduces the stress shielding effects. It is also easy to determine the cervical interbody fusion radiologically. However, the problems of cages are known as increasing subsidence and loss of cervical lordosis11,39). These results led to the development of a stand-alone cage with integrated fixation device for Zero-profile segmental stabilization (Synthes GmbH Swithzerland, Oberdorf, Switzerland).
Many authors reported that the clinical outcomes between the stand-alone cages and the anterior cervical plates for cervical disc disease were similar13,16,17,33). There are some articles about the Zero-profile devices3,4,8,12,15,18,23,24,29) or focusing dysphagia in the anterior cervical discectomy and fusion3,34,41). Some authors found the Zero-profile devices have lower incidence of dysphagia compared with titanium plate and cage29,34,41). However, we limit its use because of National Health Insurance allowance at the moment.
In addition, there is no direct comparative research about clinical and radiological outcomes among three groups, as far as we know: Zero-profile devices, stand-alone cages, and anterior cervical plates with iliac bone grafts for the cervical disease. Here, we wrote this paper to compare the clinical and radiological outcomes among them.
MATERIALS AND METHODS
1. Patients
Retrospectively, we evaluated total sixty patients treated with a single level ACDF from January 2008 to June 2013 in a retrograde order. The demographic findings of the patients were summarized (Table 1). They were divided into three groups; Zero-profile devices in group A (n=20), standalone PEEK cages in group B (n=20) and cervical anterior plates with autologous iliac bone grafts in group C (n=20). The average follow-up durations of the group A, group B and group C were 13.2 months, 13.1 months and 13.6 months, respectively.
The inclusion criteria were; (1) signs and symptoms of cervical radiculopathy or cervical spondylotic myelopathy which was unresponsive to the conservative treatment, (2) single level disease confirmed by clinical symptom and imaging (Computed tomography scan or Magnetic resonance imaging), (3) complete continuous clinical and imaging data. The exclusion criteria were; (1) history of previous cervical spine surgery, (2) others cervical diseases, including infection, tumor, deformity or ossification of posterior longitudinal ligament, (3) requirement for simultaneous anterior and posterior surgery, or hybrid surgery.
2. Operative Techniques
All operative procedures were performed by one neurosurgeon. A standard anterior Smith approach was performed. After removing the disc material, the cartilage endplates were scraped with a curette and high speed electric drill. The posterior osteophytes were removed by Kerrison punches. Once neural decompression was performed, the height, length and depth were measured of the discectomy level. For fusion bed, milling procedure was performed with diamond drill. The patients were reconstructed with three different methods.
In the Group A, the interbody fusion was performed with Zero-profile devices with four screws were tightened into the adjacent cervical bony segment (Fig. 1A). In the Group B, the inter-body fusion was carried out with PEEK cages (Fig. 1B). The DBM was filled into the cage for fusion in the Group A and B. In the Group C, the inter-body fusion was accomplished with anterior cervical titanium plates and autologous tri-cortical iliac bone grafts fixed by four screws (Fig. 1C). We advised all patients to use of a cervical collar for a month after the surgery.
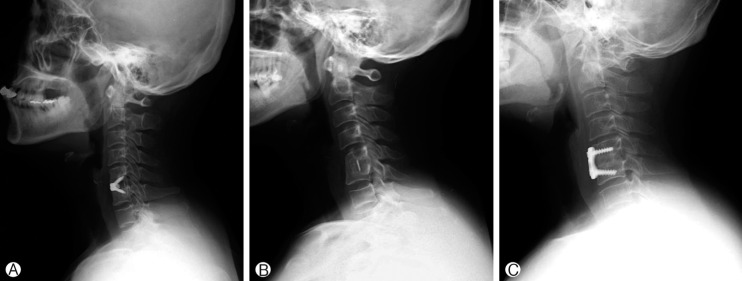
(A) Post-operative radiographs showing the Zero-profile device for a single level cervical disease. (B) Post-operative radiographs showing stand-alone cage for a single level cervical disease. (C) Post-operative radiographs showing anterior cervical plate with autologous bone graft for a single level cervical disease.
