Influence of Alendronate and Endplate Degeneration to Single Level Posterior Lumbar Spinal Interbody Fusion
Article information
Abstract
Objective
Using alendronate after spinal fusion is a controversial issue due to the inhibition of osteoclast mediated bone resorption. In addition, there are an increasing number of reports that the endplate degeneration influences the lumbar spinal fusion. The object of this retrospective controlled study was to evaluate how the endplate degeneration and the bisphosphonate medication influence the spinal fusion through radiographic evaluation.
Methods
In this study, 44 patients who underwent single-level posterior lumbar interbody fusion (PLIF) using cage were examined from April 2007 to March 2009. All patients had been diagnosed as osteoporosis and would be recommended for alendronate medication. Endplate degeneration is categorized by the Modic changes. The solid fusion is defined if there was bridging bone between the vertebral bodies, either within or external to the cage on the plain X-ray and if there is less than 5° of angular difference in dynamic X-ray.
Results
In alendronate group, fusion was achieved in 66.7% compared to 73.9% in control group (no medication). Alendronate did not influence the fusion rate of PLIF. However, there was the statistical difference of fusion rate between the endplate degeneration group and the group without endplate degeneration. A total of 52.4% of fusion rate was seen in the endplate degeneration group compared to 91.3% in the group without endplate degeneration. The endplate degeneration suppresses the fusion process of PLIF.
Conclusion
Alendronate does not influence the fusion process in osteoporotic patients. The endplate degeneration decreases the fusion rate.
INTRODUCTION
Alendronate medication has been the standard treatment for patients with osteoporosis2,24). Alendronate binds to resorption surfaces of the bone and is locally released during acidification, and the rise in concentration stops resorption and membrane ruffling without destroying the osteoclasts23). Alendronate altered the density distributions, thereby decreasing the area with a high fracture risk, resulting in increased vertebral strength7). Despite these good effects on treating osteoporosis, using alendronate after spinal fusion is the controversial issue due to the inhibition of osteoclast mediated bone resorption. Many in vitro studies show the negative effect of alendronate to the lumbar spinal interbody fusion6,9,13). However, recent prospective randomized control studies showed that alendronate overcame its detrimental biological effect on the healing process of spinal fusion 18. The endplate degeneration of the lumbar spine has been thought as the source of back pain, but it also influenced the lumbar spinal fusion12). Signal intensity changes of vertebral endplates and subchondral bone are often observed in magnetic resonance imaging (MRI) in patients with spinal degenerative diseases. In 1988, Modic et al.16,17) summarized these changes and classified them into three types, and then Modic changes (MC), as a medical term, were used in the studies on spinal degenerative diseases. Although the etiology of MC remains poorly understood, some progress has been achieved in basic research during the past two decades, including studies of the prevalence and some clinical significance.
What if there is the endplate degeneration at the fusion level, would activity of osteoclast increase or decrease to influence the fusion process? If the activity of osteoclast increase than is it reasonable to give alendronate to patient by expecting the inhibiting effect of osteoclast? If the activity of osteoclast decrease than is it harmful for giving alendronate to the patient?
The object of this retrospective study was to evaluate how the endplate degeneration and the alendronate medication influence the fusion rate of osteoporotic patient through radiographic evaluation.
MATERIALS AND METHODS
1. Patient Population
In this study, 44 patients who underwent single-level lumbar interbody fusion using cage were examined from April 2007 to March 2009. Nine patients were male and thirty-five patients were female. The patients' mean age was 64.7 years (range 60-74 years). The patients were diagnosed as degenerative spondylolisthesis, isthmic spondylolisthesis, severe intracanal stenosis, foraminal stenosis, and recurred herniated intervertebral disc (HIVD). The minimum X-ray follow up period was 2 years (range 2-5 years) and the mean follow up period was 33.8 months.
All patients were diagnosed as osteoporosis using computed tomography (CT) bone densitometry and recommended for pharmacological treatment. The diagnosis of osteoporosis was made according to the World Health Organization. Patients were divided into the alendronate group (alendronate sodium [Fosamax] 35mg/week) or the control group. The control group was classified as patients who were not taking alendronate for less than 1 week due to poor economic conditions and gastrointestinal trouble. Compared to the previous study18), we did not give vitamin D, calcium supplement, and any other medication for osteoporosis to the control group. The mean preoperative lumbar spine BMC and T-score were 63.76mg/cc and -3.75 in the alendronate group, and 69.58mg/cc and -3.98 in the control group. There was no statistical difference between age and BMC, and between the control and alendronate group.
