Spinal Paraganglioma Adherent to the Cauda Equina
Article information
Abstract
Paragangliomas are rare among intradural spinal tumors. Most of them are benign, but aggressive behavior and local recurrence can occur. Cases of paraganglioma are, difficult to diagnose radiologically; hence, diagnosis is confirmed histopathologically. Radiologically, paragangliomas are similar to ependymomas, and, histopathologically, they are similar to neuroendocrine tumors. We evaluated the case of a 76-year-old woman with a spinal paraganglioma that was associated with back pain and radiating pain in both the lower extremities. She underwent an operation, and her symptoms were relieved. Here, we describe a rare case of paraganglioma that was adherent to the cauda equina.
INTRODUCTION
Paragangliomas are rare among intradural spinal tumors. Most of them occur on the periphery of the cauda equina. Radiologically, they are similar to ependymomas, and histopathologically, they are similar to neuroendocrine tumors. Most of them are non-secreting tumors, although they are of sympathetic origin. Back pain is the most common symptom, and they are not associated with tachycardia, flushing, or hypertension. The treatment of choice is total surgical resection, and no additional treatment is needed with total resection. Most of them are benign, but, recurrence can occur in cases involving a failure of the total resection. Radiotherapy may be needed in cases of incomplete removal and recurrence. We describe a rare case of a paraganglioma that was adherent to the cauda equina that presented with low back pain and radiating pain in both the lower extremities.
CASE REPORT
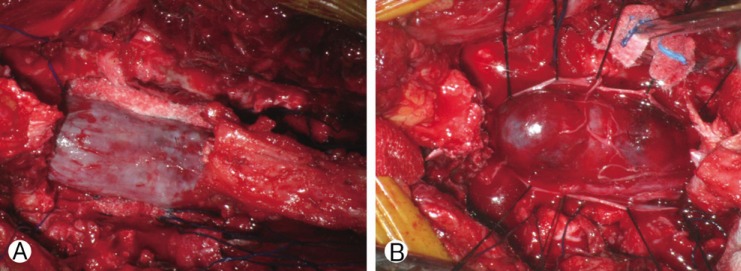
A 76-year-old female visited our department with complaints of low back pain and radiating pain in both the lower extremities for more than two months. She had no specific disease history, except for hypertension. The neurologic examination revealed no motor or sensory changes or pathologic reflexes. Magnetic resonance (MR) imaging revealed a lobulated sausage-like intradural mass (Fig. 1). She underwent a total laminectomy and near-total tumor removal. During the operation, the dura was firm, tense, and slightly bulging (Fig. 2A). After opening the dura, a reddish, friable, and well-marginated mass was observed (Fig. 2B). We removed the mass near-totally except for the lesion that was adherent to the cauda equina. The lower back pain and radiating pain in both the lower extremities were diminished. A histopathological examination confirmed that it was a paraganglioma (Fig. 3). Radiation therapy was recommended due to the incomplete resection, but the patient refused. Thus, we did not provide any additional treatment involving chemotherapy and radiotherapy. She was discharged with no neurologic deficits.
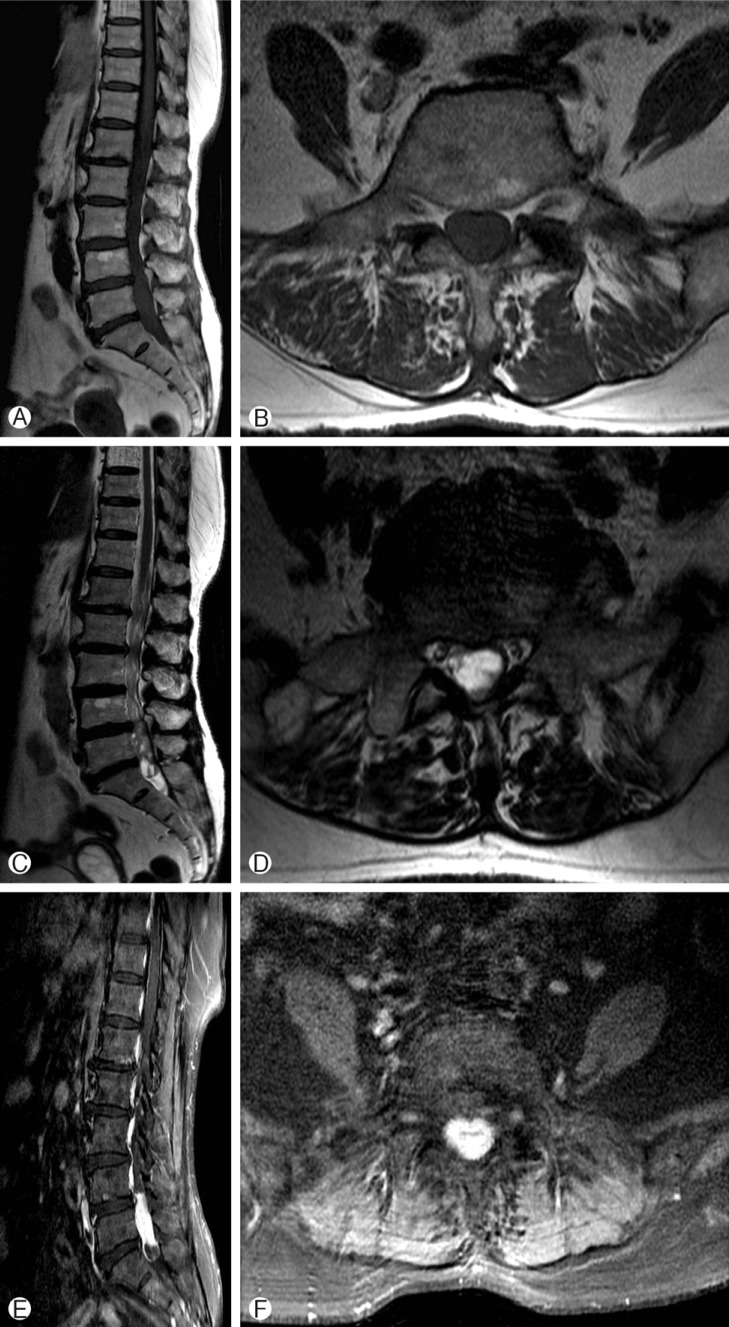
Preoperative magnetic resonance (MR) imaging shows a low intensity mass on a T1 weighted image (WI; A, B) and a high intensity mass on a T2 WI (C, D). After gadolinium enhancement, a well-enhanced mass is noted (E, F).