3. Clinical Evaluation
Clinical outcome was evaluated according to the Odom's criteria. These criteria provide the healthy status and daily activities limitations. Patients were rated as excellent, good, fair and poor. Excellent state is all preoperative symptoms relieved and abnormal findings improved; Good state is minimal persistence of preoperative symptoms; Fair state is definite relief of some preoperative symptoms, but other symptoms unchanged or slightly improved; Poor state is symptoms and signs unchanged or exacerbated. Furthermore, postoperative dysphagia and chronic donor site pain were observed.
Incidence of dysphagia-related symptom was recorded using the system defined by Bazaz6). Severity of dysphagia was graded as none, mild, moderate or severe (Table 2).
4. Radiological evaluation
Three radiographic parameters were estimated at the preoperative, the immediate postoperative and the last follow-up time (range: 12-15 months), finally. The lateral plain radiographs of the cervical spine were used for the measurement of the midpoint interbody height (IBH), the segmental kyphotic angle (SKA) and the overall kyphotic angle (OKA) in index level.
The IBH is defined as the distance between the midpoint of the superior end plate of upper vertebra and inferior end plate of lower vertebra of the affected segments. The SKA (α) is defined as the angle between the superior end plate of the upper vertebra and the inferior end plate of the lower vertebra of the affected segment. The OKA (β) is defined as the angle between the inferior endplate of C2 and the inferior endplate of C7 (Fig. 2).
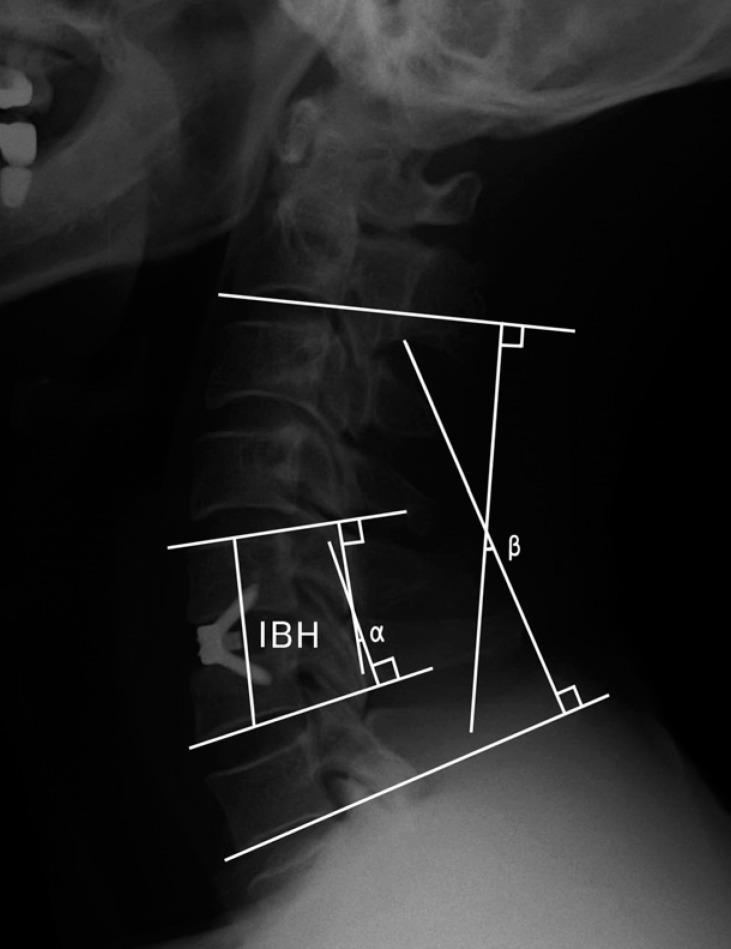
Postoperative radiographs illustrating the interbody height (IBH), the segmental kyphotic angle (SKA=α), and the overall kyphotic angle (OKA=β).