2. Radiographic Assessment
Endplate degeneration is categorized by the Modic classification16,17). Modic change type 1 [hypo-intense signal in T1-weighted imaging (T1WI) and hyperintense signal in T2-weighted imaging (T2WI)] is corresponding to the vertebral body edema and hyper-vascularity. MC type 2 (hyperintense signal in T1WI and hyperintense signal in T2WI) is reflecting fatty replacements of the red bone marrow. MC type 3 (hypointense signal in T1WI and hypointense signal in T2WI) was consisted of subchondral bone sclerosis.
The plain static radiographs were examined by two different neurosurgeons. They were interpreted as demonstrating the presence of fusion if there was a bridging bone between the vertebral bodies either within or external to the cage22). Fig. 1A shows a typical radiograph assessed as demonstrating a solid fusion. Fig. 1B shows the features of a pseudarthrosis with discontinuity in the bone graft and lucency adjacent to the cage.
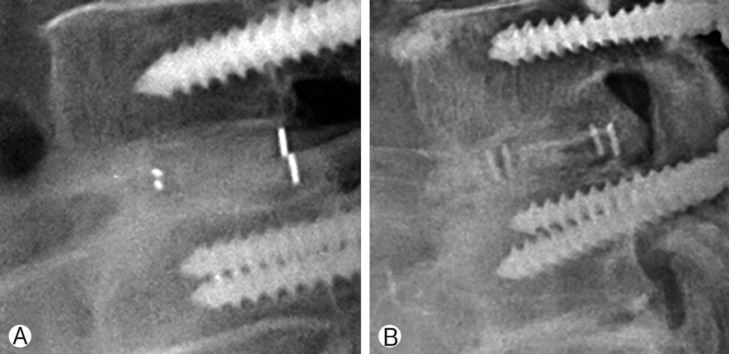
(A) Plain static radiograph interpreted as a successful fusion. (B) Plain static radiograph interpreted as a non-fusion.
The flexion radiographs were taken with the patient in the standing position trying to bend forward as far as possible, whereas the extension radiographs were taken with the patient maximally arching his or her back. The spinal surgeon used the method advocated by Simmons15), which involved identifying two landmarks on the anterior portion of the superior and inferior vertebral bodies, drawing a line through these landmarks, and measuring the angle subtended by the two resulting lines. An increase of 2° in the acute angle made by these two lines on extension views was considered to be a sign of nonunion. The apparent fusion rate was also determined using this same method, except that the 5° cutoff prescribed by the United States Food and Drug Administration (FDA) was used.
RESULTS
The chi-square test was used to determine whether there is a significant difference between two groups in Fig. 2 to 6. The p value (<0.01) was used to test statistical significance of evidence. The SPSS21(Statistical Package for the Social Sciences 21.0) was used to analyzed. Overall, 75% of fusion rate was seen and 25% of non-fusion rate was seen. In alendronate group, fusion was achieved in 66.7% compared to 73.9% in control group (no medication) (Fig. 2). There was no statistical difference between the two groups (p=0.599). Alendronate seems to have no effect on the fusion rate.

Fusion rate of the group with alendronate medication and the group with no-medication. In alendronate group, fusion was achieved in 66.7% compared to 73.9% in control group (no medication). There was no statistical difference between the two groups (p=0.599).
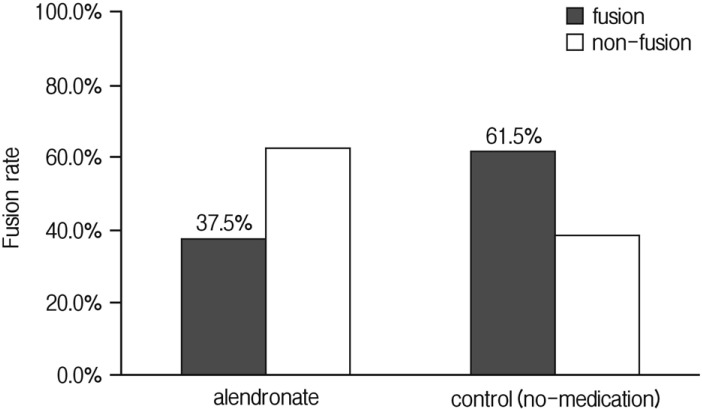
Fusion rate of the group with Endplate degeneration (with Modic change). In alendronate group fusion was achieved in 37.5% of patients. In control group fusion was achieved in 61.5% of patients. There was no statistical difference between two groups (p=0.284).