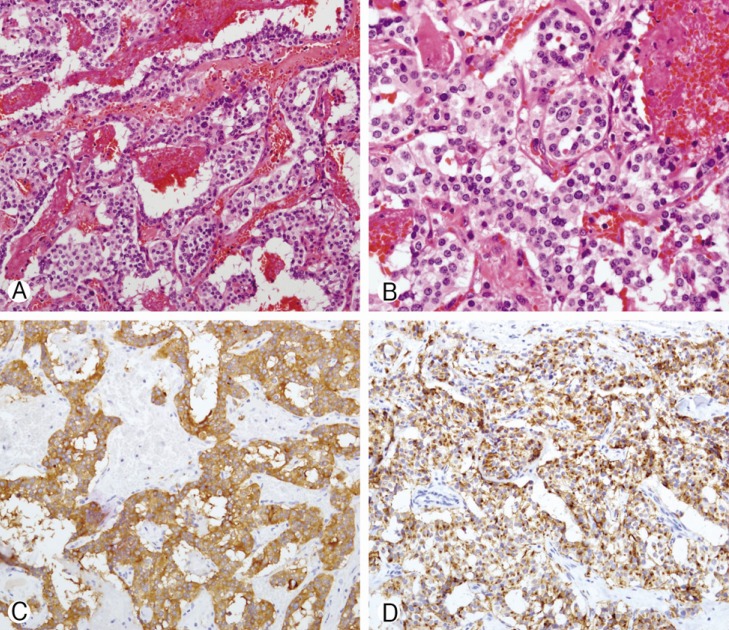
(A) Histologically, the tumor cells are disposed in nests of lobules (Zellballen), which are surrounded by a delicate capillary network (Hematoxylin and Eosin stain, ×200). (B) The tumor cells have central round to oval nuclei; and cytoplasm is usually eosinophilic and finely granular (Hematoxylin and Eosin stain, ×400). Immunohistochemistry reveals that the tumor cells show immunoreactivity for synaptophysin (C) and chromogranin A (D).
DISCUSSION
Paragangliomas are uncommon, benign, and well-circumscribed vascular tumors. Spinal paragangliomas commonly occur around the cauda equina. Back pain and radiating pain to the lower extremities are common symptoms. Extradural paragangliomas may compress the spinal cord, resulting in paraparesis5).
From a pathologic point of view, paragangliomas are similar to parasympathetic tumors. However, functional paragangliomas are rare6). Histopathologically they are similar to parasympathetic tumors that occur in the carotid body or glomus region. Althogh they are also similar to catecholamine-secreting tumors, symptoms of flushing, tachycardia, or hypertension are rare. However, a case in which hypertension was controlled after thoracic paraganglioma removal has been reported12).
Preoperative diagnosis is difficult with radiological tools. MR images of paragangliomas in the cauda equina region are non-specific and are relatively isointense on T1-weighted images and hyperintense on T2-weighted images. Cystic components may be found within the tumor3).
Differential diagnosis between paragangliomas and ependymomas is difficult. Routine staining is similar in paragangliomas and ependymomas2). Neuronal markers, such as synaptophysin, are helpful. Immunohistochemically, neuron-specific enolase, synaptophysin, and chromogranin staining are positive2).
In the cauda equina region, it is very difficult to distinguish paragangliomas from ependymomas. Cauda equina paragangliomas are classified as grade I on the World Health Organization (WHO) classification. However, ependymomas are classified as WHO grade II-III. Thus, paraganglioma-ependymoma differentiation is very important8,9).
Complete surgical resection is the treatment of choice. After total removal, the prognosis is relatively good. Locations in the cauda equina are exceptional1). Recurrence after surgery on a paraganglioma in the cauda equina region, especially if it is encapsulated, is rarely encountered2). The surgical goal is complete total resection with preservation of the surrounding nerve roots1). Our case involved an encapsulated paraganglioma. Thus, we did not treat the patient any additional therapy, and conducted a close follow-up.
Radiation therapy is recommended in cases of incomplete removal or recurrence. However, the effects of radiation therapy are controversial9,10). After incomplete surgical resection, prolonged postoperative observations are mandatory because of the slow evolution of paragangliomas4).
Distant metastases very rarely occur5), and metastatic paragangliomas of the spine have been reported7,11).
CONCLUSION
We describe a case involving a spinal paraganglioma that was adherent to cauda equina. A histopathological examination confirmed the diagnosis. Total resection was difficult in this case due to adhesion to the cauda equina, and close follow-up may therefore be needed.