Postoperative subsidence was defined as any settlement in the disc height of at least 3 mm on the lateral radiographs16).
5. Statistical Analysis
Statistical analysis was achieved using SPSS for Mac (version 20.0, SPSS Inc, Chicago, IL, USA). Clinical and Radiological interval changes of subgroups were analyzed using the ANOVA test, Chi-Square test, Mann-Whitney U-test and Wilcoxon signed rank test. The statistical significance was defined as p<0.05.
RESULTS
1. Clinical Outcome
Postoperatively, the majority of patients of all groups were good or excellent according to the Odom's criteria. There was no significant difference among them(p=0.766) (Table 3).
One (5.0%) patient complained of mild dysphagia 2 weeks after surgery in the Group A and B, however, the dysphagia disappeared after 2 months. There were six (30%) patients complained of dysphagia in the Group C. Four patients complained of mild dysphagia 2 weeks after surgery. Two patients complained of moderate dysphagia 2 months after surgery. After conservative treatment, such as oromotor fascilitation and feeding training, five patients had recovered after 2 months and one patient recovered after 6 months. The incidence of dysphagia of Group A and B was lower than Group C (p= 0.040) (Table 4).
2. Radiological Outcome
1) Zero-profile Devices
In the Zero-profile devices group, the immediate postoperative IBH was increased compared with the preoperative time and then decreased at the last follow-up time (p=0.000, p=0.000), respectively. However, the mean IBH was increased from the preoperative to the last follow-up time (p=0.000). The immediate postoperative SKA was decreased compared with the preoperative time and then increased at the time of the last follow-up (p=0.001, p=0.000), respectively. However, the mean SKA was decreased from the preoperative to the last follow-up time (p=0.000). There were no significant interval changes of OKA as time goes on (Table 5).
2) Stand-alone Cages
In the stand-alone cages group, the immediate postoperative IBH was increased compared with preoperative time and then decreased at the last follow-up time (p=0.000, p=0.000), respectively. However, the mean IBH was decreased from the preoperative to the last follow-up time (p=0.000). The immediate postoperative SKA was decreased compared with the preoperative time and then increased at the time of the last follow-up (p=0.004, p=0.007), respectively. However, the mean SKA was increased from the preoperative to the last follow-up time (p=0.011). There were no significant changes of OKA in process of time (Table 5).
3) Anterior Cervical Plates with Autologous Iliac Bone Grafts
In the anterior cervical plates with autologous iliac bone graft group, the immediate postoperative IBH was increased compared with the preoperative time and then decreased at the last follow-up time (p=0.000, p=0.000), respectively. However, the mean IBH was somewhat decreased from the preoperative to the last follow-up time (p=0.000). The immediate postoperative SKA was decreased compared with the preoperative time and then somewhat increased at the time of the last follow-up (p=0.001, p=0.000), respectively. However, the mean SKA was decreased from the preoperative to the last follow-OKA as time as time goes by(Table 5).
4) Zero-profile Devices Versus Stand-alone Cages
The change of IBH showed significantly more decreased in the Group B than the Group A from the immediate postoperative to the last follow-up time and from the preoperative to the last follow-up time (p=0.025, p=0.000), respectively. The change of SKA showed significantly more increased in the Group B than the Group A from the immediate postoperative to the last follow-up time and from the preoperative to the last follow up time (p=0.033, p=0.025), respectively. The change of OKA showed significantly more increased in the Group B than the Group A from the preoperative to the last follow-up time (p=0.044) (Table 6).
5) Stand-alone Cages Versus Anterior Cervical Plates with Autologous Iliac Bone Grafts
The change of IBH was significantly more decreased in the Group C than the Group B from the preoperative to the immediate postoperative time (p=0.036). However, it was significantly more decreased in the Group B than the Group C from the immediate postoperative to the last follow-up time (p=0.001).
The change of SKA showed significantly more increased in the Group B than the Group C from the immediate postoperative to the last follow-up time and from the preoperative to the last follow-up time (p=0.000, p=0.006), respectively. However, there was no significant difference of OKA between them(Table 6).