The endplate degeneration was classified by Modic16,17). A total of 52.4% of fusion rate was seen in the endplate degeneration group compared to 91.3% in the group without endplate degeneration (Fig. 3). There was a statistical difference of fusion rate between the endplate degeneration group and the group without endplate degeneration (p=0.599). Endplate degeneration decreases the fusion rate in PLIF. However, subtypes of MC do not influence the fusion rate. There was no statistical difference of fusion rate between the MC types (p=0.293) (Fig. 4).
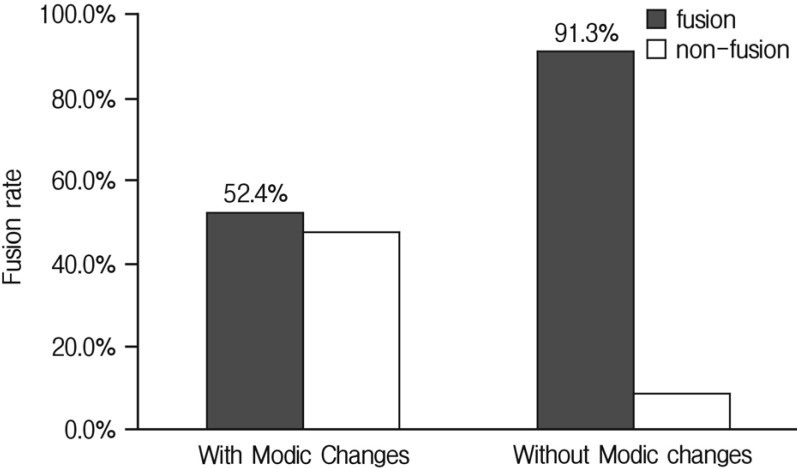
Fusion rate in the group with Modic changes and without Modic changes. 52.4% of fusion rate was seen in the Modic changes group compared to 91.3% in the group without Modic changes. There was a statistical difference between the two groups (p=0.004).
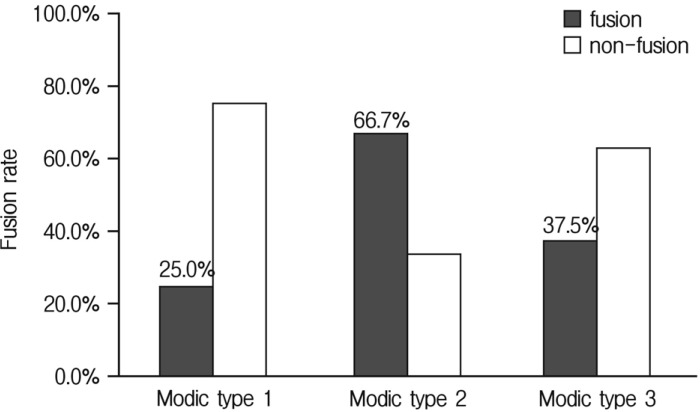
Influence of Modic changes type to fusion rate. There was no statistical difference of fusion rate between Modic change types (p=0.293).
Comparison of alendronate effect on patient without endplate degeneration shows in Fig. 5. In alendronate group fusion was achieved in 92.3% of patients. In control group fusion was achieved in 90% of patients. There was no statistical difference between two groups (p=0.846). Alendronate did not influence the fusion rate of patients without endplate degeneration. Among patients with endplate degeneration fusion was achieved in 37.5% of patients in alendronate group. In control group fusion was achieved in 61.5% of patients (Fig. 6). There was no statistical difference between two groups (p =0.284). Alendronate seems to have no effect on the fusion rate of the group with endplate degeneration.
DISCUSSION
The skeleton is a dynamic tissue that could remodel and repair the constant mirocracks that develop both in the cancellous bone and in the cortical bone for a lifetime8). It had been assumed that the mechanisms of bone remodeling were likely to be different in cancellous versus cortical bone8). Specifically, the assumption was that the cells needed for bone remodeling traveled directly from the red marrow to the bone surfaces in cancellous bone, whereas they accessed cortical bone via the vasculature20).
The successful spinal surgery is depending on gaining the long-stand spinal stability. Because of the spinal instrumentation gives short-term support, the solid bony fusion is necessary to obtain permanent stability. Coordination between bone formation and resorption is very important for spinal fusion.
The evaluation of factors that influence the lumbar spinal interbody fusion is very difficult to assess due to the complexity of biomechanics of each patient and difference in bone quality. Effects of spinal biomechanics are hard to quantify, whereas the bone quality can be easily measured by using bone densitometry and differentiated by using MRI according to Modic16,17). Most of spine surgeons believe that osteoporosisrelated bone fragility is the primary reason for implant fixation failure11), and it leads to fusion Failure4,14).