6) Zero-profile Devices Versus Anterior Cervical Plates with Autologous Iliac Bone Grafts
The change of IBH was significantly more increased in the Group A than the Group C from the preoperative to the immediate postoperative time and from the preoperative to the last follow-up time (p=0.001, p=0.004), respectively. However, there was no significant difference of SKA and OKA between them (Table 6).
DISCUSSION
Degenerative conditions of the cervical disease are commonly treated by discectomy and subsequent interbody fusion. ACDF is the gold standard for the surgical management at the present. Although the cervical total arthroplasty is possible operative techniques25,32,40), the inclusion criteria are somewhat limited2). On the ACDF, the biomechanical stability is mandatory7,9,28,30,42).
Various types of cages have been used to perform ACDF, including titanium, carbon fiber reinforced polymer (CFRP), and polyetheretherketone (PEEK) cages. The radiolucent PEEK cages have superior biomechanical properties and a similar elastic coefficient to that of human bone, as well as a reduced stress shielding effect, which reduces the bone weakness and increases the fusion rate. However, graft extrusion was reported as 2% on the average. In our study, there was no graft extrusion, nor screw loosening.
Generally, anterior cervical plates using various interbody grafts enhance stabilizing properties and increase fusionrates1,12,22,31,47). However, this procedure using anterior plates is associated with various intraoperative and postoperative complications, especially dysphagia. It also demands iliac bone harvest which causes chronic iliac site pain5,37,38). Studies have demonstrated that the chronic pain rate can still be 18.7%, two years after iliac crest surgery14,35). Three patients (15%) of our Group C complained of chronic postoperative donor site pain. The incidence was lower than the previous other study14,35).
Meanwhile, the cervical stand-alone cage with integrated fixation for the Zero-profile segmental fixation devices has four screws for internal screw fixation and a one-step locking mechanism. This device is made of radiolucent PEEK polymer and has a radio-opaque titanium alloy plate to verify placement. This Zero-profile device acts as a stand-alone device for use in cervical interbody fusion4,8,12,15,18,23,24). Its design combines the functionality of a cervical interbody spacer and the benefits of an anterior cervical plate which limits the risk of damage to adjacent organs like vessels, soft tissues or nerves. Biomechanical testing has shown the stability of the Zero-profile device to be similar to that of established anterior cervical plate with cage34).
Many authors reported that the clinical outcomes between the stand-alone cage and the anterior cervical plate for cervical disc disease were similar13,16,17,33). This current study including Zero-profile devices found that there was no significant clinical difference for a single level cervical disease among them (Group A, B and C) according to the Odom's criteria (Table 3).
In ACDF, a common complication is chronic dysphagia with a general incidence of around 3-21% before the Zeroprofile devices era10,30). Wang et al.41) found that only one of twenty two patients (4.5%) using Zero-profile device and eight of the twenty five patients (32%) using anterior cervical titanium plate and cage complained of dysphagia. Azab et al.3) reported that 39 of 75 patients (76%) using Zero-profile device had mild dysphagia with symptom duration of 17±9 days. At 6 weeks' follow-up, 8 patients (10.5%) complained of mild dysphagia which resolved completely by 3 months in all of them.
Although the exact pathophysiologic mechanism of dysphagia after ACDF remains unknown, Lee et al.21) reported that dysphagia was related to the thickness of the titanium plate at the level of fusion. Fountas et al.10) explained postoperative dysphagia due to soft tissue edema, hematoma, esophageal injury and adhesion formations around implanted cervical plates. This Zero-profile device can be completely contained in the decompressed intervertebral space, avoiding the mechanical stimulus to the esophagus and other pre-vertebral soft tissues41). It may lessen the incidence of the dysphagia. In addition, the Zero-profile device is not placed across the anterior vertebral body, which reduces the dissection of pre-vertebral soft tissues and preserves as many normal anatomical tissues as possible41).
This study showed that the dysphagia incidence of Group A and Group B was 5%, respectively, while that of Group C was 20% in the early postoperative period and 10% in the medium period (Table 4).
After conservative treatment, five patients had recovered after 2 months and one patient recovered after 5 months. Our dysphagia incidence was consistent with other studies34,41).
On the other hand, the radiologic change of IBH and SKA of all groups had similar pattern as time passes. That is, the immediate postoperative IBH was increased from the preoperative time and then decreased at the time of the last follow-up (p=0.000 and p=0.000 in Group A, B and C), and the immediate postoperative SKA was decreased from the preoperative time and then increased at the time of the last follow-up (p=0.001 and p=0.000 in the Group A, p=0.004 and p=0.007 in Group B, p=0.001 and p=0.000 in Group C) (Table 5). However, they did not affect the OKA change as time passes (Table 5).
From the immediate postoperative to the last follow-up time, the change of IBH showed significantly more decreased in the Group B compared with the Group A and Group C (p=0.025, p=0.001), respectively. In addition, from the immediate postoperative to the last follow-up time, the change of SKA showed significantly more increased in the Group B compared with the Group A and Group C (p=0.033, p=0.000), respectively (Table 6). However, they all did not affect OKA among them(Table 6).
We think the radiologic comparison of intergroup at the preoperative time was not meaningful because of preoperative individual difference. What we want to highlight is the interval changes of each radiologic parameter.
Interbody subsidence and loss of cervical lordosis are important problems of cages as well11,39).
Many studies reported that subsidence rate varies between 23.4-50.5%27,44). There has been reported the risk factors associated with subsidence. Nonsurgical risk factors are obesity, bone mineral density and smoking, while surgical factors were anteroposterior diameter of cage and intraoperative distraction46). However subsidence does not always result in poor prognosis or aggravation of symptoms, and mostly does not cause symptoms or morbidity33,43,45). In this study, the incidence of subsidence was 50.0% in the Group A, 70.0% in Group B, and 45.0% in Group C. There was no statistical significance among them between Group A and Group C(p=0.338) (Table 7).
In cases of subsidence, we frequently observed the final fusion was formed with some segmental kyphotic change that did not cause secondary symptom. They did not have to require re-operation.
However, the radiologic summation effect of IBH or subsidence20) and kyphotic change should be considered in multi-level procedure or kyphosis anticipated. For example, the anterior cervical plate with cage or autologous iliac bone graft has been known as the most preferable choice. However, selection of the Zero-profile devices may be suitable as well considering its similar radiologic result with anterior cervical plate and iliac bone graft group.
We performed computerized tomography (CT) scans to evaluate fusion in five patients of the Group A in twelve months after the operation that showed definitely bridging bone formation within the cage and around the cages at (Fig. 3). However measuring the distance between the tips of the spinous processes at the surgically treated level in flexion-extension lateral plain x-ray is most reliable and strict method for evaluating spine fusion apart from CT scan.

Coronal cervical CT scan of a patient with Zero-profile device on the C6/7 level illustrating bridging bone formation.
Although different cervical levels in this study may be pointed out the problems, we observed just the change of IBH, SKA and OKA by time period. Therefore, we think that their radiographic analysis was not influenced by the levels. The pitfalls of this study were followings; Firstly, small number of patients. Secondly, Zero-profile device has been used lately. Thirdly, we did not demonstrate fusion rate among them. Therefore, these short points may have our results be biased.
CONCLUSION
There was no significant difference according to the Odom's criteria in a single level cervical disease among three groups. However, the incidence of dysphagia is significantly lower in the Zero-profile device and stand-alone cage group compared with anterior cervical plate and iliac bone graft group(p=0.040). Naturally, the Zero-profile devices and stand-alone cage need not iliac bone harvest. The Zero-profile device group has similar radiologic result with anterior cervical plate and iliac bone graft group. Although, prospective randomized trials with more patients and longer follow-up in the Zeroprofile device are necessary to confirm its pros and cons, surgeon should select the prime device in the light of patients.