Both osteoporosis and MC related spinal fusion rate has been known to be low compared to normal or osteopenic patients12,18). The only available human study shows osteoporosis and alendronate influence the spinal fusion rate18). This study demonstrates a solid fusion was achieved in 95% of patients in the alendronate group, and 65% of those in the control group18). Most animal studies1,3,5,13,19,21,26,27,28,29) evaluating the impact of bisphosphonates on fusion rate have not found statistically significant changes with treatment, although this fact may be attributable to low statistical power. The animal literature does suggest that bisphosphonate therapy results in a less histologically mature fusion mass; however, the impact of these changes on fusion mass biomechanics is unclear. There are many studies about the endplate degeneration correlating with the symptoms, but few studies report a correlation between MC and spinal fusion. Kwon12) shows that the bony fusion rate was 97% in patients without degeneration and 83% in patients with MC. The bony fusion rate in each group was 81% in type 1, 84% in type 2, and 55% in type 3. The clinical success and fusion rates were significantly lower in patients with type 3 degeneration12).
Generally accepted fusion rate of lumbar spine is around 85-95%10). In our study, the overall fusion rate was 75%. Since half of the patients had MC in lumbar spine endplate, which could lower the fusion rate, fusion rate of our study could be acceptable.
We reviewed the osteoporotic patients into two groups. The fusion rate of the alendronate group was 76.2% compared to 73.9% of the control group. There was no statistical difference between the alendronate group and the control group. This result refutes the previous prospective randomized controlled study18). From this result we could speculate that alendronate does not alter fusion rate in osteoporotic patients.
We reviewed the patients into endplate degeneration and without the degeneration groups. A total of 42.9% of non-fusion rate was seen in the endplate degeneration group, compared to 8.7% in the group without endplate degeneration. There was the statistical difference of fusion rate between the endplate degeneration group and the group without endplate degeneration. Endplate degeneration had potential to decrease the lumbar interbody fusion. We also compared the fusion rate of endplate degeneration by MC. There was no statistical difference of fusion rate between MC. The degeneration itself influenced the fusion rate, but there was no difference between fusion rates of the MC subtypes. Small sample size and surgical technique might influence the outcome. Most of the spinal surgeons use endplate decortications technique, a process of making microfracture of fusion bed, during lumbar interbody fusion. This process would eliminate the cortical bone and sclerotic endplate degeneration, such as MC type 3, to making bone marrow surface in fusion bed. However, endplate degeneration seems to influence the biological environment for those osteoclasts and osteoblasts. The limitation of this result is that the thickness of sclerotic endplate had not been measured. The thicker at the endplate sclerosis, the harder to make good fusion bed.
We also put both factors, alendronate and endplate degeneration, together to see how these factors influence the fusion rate of the lumbar spine. The effects of alendronate on osteoporotic patient with and without MC show that alendronate did not influence the fusion rate of patients whether patients had a MC or not.
The limitation of this study was that despite the wide use of flexion-extension radiography, the definition of a solid fusion still remains controversial. In the radiologic assessment of interbody fusion using carbon fiber cages, the use of plain radiographs and flexion-extension radiographs produced much higher fusion rates than assessment with thin-section helical computed tomography scans25). The thin-section helical computed tomography studies demonstrated the radiographic presence or absence of bridging bone, a property that was not seen with plain static radiographs or flexion-extension radiographs22). Another limitation is the biomechanical loads on fusion level that could not be measured in number due to different lifestyle of each patient, such as jobs.
Finally, we still have several questions to be answered in future research: (1) How long should patients take bisphosphonates before and after spinal fusion surgery to improve the strength of vertebral bodies? (2) Could the current findings in a single-level posterior lumbar interbody fusion be applied to other situations, including multi-level spinal fusion, or correction of spinal deformities? (3) How will different types of spinal fusion, especially posterolateral lumbar fusion, affect the fusion process under alendronate medication? (4) Does bridging bone under alendronate treatment have sufficient mechanical properties and bone quality?
CONCLUSION
This study showed that alendronate does not influence the fusion process in osteoporotic patients. The endplate degeneration decreases the fusion rate, even though there was no difference in the MC subtypes. With the presence of endplate degeneration, alendronate does not influence the fusion rate in osteoporotic patients.
The effect of alendronate medication after the single level PLIF still remained unknown. The decortication technique is more important than medication in endplate degeneration at the fusion site.
